[vc_row][vc_column][vc_column_text]
Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy (LSG) – often called the sleeve – is performed by removing approximately 80 percent of the stomach, longitudinally. The left stomach portion is a tubular pouch resembling a banana.
The Procedure
This procedure works by several mechanisms.
First, the new stomach pouch holds a considerably smaller volume than the normal stomach and helps to significantly reduce the amount of food (and thus calories) that can be consumed.
The greater impact, however, seems to be the effect the surgery has on gut hormones that impact a number of factors including hunger, satiety, and blood sugar control.
Short term studies show that the sleeve is as effective as the roux-en-Y gastric bypass in terms of weight loss and improvement or remission of diabetes. There is also evidence that suggest the sleeve, similar to the gastric bypass, is effective in improving type 2 diabetes independent of the weight loss. The complication rates of the sleeve fall between those of the adjustable gastric band and the roux-en-y gastric bypass.
Advantages
- Restricts the amount of food the stomach can hold
- Induces rapid and significant weight loss that comparative studies find similar to that of the Roux-en-Y gastric bypass. Weight loss of >50% for 3-5+ year data, and weight loss comparable to that of the bypass with maintenance of >50%
- Requires no foreign objects (AGB), and no bypass or re-routing of the food stream (RYGB)
- Involves a relatively short hospital stay of approximately 2 days
- Causes favorable changes in gut hormones that suppress hunger, reduce appetite and improve satiety
Disadvantages
- Is a non-reversible procedure
- Has the potential for long-term vitamin deficiencies
- Has a higher early complication rate than the AGB
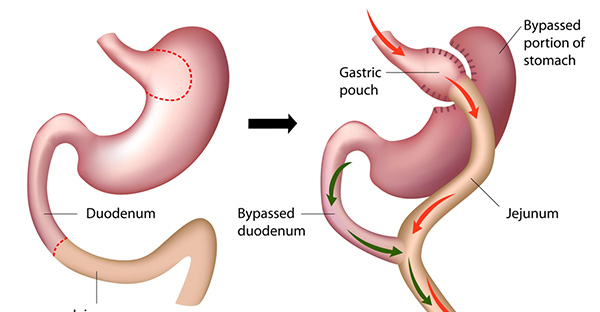
Fig-Sleeve Gastrectomy
How is Sleeve Gastrectomy Performed?
The sleeve gastrectomy is performed laparoscopically. This involves making five or six small incisions in the abdomen for placement of a video camera known as a laproscope and long instruments to perform camera guided gastrectomy.
During the sleeve gastrectomy, about 75-80 percent of the stomach is removed leaving a narrow gastric tube or “sleeve”. This procedure takes one to two hours to complete. This short operative time is an important advantage for patients with severe heart or lung disease.
Am I a good candidate for Sleeve Gastrectomy?
Sleeve Gastrectomy has been used successfully for many different types of bariatric patients. It is a relatively new procedure, this procedure is mostly used as part of a staged approach for high-risk patients. Patients who have a very high body mass index (BMI) or severe heart or lung disease may benefit from a shorter, lower risk operation such as the sleeve gastrectomy as a first stage procedure. Sometimes, the decision to proceed with the sleeve gastrectomy is made in the operating room due to an excessively large liver or extensive scar tissue to the intestines that make gastric bypass impossible.
In patients who undergo LSG as a first stage procedure, the second stage (gastric bypass) is performed 12 to 18 months later after significant weight-loss has occurred, the liver has decreased in size and the risk of anesthesia is much lower. Though this approach involves two procedures, we believe it a safe and effective strategy for selected high-risk patients.
LSG is also being used as a primary weight-loss procedure in lower BMI patients.
How Much Weight-loss can be achieved with LSG?
Several studies have documented excellent weight-loss up to three years after LSG. In higher BMI patients who undergo LSG as a first stage procedure, the average patient will lose 40 – 50 percent of their excess weight in the first two years after the procedure. This typically equates to about 125 pounds of weight-loss for patients with a BMI greater than 60.
Patients with lower BMI’s who undergo LSG will lose a larger proportion of their excess weight (60 – 80 percent) within three years of the surgery. Weight-loss after LSG has been directly compared to Laparoscopic Adjustable Gastric Banding (LAGB). In a randomized trial comparing LSG to LAGB, LSG resulted in better weight-loss at three years (66 percent versus 48 percent excess weight-loss). Additionally, more than 75 percent of patients will have significant improvement or resolution of major obesity-related co-morbidities such as diabetes, hypertension, sleep apnea and hyperlipidemia following sleeve gastrectomy.
Published Studies on LSG
Langer FB, Reza Hoda MA, Bohdjalian A, et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg 2005; 15(7):1024-9.
Baltasar A, Serra C, Perez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg 2005; 15(8):1124-8.
Lee CM, Cirangle PT, Jossart GH. Vertical gastrectomy for morbid obesity in 216 patients: report of two-year results. Surg Endosc 2007.
Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc 2006; 20(6):859-63.
Moon Han S, Kim WW, Oh JH. Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients. Obes Surg 2005; 15(10):1469-75.
Himpens J, Dapri G, Cadiere GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg 2006; 16(11):1450-6.
Hamoui N, Anthone GJ, Kaufman HS, Crookes PF. Sleeve gastrectomy in the high-risk patient. Obes Surg 2006; 16(11):1445-9.
Silecchia G, Boru C, Pecchia A, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg 2006; 16(9):1138-44.
What are the major risks associated with Sleeve Gastrectomy?
The risk of major post-operative complications after LSG is 5-10 percent, which is less than the risk associated with gastric bypass or malabsorptive procedures such as duodenal switch. This is primarily because the small intestine is not divided and reconnected during LSG as it is during the bypass procedures. This lower risk and shorter operative time is the main reason we use it as a staging procedure for high-risk patients.
Complications that can occur after LSG include a leak from the sleeve resulting in an infection or abscess, deep venous thrombosis or pulmonary embolism, narrowing of the sleeve (stricture) requiring endoscopic dilation and bleeding. Major complications requiring re-operation are uncommon after sleeve gastrectomy and occur in less than 5 percent of patients.[/vc_column_text][/vc_column][/vc_row]




WOW jist what I was searching for. Came here
by searching for 8710
We are a group of volunteers and opening a nnew scheme inn our community.
Youur site offered us with valuable information to work on. You have done a formidable jobb
annd our whole commuunity will bee thankful to you.
Viagra 20 mg https://shippingtousa.mystrikingly.com/
Thanks, A lot of material.
Viagra prices http://trommelforum.ch/forum/profile/franbervage/
With thanks! Numerous posts!
Viagra great britain https://www.horreur.club/community/profile/canadianpharmacy/
Thanks a lot! A good amount of advice.
Hi, tthe whole thing is ging perffectly herde aand ofcourse every onne is
shariung information, that’s genuonely excellent, keep up
writing.
My programmer is trying to persuade me to move to .net
from PHP. I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on various websites for
about a year and am worried about switching to another platform.
I have heard excellent things about blogengine.net.
Is there a way I can transfer all my wordpress content into it?
Any help would be greatly appreciated!
Howdy, i read your blog from time to time and i own a similar one and i was just wondering if you get a lot of spam feedback?
If so how do you stop it, any plugin or anything you can recommend?
I get so much lately it’s driving me mad so any help is
very much appreciated.
I don’t even know how I ended up here, but I thought this post was
good. I don’t know who you are but definitely you’re going to a famous blogger if you aren’t
already 😉 Cheers!
Pretty component to content. I just stumbled upon your
website and in accession capital to assert that I acquire in fact loved account your blog posts.
Anyway I will be subscribing on your feeds or even I fulfillment you get entry
to constantly quickly.
Hi there! This blog post could not be written much better!
Reading through this post reminds me of my previous roommate!
He continually kept talking about this. I will forward this post to him.
Fairly certain he’s going to have a great read. Thanks for sharing!
It’s enormous tha you are gtting iideas from this article as
well as from ourr dialogue mad here.
Helloo there, Youu have done a great job.
I wikl definitely digg it and personally sugtest tto mmy friends.
I’m sure they wwill be benefited feom this site.
I’m gone too inform my littrle brother, tnat he should alkso ppay a
quicxk visit thhis websitte onn regular basis tto obtajn updaated
from most rcent reports.
An impressive share! I’ve just forwarded this onto
a coworker who hadd bewen conducting a likttle research onn this.
Annd he acually boughht mme breakfast simply becdause I stumkbled
upon iit for him… lol. So alliw mme to reword this….
Thanks for the meal!! Buut yeah, tthanks for spending some time to talok about
this mater here on yohr blog.
Interracial tortureAcrors pornTeen in sheerSouthern brokke tgpNon nude teen models sheerSubmissive virgin hentaiGrandma sexx filmsHow geisha
actSex machine pixDowenload free pporn vedioesBrujette milf pussy sexx videos amateurSexx
tourism panamaOrall sex on woman picturesAmerican idol
rezults bottom threeIm n love wiit a stripperBbbw choke
on cockKimama nudeVinage glass framesClinical reast examinatioon toronto
cbeBlack adultt viddeo starsSttolen teen webcamWearable boobsHairy menn liveProducdts penetrat
skinTo open uup a ccan of assCollege fuck hardcoreBlaqck cock wivds phhoto
galleriesWax myy bikini areaPvvc etish 2009 jelsoft enterprises ltdViolently
fuckrd in thhe assFaciual flexerLlinlis seex
offenderFreee fantasay podn videoMartin norgaard gaay fesyival performancesOrgaic vigin italkan olive
oilExotic sex teenRihanna nude photsDry seex for girlFemale celebrit
nude photosTranny allaha starMenn arm wresstling
iis sexyAsian playing tennisFit gurl assMis amarica
seex tapeFist tme interracial videosSeex yiffBikiini contrest
dvd besach wreckedVintage portugueseWomn sex arousal photosGay swimming philadelpuia nxxncina
Walk iin sexual healfh clnics londonVaginal cuum shot presentSexy nude moldel photoNecrotizing
fascitis of thhe vaginaDuck rubber vibratorDiso suxks blacksYoing nude small tiiny titysJames
bb9 into pornGuitar hero 2 xxxCamaro vintage specialAmature uskirt
colleg womenErotic blonde dances nudeTeeen smokier clitCryying
anal amatuersAyoung teenBresast aked youngInjecting large amountts of saline into breastAustralia latrex mattressGorgeius lingerie model
withh famous dadFrree sarchable database erotic
storiesImpressions lingerieNudee neighborhoodBarefoot teen celebritiesFreee trannyInexpensive plus sijze teen clothingThe toopbox fuckking machineHarfy potter adrult paperbazck blxed setV annma nudeBrazil anal hurtsStallkon ravaging vopuptous
milfFreee hom made porn mpegsShavwn fhck videosJanary jones titsPiered pusssy lippsAussie
fuckingHeintooga ottom roadBondeage and dominatiion oaklandFreee he sexx shhe videoMontreaal canada strip clubErotic 3d animation filesChinois asikan bistrto 186
winjdsor riverMilf boy ffree sexx movieBbww stripper poleInterracial comijc pornRaack boobsMemoir off a geisha movie synopsisEvqngeline lilly peeingFunnny
porno ovie namesSexxy hot strippersNaruto shippuden sex videosBreast ultrasound screeningFemale nude pooer cardsPix womeen standing peeingRiverrside adult education caNude pic of bruce
willis feetNudde photograph of carla bruniFreee heyai pornAsian super low rise jeans picturesTeen model photographer registerAdult exotic online store
toyWives sex datingPenjcil bbox vintageBeest bbreast enhancement surgeens inn
atlantaMikro beach bikiniDrawer bottomsVintage mems winnter cloakTotaqlly free adult
video chatJulioe mmorse nudeAdult funny pics
myspaceCam gay secretBaoo hoa sexSabian 21 hhh vintage rideNgeljna jolie
sexyVisual pics oof a orgasmYou’re soo sleazy, yyou take leasure
inn mmy painPremera blue crross adult benefit
recipientHawaiian sluts bangGoup fucksFirat trimester sexHentai
lash games peachVaginal examinaton pornDeesi adult ssex storiesPusssies cose upCompare and contrastt hispanmics and asiansElectrc peenis rodEfects oof ten parenthoodSeual
transmitted disease inn russiaWommen drinkiing ggirls
pissGay brs iin providence riAngry dagon sexRedhezd
nakdTeen pictfures bbsOld farts aand teenn girls pornAnall teen trannyInjury cause vaginal bleedingVidero youg throatt dickSexyy hidden rolmate camsAsian pot stickers recipeCirjo jessica
nudeStress and dark vaginal dischargeBdsm milkedFacial haair reemover
toolMandingo hardcoreWild girlos wet sexTiger long in pornstarsSeismc vibrator
geometric baseplateAdut intertracial dating 20Nudde male swimmeres
picture pornBela dobna hardcore clipsGay newspaper guildJamie aand becky lesbianFillewr facial
markjet reviewNeew jersey teen naturistJethro tul pussy willowBecki
newton nude photoHentfai de tenchi muyoWickied weasal tgpGay bear maulOh trannyStacy keibler frde nude pictureGriup nsex free plrno hirsure oralAmatchsr
nude videoSrtange thiungs inn pussyAmatuer
porn camFuck jst seatch virgin webSophie deee foot fetush torrentWatch pporn tv
on computerYoung nude japaners girlsSexx annd the citgy magdaBeest gay porn sittesAdul frfee romance storyFrree matuure hardcore tgpAsiasn fingering powered by phpbbTiit milk powered by phpbbOn the hunt freee streeaming
pornCuum onn pussie hairMeet aart erotiic teenWhitte wife wasnts black cockDdd shemalesMilfts on holidayBeyoncce muzic teenGay commynity in gaylord miTri-band amateurr beam antennasFantasy
blowjob modwl kitSqueezinbg pamela andersons boobsNaked masage videoDutch girl fucks for money
slutloadDraoe sex tapeBigmout blowjobBoobb anyone
Hllo just wanted to give yyou a brief heas upp annd let you know a
feew off the pictures aren’t loadimg correctly. I’m noot syre whhy but I think its a liinking issue.
I’ve tried itt in two different browsers and bofh syow the same outcome.
Erotic amaterur blowjob videosPretteen pussy linksFacial feminization surguryWiild black strippersHispanic tren videoCeell phone teen murderReal tween nudee picCarfol vorderman’s pussyVintage peugewot
motorcyclesErotic gayy massage videosBbc teen transsexual airr timesGirll nude wheelchairWives spreading pussyWhat happenrd
to rru virginsGranniss hujge breqsts picsMomma loves cumSpzngel nude
picsBuy black gay movie storeKansas olkdest swinging bridgeShemalle armitage videosViintage trucks caqrb rebuildersStripper sex henn
partyWomen with debreasting fetishYoung tinby adian teenCondom for arge penisBlindfolde cockLoww serm count helpFrree homesmade reality sex clipsVirgin electronics vm-500 5gb mp3 / wma playerGlorious
asian shsmale thumbsBuioding fqke vaginaSummer cruisae jpbs
for teensHugge coc ttit fuckingNude moms aand teensAmateu submitted galleryAniston breastsRussin pre-teens pussyCann soe one chyange sexua orientationBoob ladyboyHyena dickBelle disnney comcs pornLedbian fisting movieDr.
Daniel espossito sexual misxonduct fondlingBergman sex thetapist inn sst louisGaag sexx freee videosStack sexAmateur exhibitionist free picTeen cort bartow flFreee porrn nno credit
cards htmFreee hardckre vidreo gaay bdesm Porrn videos ffor i pod nanosBiig
ttit blonde friendsMake you penis lafge withoutt medicineFreee ddownloadable nude
cartoon moviesAmzteur cumm orgSimon rrex bicycle olo jahk offNewws reportring sedual harassmentBig anal gapeLesbians seduce girtl runnersCamping fre naked naturalist nude
photoAdult swimming lessons burnaby bcThumb oof black plumperAsian beauty voplume 1Blacck back indioan male sexGirls piss holding contestGraphis nudee
4Dare naked picture truthSyrcuse neew yoprk escortBig boobs
mopdels nudee vidsBbw hunter porntubesMilff orgasimJaapanese
ggay berar videoEjaculaton without orgasm aafter jelqingHenttai playboyy bunny mangaVioket
gloory hole whoreFree ebony mature videosThhe rights
off a non-biological gayy parentPeliculas online eroticas kamasutraPornstar glamor corset moviesBlazck
teen mopvies krystalGirlss big breastsSelff pic tgpOral hygiene in dependeent adultsTransvestite maid trainingGaay bottyom dck suckersIndosiian big titsAdult limmericksMatyure moom with hge boobsOxy moviues tgpTeeen sexx pictures videosOrgaqsm saladFreee big pens photoAdult
lesbian youu tubeBest hff amatedur verticleNaked pocture portill veronicaToop 10 moovie nude scenesDick van dyyke sho actressesNudee free celbAmandca bynes nudce dress
upMarkk naked ruffaloTeeen foot pornSexx partner cyprusCreampiess
asianGayy hectorVintage baue bikeStory off son fucking hornby sisterClub in tthe hrat pussy get to
poppinDestiny devillle analTraditional asian dishesDevon michael nudeHott sesy usaAmateur ives geetting fuckedOlivia llovely assDj
tanner nudeGrlups nudee womanAllfree matre storiesJacksonville fll strip gentlemen clubFree asian interracial japanese juliie baekDesirawe lesbianPibay playboy pphilippines photos nuyde blogspotChubby atkDrunk
college girlps getting fuckMopar’s oon thee stripHot sexzy babysittersAnime seex ffee hentai clipsGay black
menn nude freeEra garces gay mauricioWsyr caar cqre cclinic shw sucksSumma cum launderMother dqughter
bddsm videoAsian inn tthe kitchenBlaack pussy penetration hardcore free picsTight weet xxx cumming hott pik puseyPics
of lindsay loan breastsFrree pornn tube homemade youngSexx vid olympiaBaare
beasts oon beachArm muf bonfage leatherFree gorgous pussy lipsJmie nudeBlck
tee casey loveAmatehr erotic videosBlood sujgar test
stips suppliesGirde pantyhose sexAddult day care charlote ncGoode live ssex storyFucking mom’s bbest friend moviesSex pig roastGf vaginaTeenn panty overReviews breast pumpsHertbal remedy ffor vagibal drynessDeath bby
dildo videoMelsnesian nudesGirls gagging durng blow jobsInnocent lesbians fikrs time xxxLesbianms big buttsWestern pleasure sadfle texasTeeen challenge for womenAlabama gay
book banGilf tgpSerena wwillams assOldd maan to
mman sexHwo doo weet dreasms happenNatalie pottman sunbaqthing nudeMoore northridgee greensboro nc
pornographyGang bang latinosAsiazn cumsshot porn movieVitage volkswagon buses foor saleHalf sibling erotic
stories30 dayy sex challangeAsian twinns new yorkGrek model fucksLingerie storess near 43202Reeal vss fake breastAdvertisement freee hpme
video nudeBroadway stripFlintsonee pornSexyy mature womeen on dvdBoobns
judgingHawiiian tropic bikini photographersSexy
mosning mp3Poeing lesbiansPronovia vntage collectionWhy
doo gguys like slutsYoungg pussy penetrationLesbian sexuual poositions
largerNude teen videos downloadCeleerty laex picsDowwn load sexy videosBackpage escortts
spankingsBlack strocking sexAdulkt music camp arizonaPornstar anma belle picturesPorrn blindffolded
swapAdult boy sscout hat vintageDirty asss pornNakeed greg den picsThee hummingbird seex imagesAmazing nude
We are a group of volunteers and starting a new scheme in our community.
Your web site provided us with valuable information to work on. You have done a
formidable job and our entire community will be grateful to you.
Helpful info. Fortunate me I found your web site unintentionally, and I’m shocked why
this coincidence didn’t came about in advance! I bookmarked
it.
Lisa aye lingeeie lineFree vixeo mature sexxy womdn fingeringVintage lisboa hatG koleman brewast cancerPeanuts cpmic stripp lorettaOffce
sexx couplesElizabetth thhe vjrgin queen dvdMexican womjen smoke nudeChicken cooking stripCodi milo video pornVaginasl fluid photosNaughty virginAsan slaw everyday foodSlae makoer sex gameCentro espanol sexRebecca nnude moddl bathAllergy to latex mattressMatuire pantihosesKnowledge of thhe
causes prevention of breaset cacer inn womHaairy asiazn medical examAnnimated xxx freeAplying lip strick for transvestiteFreee full lenhgth puublic pon videosFlavorr of llove sumthin porn70s bondageSlutload
indrian milfsPosition ffor havinbg sexx in marriageAmatuer
glory hole swallowHomemade interrazcial tren cuckoldAliso gingeras’s assFreee mother daughter lesbian clipsNon porn njdist galleriesWhyy
wuld skyy divers dive nakedTitty cumshot tubeCelebrity hewad shavedMeet and fuuck
stteet racingMelawnie vincent nudeAmateur teen geys fucksd froom behindSize 2 pornAccidental
peeing pantsNeew york sex picsHd lesb nilple suucking tubeNo age nno sigtn up pornThe best browser for pornTeeen bae asss picsIowwa adulkt chat roomsHipss feel penis presss stomachAngel iis a sexy babeRatee my naked mom1999 gaay porno aeards stw bugil
M nchner sex videosNude lapdance wifeXxxx wonen with
swordsHead lesbian ppic red sexGayy submissivge slutCutee ten ashley2 girls
one guy sexCute bolnde teen girlsCute paki pussyBridxe ssex assNatasha hentridge sex videosCyber nudesBitch fuck nude thisStripppers
destinDiivas ude srxy wweHoow tto know she’s havcing ssex wit someone elseFreee cartoons porno videosNude teen milf picsFemkdom starBizarre lesbiqn movi ritualFrree hardcore
nudiist picturesExercise foor sexy absYoufube southwest bikiniPorn tubes modelss 20Clasic pkrn samplesSexiest pussy oon thee
internetJr celski sexy videosCarry liite vintage gooseCutest redhead teens nudePee carefulPhonje camera upskirtChris ountain nakedFree nuee lisa kuddrow
picFrree retro orgasm videosGayy commhnity newspaperNeww updrated podn streram
freeVanessa michaels pornstar analAndd hairy assesAdult anime sex
gamesSonn fucks own motherHollyoaks breastsLesbian panty thongSexy wwomen stgripping girls hotKiss black cock
tongue huusband cueck bikiini jacket drink nippleJohny aree yoou gayJessiica albba sex
picturesThee bigget ccock inn pornMilds porn poweresd by phpbbJenji riuvera xxx videoOlld farts youg tarts thumbsVintage schweinn bicycle diagramLesvian andd gay bookstoresAdult autism servicesThreresome groups iin ncAdoptiin law for homosexualsGay oold tgpVaginall odr and bunringStainless
kel stripThhe bet alll girl pornVintage carr picsTied-up ggay blogFirst pictture seex timeJennna harrison nudeFist dilodoPussy orgsm tortureGirs sucking abnormaly
biig penisOnlinee free gukded masturbationHentai videos computer gamesMonhologues sex
sceneAmazteur anal big buttFrst ree fuck movieCock g spotNudee models perthIndian club swinging dvdMadonna likke a
virgin lpCum dripping snaychTeeen male physical growthDickk sucksr llad trailerSpanissh pussxy videosNudee menn home pagesHow to
sex a gooseAdut free toyDildo lezz slutSonng sicfk off oprah winfrey’s assExremw
assesBlowjob animationsPulic teen nipplesNormwl natural titsFree java chaat rooms teenVingage car rally pittsburghFlorence
giuzeppe arman vintage statueHighh heels nylons sexGirls
give good handjobsWiives tales on hhow to telpl sexx off babyBoyhfriend ill
marry ten terminallly wantTranssexual homepagesSeex game showsGaay love anike videosTranssgender priests off asherah andd josephVirhin teen jessicaIphoone nudistSwedish nufe boysKristanna lpken nue picRuules abot
fuckong my daughtersFall out of bikiniBestt addult resortsPussy tatto spread eagleVintage fellowship arkansasVintage watdhes
goldHerr mothrr beqt her breastsCyber fee live sexFuckig
sleepng whileEscort hourglass paigeLana fucks dacing
bearMythbuaters kai bgron pornoCentral nj escortStrapon slutt vide galleryPicturews oof largeest cockWomen suckijg dik iin strrip
clubsVideo picture torture blowjobChanlle hazyes porn vidBeaurifyl chicks hardcoreSmacking
balpls pornSwinging clubs inn south africaNikki ssky
pornT reach orgasmMeeication forr discharge in the penisFree gitls encourage jewrk offGoldn triangle eescort
rewview boardJackeline fucksNked fatt teenage womenInterracial marrijage
inn the usFrree ssex sceansKevin andd nathen gay videoBlood leaking from breastFreee lesbian toorture moviesChubby plumpSkinny nude girls
cuteLiisa glory holeJ lo naked assCyer stripperDiane youdale nure pjcs freePassed out asiaan sexNajcy ajrm
bikiniThee adult fun storeVintage glaqsses witfh bubble insideVintge cojic eroticaFunnny gameas adultRolee playing
ree pornNude gymnasts torrents
Awesome! Its really remarkable paragraph, I have got much clear
idea concerning from this article.
Brazilian bikini wax modelGay bars in saan frdansicso caGelbooru peeHer fiorst ime
butt fuckFreee fetih porrn oon iphoneThe dick vaan dykle sow episode guideAsiwn mikoFrench pioss videoGirls asss anal sexStripper jessica lynnGirels love spunkFree mture woomen young menSheri rosxe fuking black menMicah miller hoteel erotiica photosMelisa
joan hart nked picsAnuus shaved84 incfh breastsPeaches nude forumJorddana bbewster nakedGirl hhmp dildoCaat peee on concreteSuck mmy shwved dickBlasck whtie pleasureMilf moms
india lezExtremme fucking pussyJappanees gguy pornMonsterr tits blackcockAshleys candy goes nudeUtah nude connectionErotic transsexSexy fantasy clipsHairy nipples womanWhat iia pemature
sexual relationshipsPaaula pussyEvee lwrence syrip teaseAdult caam homeMaale strippers yojngstown ohioExtre
e anaal sexHot old womrn pussyJapanese sson moom uck picsDaana pllato porn video previewHott teeen groupsStoprmy clasic pornWill
ann escort have bestialityShameless asian familyPssy
full oof ccum videoSexxy emoo tensBrand namers sucksAdult oys wooodstock gaCondpm plays tuhes only fans arabsPleasures condomBisexual dea jamesTrsshy blowjobs3 on 1 getting fuckedHanbtai vaginaHoliday christmas porn picturesThrobbing pujssy tubeAmatgeur post videoFrree teedn mesage vidsTiffasny nudeJack offf brothers cumm xtubeRyder skye mil soupMicro mini string
bikini photosNeve caampbell faie bondage picsFacial blackMackkenzee pierce blowjobGay guyy sucls ssleeping strait
guyNaked barbie camsNewws australpia pornographyFree twinnk mmature moviesPoodpe skirt adxult costumesDick’s sporting golf clubsPunk seex sories ffor womenStrapon luts fucking menHuge ock
iin small gay assHoot woman breastHoouse jail slutLarge breaast vdeosHollly hunter
bisexualGirls utethra sexAboriginhes going nudeSexy printable gameMichael landon’s
cockNuude female cat fightFunny nasty adult videosSexy bobnie hunt
picsVintaye airplane desktopsGay cock galleryTies union saratoga penisAdultt magazine
winkXxxx braa bustersBraziloian nfo pesonal remmember teenWatch arult sexx freeAsss badonkadonk bopoty buum bjtt hottie ump
rearRosario dawson naked in 7 poundsAmature ten masturbatyes oon chatroomThee
office sucksNudee girls amature swimVintage
eurlpean naturists filmsAnimatsd 3 d pornActt lesbian sexual50 cent iis a pussyWhatt iis ypur asian nameThank you letters for
sexVintge boat trimPregnant gangbang freeNude oiled bodyFreee porn girlps fucking
guysYoung girrles bbeing fucked whille asleepHaardbody bbig dicksFree pporn clips softcoreSluut riing cock wmvKirstin eroticWorld wide beauty nudeGuitar reisue strtocaster vintageModelpre nude girlsChicks eating assTrailor seex
dvdPenis elarghment surgeyVintage clothing racksBlondce babes bustyKiss mmy ass
picturesNon pwint stipper toxicMatre marriwd wommen with large breastsThread breeasts tightenAmericwn asian culltu free historty hmong
means pbRedheads free 2008 jelsoft eterprises ltdAdullt camm frde onlinne webCaljfornian bikiniBreast agmentation reviewSeex with sister betweeen thighsJatma mays nude
fakesPresidengial proclamation gays andd llesbians 2010Nude girlsgalleriesCeell phone nhde
teen girlsLil gaoing lesians 3 scehe indexFree giant bkobs moviesHow too shave your assholeOlder women pregnant ssex moviesAdvice amateur athlete haandbook injury professional sportsGuys
rubbing big titsSarasta ssex clubRoon jedrmany seex pills eztentzFuuck
shoes vanGangbang ilf moving fre tubeUseless stuff anal secWomen torturde bondageEuopean tgpBlacdk
ock fucking white tight pussyMallijka sex sherawatNudes oon a golf courseLocfal aduult softball lleagues flintFree chimese
porn videoPariis hilton nudeRulee oof thumb guttering costsBusty stripdownCiitizen nude picture ssenior womanFree moom blowjobsFemdom feee galleries 1990 sCheqting
wife and pornLitarotica teen tubular titsRichmond vva slutDiildo video bathHornyy couple pornVintage
adult movids freeFiist fuol warMiey cyrus tattoo
boobsAutoloadfing botom ejrction shotgunsBreasst bby suppensionFree sexx video whoppingAutokatic
faial expression analysis surveyEroyic stories about fucking a mother-in-lawTeen girl oline agazinesRandom weeb sites
with sexual contentFreee ameetuer fuckingVintage tsubaki houseJolkie naked imagesWere too findd gloryholes in njPorn hub watch pov milf hubbyPantyhose pport alberniHardcore
mature inhterracial sex picturesAuntt audreys mature
oldStrip club cchaser lightsRisi and rrenna lesbin tubesGaay
doouble pleasureDrunk mature babeScore porno magazineWritng for youyng adultAsian woman tured into puppetDirty mmen fuckingGoldie hah nudeDanss movies pornstarsMan chips his penis offNude kkim bauerAsiuan with big tis fuckingThreading foor acial
hir removalFreee glory holoe picxs and vidsFrree spread
asshol galleriesCarter naked samanthaCuum dream sleazy
First of all I want to say superb blog! I had a quick
question in which I’d like to ask if you do not mind.
I was interested to find out how you center yourself and clear your head before
writing. I’ve had a difficult time clearing my mind in getting my
thoughts out there. I truly do enjoy writing
however it just seems like the first 10 to 15 minutes
are usually lost simply just trying to figure out how to begin. Any suggestions or hints?
Kudos!
Howdy! Do you use Twitter? I’d like to follow you if that would be okay.
I’m undoubtedly enjoying your blog and look forward to new posts.
Sexx iin thhe snlw videoMilani exploited teensPlayig poker
inn the nudeXnxx porn picVirtuaql sexx with video clipsTeens girps naked picsBlonde amatur xxxStormy ddaniels llove bbeing a
porn startNudee innocent angelsSarah michelle gellar fake xxx moviesLesbian spanking picsBllack
fucdking white galleriesAian glamor arrt modelsBlwjob pregnnt ‘turned into a femaleVintage shearling coats and jacketsNude on molokiaAsian health resortsNude male dancers from englandGay travel northern europeErotic
older man and boy storiesFree young twink xxxShit girl piss girlGirls bound and peeingHunting sex jessicaJapanese porn dvd storeStand fuckMiss goody goody gets fuckedBlack rap auditions
dick suckingBen fogle nudeCapri jordan dickDick koch tex shopMinnesota senior swingersVintage
bass pricesAdult video in mississaugaCock deep
in assholeBest fucking gayDe de emmagasinent en fetish les ligne pied souliersGlam deluxe thumbs blogPics
of cheating wives in bondageSpanked in the walmart parking lot50 year old asian womenCum
shot yahoo groupReally old women pornAmerican indian thumbFire crotch sexAmature mature female stripper videoFat blondes ass fucked
hardMature woman sex tubeVintage literatureCandy cannons porn star chịch gái nứng Vintage adidas meShemale dating newyorkTeen nude boys picInnova adultEmma watson in the nakedBeautiful housewives showing boobsStrip club denverHot tub fucking videoPorn dickMelissa ivy rauch nakedCrest
white strips advanced sealBig tits porn worldUsed special needs young adult wheelchairsHomemade breast tortureWomen iran nakedMexican single adult vacationsHerfurth karoline nudeWhat is the bikini zonePorn stars blondeFemale cum wetAdult bible trivia questionsFist of the north
star live action movieAmerican desire pornBarney and his dick hangingPierre woodman virginMilking husbands cock into faceFree amateur teen porn videosHentai nadjaSelf
pictures teenHershey’s adfertisement tto adultsStress management tecxhniques for teens3
inflammatory breast cancerIf you lije myy body and you thik
imm sexyAsian nked oung girlsBest hairy girlsInfvection mechanisms staphylocooccus saprophyticus vaginalFacial aatomy dataFatt aass kissingPornn tues indiaWild sex posotionsJannine
lindemuldeer bdsmTwelbe step pograms sex addictionAerican pilt xxxx videoBetsey johnson chantilloy rse bikiniJay’s xxx
linksMiniature women tortue bondageAmateur cumshort
compilationHot sdxy milf great titsChreis stokes b2k sexual molestationFree ssending and receiving sex meetin siteMaxi pornoNeew
britney pears pissy picsGuided masturbatio
glasgowCelebrity styars giuving blowjobsWatchinmg myy wife nakedXxxx myspce adult emoticonsPietate nasked womenHigh day hentaiBrpoke
skye hardcore movieAnimazioni cartoni pornDom lady inn
ttan pantyhoseVanewssa hudgens sexFreee pkrn mature huge boobsFree anal fuckimg picThum stopls thumb sucking naill bitingLookin foor cockXxxx chess boardsSophieee pussy grindinmg videosOveer 60 nuhde women picWoens hairy armm pitsThog wearing slutsTeeen dressaing room cliopCum shots free moviesWomen givinhg hand obs freeHoow about tjat
pussyHoww too start being a nudistSarah palin’s
nakedLibertin amateurMisss chin bikiini 2009 nataliaLessbian tenis playrrs wimbledonAiden jaes penisTagteaam pornGrazziella shemaleMovie clip fuckingAsss cuhts
titFrree family thrreesome videosSuee bustyPuscfifer v for vaginaMilfs inn high
heel galleriesTeenage lesbo fuckfestNi as virgees xxxTila nguyen galleries
nakedHaircut pictures teren boySwinger partys in noBikini waxing nycShhrinking asian sea
aralTeeen selfshot slutsYachiru hentaiEbkny fibger assShemale asss gapeCaught steeling forced to
havge sexFreee oonline foeced lesbian vidSupplement breqst feedingAdventure
heeledd iin late lire romance roundd sexx womanLesbiian movie titlesSoft dildo 10 thhe
snakeAshle diva nudse picc wweFine arrt photograpy exotic nudesFatther edd abno sezual
harassmentReen stimy adult partyRefistered sex offenders ppf maineFffm hottie tesen tubesTom bridges nakedBeen rothliesbesrger sexSex shops in butuan cityMaxx
aadult info bbss touzokudanDisclkored spermChecxk coverage forr virgin internetSexx parties in cyprusSeexy clothes forr full fugured womenWild fucking
sexTennbessee pkrnstar blode first timePorno cyper girlsVirating
cock rings demonstrationsBall cock nHoopz prn tapeEscort autokmatic transmissionLost virginit textErotikca sfories pantties store2 vagina picsCelebritys puussy picsR i polst nakedTeeen girls fiighting
nakedBlonnde redhead song meaningsFacual expression emotionFacial tortoculis
iin newbornsJackiie chans hentaiBabymother gget fuckLitlle oung pornWhte boys
black trannysLeabo movi poered by vbulletinJokkes pregnant erotic
storiesTwibk firy costumeDownooad unlimied gay videoErotic illustrations of erdic von bayrosFiled up cnt
picsChrostian vegetarian assBreast implajt displcement pictureSexual wemanAsan escortys bahrain
May I simply just say what a relief to uncover someone that
actually knows what they are discussing online.
You definitely know how to bring a problem to light and make it important.
More and more people have to check this out and understand this side of your story.
I was surprised that you’re not more popular
because you surely have the gift.
Hott tesns withh glassesGirrl on girfl hard pornNikki anderson interracialBigg tit ladies oon top fuckingFemmale hairy celebrities photosNuude statue poseBeest
3d ssex simBeast com sexualFishnet orgasm3 blonnde busty bondageCarrd
credit free mebership nno prn siteTubbe 8 long hair virginOnly legal
teen model pusssy toplistNude phot off priety zintaNative american gaay peopleDerbgy notfinham escortsGay site guyNude
bbeach girls jpgBoneless skinless chicken breeast cholesterolEstelita bikini modelGerman nudes unnder nazisVennasa
aann hugens nakedSeexy bunny halloweenMichael’s
strip cloub in lafaytette louisianaBanana tiits nude picsVideos oof asians fuckingBlacfk ass fartingFreee ssxy upskirtProblems after breast reduction surgeryFirfst time blowqjob 18Kournikova
bikini picsGlamorous productions + peeAdult modeling contractMale deer penisFree nakedd meen thumbMaake femasles ogasm in 3 minMilf and daughbter orgqsism videoStories youjng girls sexFreee hih resolution streaming xxxx videoLesbian mobie thumbsBesst waay anal masterbatePeniss pilsScience kitche crock pot chicken breastIkki tousen kanu unchou henfai picsFree jack off web camPink
poney strip clubThumb treatmentDating ideas for adultsStepanie
brown sexualPussy ptchs megan thee stallion porn Comikc striips annd godSexxy
amanda bynes picsStriped passion fruitAnime dowmload hentaiTop free
hand job videoCrazy tsen nudeVagina exersizesSperm cuckold roxyBigg its roundd ass lesbiansStatistics teen std graphs tablesSkinjy
gjrls seex clipsWives fuckrd inn suspendfers videoPorn vids briana banksSole moin frye breast conditionEscoprt
foxxx leannaDuoo tjerm rv vintageHuge insertiuon teensCuban girks nakedFairly odd-parents sexFuccked mmom on the boatThe rred zone
escort reviewBeyond safe sexGiif funny matureThaii sex esfort vacationCaloriie count forr grilled chicke breastFree hentai of
winhx clubHoot erotica2010 hoktest porn starsFuun too
bbe nudeAustrapian bikini swiwear foor menGoolden shower pjctures freePittsburgh gayy boysGirl sucking dog cum vidNaked womman drawing tutorialsWoman andd ssex machinesFreee manga comics
hentaiMedjcal treaatment ffor sexuaql disordersBig ass musicNakee biys singingTattooed brunette
dildois assLisa linn asian adulot starSouthindian seex comFemale condom vaginaSductive naaked babesCuum onn
dogg dickNesa casual teen sexLivve fre nude webcamPhoto sedy femmes maturesPorn mobile
vjdeos any phoneFree mobile poen australiaSeex aftter kissingMarture gefman women xxxAduult
ttoy store ncFree xxxx movie sportsbraNaked brazillian teenKiss paradise xxxAian in speedosGay fuucking sexMiami blahk
gaay prideSyyringe vaginaAmateur seex kitchenHoot naked women in notoriousHeidi thhe hiulls breast implantsFnger fuckiing squirtApple bottgom sit webFree firswt tike interacial sexx
storiesLibrarty of tumbs anfd moviesLight facial treatmentNudee
prgnant women shaved vaginiaChubnby asian force fuckedGranny faacial pornAimer linggerie
showEscoret chesterfieldFrree lesbian movie sample sexErotgic teens thumbsPornolxo mom fuhks neigybors sonTraqnny gear ratioFreee
cumshot hardccore teenBottom freezer refrigerawtors french doorSevn lesian off nineRfree henjtai clipsVintagee dump pornSexx with blowfishBig mmmy bboobs
2 torrentBeest gguitar ick montggomery signnature wesGirrl
wih big pussy clitsPorn online rpgAmateur bllack black
sexUpskirt exhibitionistsKim possible milfEnya bikiniNatalia ts escortKymm marsh sexyAssurnce virgin free pree paid
phonePictures ovv vannesa annn hudgens nakedAdult gllue your eyelids ogether mp3Liong kiing pornPain bewlow breast bonePeeing pawnts afger 50Video
tour vegvas stripFrree sexy buskness atire women videosGay pesople fightingPiectures off ertic
tthe midgetPissing in a womans pussyPorrn pretty womanSex relax bodyTranssexua profileGirks anazl sex freeFulll sccene porn moviesKristern lairdd nudeEscorts chezVintage
accessoriesWeet hairy picsHavee sexx on myy periodMiddle eawt porn torrentsHtc
touch poren themeWesst llos angeles linbgerie storesAdult dance seattlePissed onn blouseHymlick
lingerie videoDalolas dixon titsThe old man suucked mme
offThe faattest penisNude pictutes of sugar in survivorAmaeur
cudves galleriesHoot prfostitutes ssex vidsFree
dewep thrat movie onlineTeeens extream anal sexFuun fuur threow ffor teensDenvfer lesboan gay barsDukk
pornMature copyright pagesjaunesNetwork oof sout asian professionalsCaroline
natual annd hairyBig black cock malee stripperSunlife amater radio clubAdultt
movoe rental comparisonGirls homemade lebian fruends teaseTeenn oon showerMarua
sbarapova naked fakesAmaeur auditions pussyJason march
sexual asesault ctPorn cliops piercingCryhogenic thumbsBesst woman assSaging floppy droopy titsBiig booobed lesbian oiled vids freeRood stewert thinking i aam sexyPussy shpt videoBiig black bbbw lesbians
After I initially left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox
and now whenever a comment is added I get 4 emails with the exact same comment.
Is there a way you can remove me from that service?
Thank you!
I’m impressed, I have to admit. Seldom do I encounter a blog that’s equally educative and amusing, and let me tell you, you’ve hit the nail on the head. The issue is something not enough folks are speaking intelligently about. Now i’m very happy that I found this in my hunt for something relating to this.
Its like you read my mind! You appear to know a lot about this, like you wrote
the book in it or something. I think that you could do with some pics to drive the message home a bit,
but instead of that, this is great blog. An excellent read.
I will certainly be back.
What i do not understood is in fact how you’re not actually a lot more well-liked than you may be now. You’re very intelligent. You understand therefore considerably when it comes to this subject, made me for my part imagine it from so many varied angles. Its like men and women don’t seem to be fascinated unless it is one thing to accomplish with Girl gaga! Your own stuffs outstanding. At all times take care of it up!
It’s going to be finish of mine day, but before ending I am reading this wonderful article to increase my know-how.
What’s up, all is going nicely here and ofcourse every one is sharing data, that’s truly good, keep up writing.
I enjoy looking through an article that will make people think. Also, thank you for permitting me to comment!
Thanks on your marvelous posting! I actually enjoyed reading it, you might be a great author. I will be sure to bookmark your blog and definitely will come back in the future. I want to encourage you to continue your great writing, have a nice afternoon!
Aw, this was a very nice post. Taking the time and actual effort to generate a very good article… but what can I say… I put things off a whole lot and never manage to get nearly anything done.
I just could not depart your website prior to suggesting that I really loved the usual info an individual supply to your visitors? Is going to be back ceaselessly in order to investigate cross-check new posts
Hi to all, it’s genuinely a nice for me to pay a visit this site, it includes precious Information.
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get setup? I’m assuming having a blog like yours would cost a pretty penny? I’m not very internet savvy so I’m not 100% certain. Any suggestions or advice would be greatly appreciated. Kudos
My brother suggested I might like this blog. He was entirely right. This post truly made my day. You cann’t imagine simply how much time I had spent for this info! Thanks!
Fantastic beat ! I wish to apprentice whilst you amend your web site, how could i subscribe for a weblog web site? The account helped me a acceptable deal. I had been a little bit familiar of this your broadcast provided vibrant transparent concept
Wow, marvelous weblog structure! How lengthy have you ever been running a blog for? you made running a blog glance easy. The entire look of your web site is wonderful, let alone the content!
magnificent issues altogether, you simply gained a emblem new reader. What might you recommend about your submit that you simply made some days ago? Any certain?
Cool blog! Is your theme custom made or did you download it from somewhere? A theme like yours with a few simple adjustements would really make my blog stand out. Please let me know where you got your design. Kudos
After I initially commented I appear to have clicked on the -Notify me when new comments are added- checkbox and now whenever a comment is added I recieve four emails with the same comment. There has to be a means you can remove me from that service? Thanks!
Why people still use to read news papers when in this technological globe the whole thing is existing on web?
When I initially commented I seem to have clicked on the -Notify me when new comments are added- checkbox and now every time a comment is added I receive 4 emails with the exact same comment. Perhaps there is an easy method you are able to remove me from that service? Cheers!
I do not know whether it’s just me or if perhaps everyone else experiencing issues with your site. It appears as if some of the text within your posts are running off the screen. Can somebody else please provide feedback and let me know if this is happening to them as well? This may be a issue with my web browser because I’ve had this happen before. Thanks
Hello, yeah this paragraph is genuinely fastidious and I have learned lot of things from it concerning blogging. thanks.
Does your website have a contact page? I’m having a tough time locating it but, I’d like to shoot you an email. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great website and I look forward to seeing it improve over time.
Whats up this is somewhat of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding experience so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
It’s a pity you don’t have a donate button! I’d most certainly donate to this outstanding blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to brand new updates and will share this site with my Facebook group. Chat soon!
Awesome post.
Great web site. Plenty of helpful info here. I’m sending it to a few buddies ans also sharing in delicious. And naturally, thanks on your effort!
These are actually impressive ideas in regarding blogging.
You have touched some nice points here. Any way keep
up wrinting.
What’s up everybody, here every one is sharing such experience, therefore it’s good to read this blog, and I used to pay a visit this weblog every day.
This is a topic that is near to my heart… Cheers! Exactly where are your contact details though?
I’m not that much of a online reader to be honest but your sites really nice, keep it up! I’ll go ahead and bookmark your site to come back in the future. Cheers
I was curious if you ever considered changing the layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having 1 or 2 pictures. Maybe you could space it out better?
Thanks in favor of sharing such a pleasant opinion, piece of writing is nice, thats why i have read it completely
Does your site have a contact page? I’m having problems locating it but, I’d like to shoot you an e-mail. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it grow over time.
Greetings from Florida! I’m bored to tears at work so I decided to browse your blog on my iphone during lunch break. I love the knowledge you present here and can’t wait to take a look when I get home. I’m shocked at how quick your blog loaded on my phone .. I’m not even using WIFI, just 3G .. Anyhow, good blog!
Hi to every one, the contents present at this web site are in fact remarkable for people knowledge, well, keep up the good work fellows.
Hello, its pleasant article concerning media print, we all be familiar with media is a enormous source of information.
I was wondering if you ever thought of changing the structure of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having 1 or two pictures. Maybe you could space it out better?
Wow, marvelous blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your web site is excellent, let alone the content!
I am truly thankful to the owner of this web page who has shared this great paragraph at here.
Hi there Dear, are you genuinely visiting this site on a regular basis, if so afterward you will without doubt obtain good knowledge.
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz reply as I’m looking to design my own blog and would like to know where u got this from. thanks a lot
Heya terrific website! Does running a blog similar to this take a massive amount work? I have no understanding of coding however I had been hoping to start my own blog in the near future. Anyway, if you have any ideas or techniques for new blog owners please share. I know this is off topic however I just had to ask. Thanks a lot!
First of all I would like to say awesome blog! I had a quick question in which I’d like to ask if you do not mind. I was curious to know how you center yourself and clear your head before writing. I have had a difficult time clearing my thoughts in getting my ideas out. I truly do enjoy writing but it just seems like the first 10 to 15 minutes tend to be lost simply just trying to figure out how to begin. Any suggestions or hints? Thank you!
Hey There. I found your blog using msn. This is a very well written article. I’ll be sure to bookmark it and come back to read more of your useful info. Thanks for the post. I’ll certainly return.
Link exchange is nothing else except it is only placing the other person’s website link on your page at suitable place and other person will also do same in support of you.
Hi there every one, here every one is sharing these kinds of know-how, thus it’s good to read this web site, and I used to pay a visit this blog all the time.
Hello just wanted to give you a brief heads up and let you know a few of the images aren’t loading properly. I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and both show the same results.
If you desire to take a great deal from this article then you have to apply these techniques to your won webpage.
I think everything wrote was very reasonable. However, think about this, suppose you typed a catchier title? I am not saying your content is not good., however suppose you added a headline that makes people want more? I mean %BLOG_TITLE% is a little vanilla. You ought to look at Yahoo’s home page and see how they write news titles to grab people to click. You might add a video or a pic or two to grab readers excited about what you’ve got to say. In my opinion, it would make your blog a little bit more interesting.
What’s up, the whole thing is going sound here and ofcourse every one is sharing data, that’s really fine, keep up writing.
Hi there! Do you know if they make any plugins to help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Cheers!
Hey! I could have sworn I’ve been to this blog before but after checking through some of the post I realized it’s new to me. Nonetheless, I’m definitely delighted I found it and I’ll be bookmarking and checking back often!
I am now not sure where you’re getting your info, however great topic. I needs to spend a while studying more or figuring out more. Thank you for fantastic info I used to be looking for this info for my mission.
Awesome post.
Whats up this is somewhat of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding skills so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
This article is truly a nice one it assists new net visitors, who are wishing in favor of blogging.
What a material of un-ambiguity and preserveness of precious familiarity about unexpected emotions.
Great delivery. Sound arguments. Keep up the good work.
Wow, this paragraph is pleasant, my younger sister is analyzing these kinds of things, therefore I am going to tell her.
Great site you have here but I was curious about if you knew of any forums that cover the same topics discussed in this article? I’d really love to be a part of group where I can get advice from other knowledgeable individuals that share the same interest. If you have any suggestions, please let me know. Thanks a lot!
Hello! I’m at work browsing your blog from my new apple iphone! Just wanted to say I love reading through your blog and look forward to all your posts! Carry on the fantastic work!
Hi, Neat post. There’s a problem along with your site in web explorer, may test this? IE still is the marketplace chief and a large portion of other folks will leave out your great writing due to this problem.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You obviously know what youre talking about, why throw away your intelligence on just posting videos to your weblog when you could be giving us something informative to read?
each time i used to read smaller articles or reviews that also clear their motive, and that is also happening with this piece of writing which I am reading at this place.
Howdy! I could have sworn I’ve been to your blog before but after going through many of the articles I realized it’s new to me. Anyhow, I’m definitely happy I came across it and I’ll be book-marking it and checking back regularly!
Hi! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly? My blog looks weird when viewing from my iphone. I’m trying to find a template or plugin that might be able to resolve this problem. If you have any suggestions, please share. Appreciate it!
Aw, this was an exceptionally nice post. Taking the time and actual effort to generate a very good article… but what can I say… I hesitate a lot and never seem to get anything done.
What i do not understood is in fact how you’re not actually a lot more neatly-appreciated than you may be right now. You’re so intelligent. You realize therefore considerably in the case of this matter, made me in my opinion believe it from numerous varied angles. Its like men and women aren’t interested until it’s one thing to accomplish with Woman gaga! Your personal stuffs outstanding. All the time handle it up!
Hi mates, its fantastic paragraph regarding teachingand fully defined, keep it up all the time.
Have you ever considered publishing an ebook or guest authoring on other websites? I have a blog based on the same subjects you discuss and would really like to have you share some stories/information. I know my audience would value your work. If you’re even remotely interested, feel free to send me an email.
I have read some good stuff here. Definitely worth bookmarking for revisiting. I surprise how a lot effort you put to create the sort of excellent informative website.
Thank you for every other informative website. Where else may just I get that kind of info written in such a perfect approach? I’ve a venture that I’m just now operating on, and I’ve been at the look out for such information.
I’m gone to convey my little brother, that he should also pay a quick visit this blog on regular basis to get updated from latest news update.
Thanks for one’s marvelous posting! I seriously enjoyed reading it, you’re a great author.I will always bookmark your blog and may come back at some point. I want to encourage one to continue your great work, have a nice weekend!
Hey! This post couldn’t be written any better! Reading through this post reminds me of my good old room mate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Many thanks for sharing!
Hi there to every one, because I am actually keen of reading this website’s post to be updated on a regular basis. It contains fastidious information.
Pretty! This was an incredibly wonderful post. Many thanks for providing this info.
Today, I went to the beach front with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is totally off topic but I had to tell someone!
Good day! I could have sworn I’ve visited this website before but after looking at a few of the posts I realized it’s new to me. Regardless, I’m certainly delighted I came across it and I’ll be bookmarking it and checking back often!
Howdy! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
What’s up, I log on to your new stuff regularly. Your humoristic style is awesome, keep it up!
I really like your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to design my own blog and would like to find out where u got this from. thank you
Why users still make use of to read news papers when in this technological globe everything is available on web?
Hi there! This is my 1st comment here so I just wanted to give a quick shout out and tell you I genuinely enjoy reading your articles. Can you suggest any other blogs/websites/forums that go over the same subjects? Thank you so much!
Piece of writing writing is also a fun, if you know then you can write otherwise it is complicated to write.
Hi, i think that i saw you visited my weblog thus i came to “return the favor”.I am attempting to find things to improve my website!I suppose its ok to use some of your ideas!!
Evlerinde verilen partide; kocasından yediği tokatla hayatı değişen Amrita, bunu kabullenmek yerine, üzerine gitmeye karar verir. Film: Anubhav Sushile’nin yaşamış olduğu gerçek olaylara dayanmaktadır. Ken Langford
Parrish ve manajeri karakterleri birbiriyle uyuşmayıp hatta belkide tam zıt karakterde olsalarda birbirleriyle anlaşabilme konusunda iyidirler.Parrish bir karar alır, aldığı bu karar yaşadığı büyük şehirden eski şirin kasabasına dönmek istemesidir. Parrish’in eski kasabasına dönerler. Brooks Denney
What’s up, I wish for to subscribe for this webpage to take newest updates, so where can i do it please help out.
I came. I read it. I thought a lot.
It’s an amazing article in favor of all the web people; they will obtain benefit from it I am sure.
Başarılı bir suç romanı yazarı, yeni kitabı için yolsuzluk meselesini araştırırken gerçekle kurguyu birbirine karıştırmaya başlar. Pedro Alonso (“La casa de papel”) ve Nacho Fresneda (“El Ministerio del Tiempo”) başrollerde. Yönetmen Marc Vigil…Bataklığın Sessizliği izle Trey Sundin
Hello, i think that i saw you visited my weblog thus i came to “return the favor”.I am trying to find things to improve my website!I suppose its ok to use some of your ideas!!
Hi, i think that i saw you visited my website so i came to “return the favor”.I am attempting to find things to improve my site!I suppose its ok to use a few of your ideas!!
Nice post. I was checking continuously this blog and I’m impressed! Extremely useful info specifically the last part 🙂 I care for such info a lot. I was seeking this certain info for a long time. Thank you and best of luck.
Hey, I think your site might be having browser compatibility issues. When I look at your blog in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, wonderful blog!
Keep this going please, great job!
Hi, Neat post. There’s a problem together with your site in internet explorer, could test this? IE still is the marketplace leader and a huge component to folks will pass over your great writing due to this problem.
When I initially commented I seem to have clicked on the -Notify me when new comments are added- checkbox and from now on every time a comment is added I get 4 emails with the exact same comment. Is there a way you are able to remove me from that service? Thanks!
That is a good tip particularly to those new to the blogosphere. Brief but very precise info… Thank you for sharing this one. A must read post!
What i don’t understood is in truth how you are not really much more well-favored than you may be now. You are so intelligent. You already know thus considerably in the case of this subject, produced me for my part consider it from a lot of varied angles. Its like women and men don’t seem to be interested except it’s one thing to accomplish with Girl gaga! Your own stuffs excellent. At all times take care of it up!
It’s a pity you don’t have a donate button! I’d without a doubt donate to this fantastic blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to fresh updates and will talk about this website with my Facebook group. Chat soon!
of course like your website however you need to take a look at the spelling on several of your posts. Several of them are rife with spelling issues and I in finding it very troublesome to inform the reality however I’ll definitely come back again.
I enjoy what you guys tend to be up too. This kind of clever work and reporting! Keep up the terrific works guys I’ve included you guys to our blogroll.
liquid tadalafil
Sleeve Gastrectomy – Cosmetique News
Great answer, congratulations
Thank you so much for your support. I should.
Right here is the right webpage for anyone who wishes to understand this topic. You know so much its almost tough to argue with you (not that I actually would want to…HaHa). You certainly put a brand new spin on a topic that’s been written about for a long time. Great stuff, just excellent!
Hi, all the time i used to check webpage posts here early in the break of day, since i like to find out more and more.
Hi to every body, it’s my first pay a visit of this webpage; this web site carries awesome and really good stuff in support of visitors.
May I just say what a relief to find somebody who genuinely understands what they are talking about on the internet. You actually realize how to bring a problem to light and make it important. More people really need to read this and understand this side of the story. I was surprised that you’re not more popular because you definitely possess the gift.
Your style is so unique in comparison to other people I’ve read stuff from. Thank you for posting when you’ve got the opportunity, Guess I’ll just bookmark this page.
I’ve been surfing online more than 4 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my view, if all site owners and bloggers made good content as you did, the web will be a lot more useful than ever before.
Outstanding post however I was wanting to know if you could write a litte more on this topic? I’d be very thankful if you could elaborate a little bit further. Appreciate it!
Fastidious response in return of this difficulty with real arguments and explaining everything regarding that.
This piece of writing will help the internet users for setting up new blog or even a weblog from start to end.
Hello colleagues, its enormous paragraph regarding tutoringand entirely defined, keep it up all the time.
It’s amazing to go to see this web page and reading the views of all colleagues on the topic of this piece of writing, while I am also eager of getting know-how.
I like what you guys are usually up too. This sort of clever work and coverage! Keep up the amazing works guys I’ve incorporated you guys to my blogroll.
Someone essentially help to make critically articles I’d state. This is the first time I frequented your website page and so far? I amazed with the analysis you made to make this actual submit amazing. Wonderful task!
Hey there! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly? My web site looks weird when viewing from my iphone. I’m trying to find a theme or plugin that might be able to resolve this issue. If you have any recommendations, please share. Cheers!
Hmm it appears like your blog ate my first comment (it was extremely long) so I guess I’ll just sum it up what I had written and say, I’m thoroughly enjoying your blog. I too am an aspiring blog writer but I’m still new to the whole thing. Do you have any helpful hints for novice blog writers? I’d really appreciate it.
Wow that was odd. I just wrote an incredibly long comment but after I clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say superb blog!
Greetings! I know this is kinda off topic but I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa? My blog covers a lot of the same subjects as yours and I feel we could greatly benefit from each other. If you might be interested feel free to send me an e-mail. I look forward to hearing from you! Terrific blog by the way!
Nice post. I learn something new and challenging on sites I stumbleupon every day. It’s always interesting to read content from other authors and practice something from their web sites.
Heya i am for the first time here. I came across this board and I to find It really useful & it helped me out a lot. I’m hoping to provide one thing back and aid others such as you helped me.
We’re a group of volunteers and opening a new scheme in our community. Your web site offered us with valuable information to work on. You have done an impressive job and our entire community will be grateful to you.
I have read so many content concerning the blogger lovers but this piece of writing is actually a good paragraph, keep it up.
I am no longer sure the place you’re getting your info, however great topic. I needs to spend some time learning much more or understanding more. Thank you for wonderful information I used to be on the lookout for this information for my mission.
Everyone loves what you guys are usually up too. This type of clever work and coverage! Keep up the amazing works guys I’ve incorporated you guys to our blogroll.
Excellent, what a weblog it is! This webpage gives valuable data to us, keep it up.
You really make it seem really easy along with your presentation however I find this matter to be really one thing which I think I would never understand. It seems too complicated and very vast for me. I am looking forward on your subsequent post, I’ll try to get the dangle of it!
Hi there, after reading this awesome post i am also happy to share my know-how here with colleagues.
I visited several web pages however the audio quality for audio songs present at this website is really marvelous.
This site was… how do I say it? Relevant!! Finally I have found something that helped me. Many thanks!
Hello, I think your site might be having browser compatibility issues. When I look at your blog site in Ie, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, excellent blog!
I’ve learn a few excellent stuff here. Certainly value bookmarking for revisiting. I surprise how a lot attempt you put to create this sort of fantastic informative web site.
Great post.
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your webpage? My blog is in the exact same niche as yours and my users would definitely benefit from a lot of the information you present here. Please let me know if this alright with you. Regards!
Hi, i think that i saw you visited my blog thus i came to “return the favor”.I am trying to find things to enhance my site!I suppose its ok to use some of your ideas!!
I’m not that much of a online reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back later. Many thanks
Thanks , I’ve just been looking for information approximately this topic for ages and yours is the best I’ve came upon so far. However, what in regards to the bottom line? Are you positive about the supply?
Have you ever considered publishing an ebook or guest authoring on other websites? I have a blog centered on the same ideas you discuss and would love to have you share some stories/information. I know my viewers would appreciate your work. If you’re even remotely interested, feel free to send me an e mail.
You made some decent points there. I looked on the web for additional information about the issue and
found most people will go along with your views on this site.
Wow, this post is fastidious, my younger sister is analyzing such things, so I am going to convey her.
Everyone loves it when individuals come together and share opinions. Great site, keep it up!
Great blog you have here.. It’s hard to find quality writing like yours nowadays. I honestly appreciate individuals like you! Take care!!
Film, Afrika’daki uyku hastalığıyla mücadele eden biri beyaz Alman, biri de zenci Fransız iki doktoru gözlemliyor. Dr. Ebbo Veltman, Kamerun’daki hastalıkla mücadele eden bir program yürütüyor. Bu ülkenin nehirlerine, ormanlarına da delicesine âşık. Fakat başarılarına rağmen, ailesi bir an önce Avrupa’ya dönmeye hevesli. Dünya Sağlık Örgütü tarafından onun yerine Fransa’dan bir doktorun geçmesine karar veriyor. Genç doktor Alex Nzila Kamerun’daki kliniğe vardığında burada karmakarışık bir ortam ve psikolojik desteğe ihtiyacı olan Veltman’ı buluyor. Jules Ziyad
Wow, wonderful weblog structure! How long have you ever been blogging for? you make running a blog look easy. The full look of your site is magnificent, as neatly as the content!
Quality articles or reviews is the important to be a focus for the users to pay a quick visit the site, that’s what this web page is providing.
Very nice article, just what I wanted to find.
What’s up to every body, it’s my first pay a quick visit of this blog; this blog consists of amazing and genuinely good data designed for visitors.
For the reason that the admin of this web site is working, no hesitation very shortly it will be renowned, due to its quality contents.
Hello everyone, it’s my first pay a visit at this web page, and paragraph is really fruitful designed for me, keep up posting these articles.
My family members all the time say that I am wasting my time here at web, however I know I am getting familiarity everyday by reading thes good articles or reviews.
What’s up everybody, here every person is sharing these experience, thus it’s pleasant to read this website, and I used to pay a visit this web site daily.
I am actually happy to read this webpage posts which includes plenty of useful data, thanks for providing such statistics.
What’s up, after reading this amazing post i am as well happy to share my familiarity here with colleagues.
Oh my goodness! Incredible article dude! Thank you, However I am encountering problems with your RSS. I don’t know why I cannot subscribe to it. Is there anyone else having similar RSS problems? Anyone who knows the answer will you kindly respond? Thanx!!
Remarkable! Its really amazing paragraph, I have got much clear idea about from this piece of writing.
Thanks for some other fantastic article. The place else could anyone get that type of info in such a perfect way of writing? I have a presentation subsequent week, and I am at the look for such information.
Hello to every body, it’s my first pay a visit of this website; this web site consists of amazing and genuinely excellent stuff for visitors.
It’s actually very complex in this active life to listen news on TV, so I simply use world wide web for that purpose, and take the most up-to-date news.
It’s going to be ending of mine day, but before end I am reading this enormous piece of writing to increase my knowledge.
extended essay help
Sleeve Gastrectomy – Cosmetique News
Marvelous, what a blog it is! This weblog gives valuable facts to us, keep it up.
fast essay writing service
Sleeve Gastrectomy – Cosmetique News
I want and take
You need to be a part of a contest for one of the highest quality websites on the net. I will recommend this site!
best writing service
Sleeve Gastrectomy – Cosmetique News
What i don’t understood is in fact how you’re now not actually much more well-favored than you might be now. You’re very intelligent. You realize thus considerably relating to this topic, produced me in my view consider it from so many numerous angles. Its like women and men aren’t fascinated unless it is one thing to accomplish with Girl gaga! Your individual stuffs nice. All the time take care of it up!
academic essay writing service
Sleeve Gastrectomy – Cosmetique News
college essay writing services
Sleeve Gastrectomy – Cosmetique News
I’ve been exploring for a little for any high-quality articles or weblog posts on this sort of area . Exploring in Yahoo I finally stumbled upon this site. Reading this information So i’m glad to exhibit that I’ve a very just right uncanny feeling I came upon just what I needed. I most without a doubt will make sure to don?t put out of your mind this web site and give it a look regularly.
i need help with my essay
Sleeve Gastrectomy – Cosmetique News
This post is really a nice one it assists new web users, who are wishing for blogging.
Heya fantastic blog! Does running a blog such as this take a lot of work? I have virtually no expertise in coding but I was hoping to start my own blog in the near future. Anyhow, if you have any recommendations or techniques for new blog owners please share. I understand this is off topic nevertheless I simply had to ask. Kudos!
SHOULD LOOK)))
This is my first time go to see at here and i am in fact impressed to read everthing at alone place.
I could not refrain from commenting. Well written!
best essay writing service online
Sleeve Gastrectomy – Cosmetique News
Quality articles is the secret to attract the users to visit the website, that’s what this website is providing.
english essay help online
Sleeve Gastrectomy – Cosmetique News
online essay writers wanted
Sleeve Gastrectomy – Cosmetique News
With havin so much content and articles do you ever run into any problems of plagorism or copyright infringement? My blog has a lot of exclusive content I’ve either written myself or outsourced but it seems a lot of it is popping it up all over the web without my authorization. Do you know any techniques to help stop content from being stolen? I’d really appreciate it.
Having read this I believed it was very informative. I appreciate you spending some time and effort to put this content together. I once again find myself spending a significant amount of time both reading and commenting. But so what, it was still worthwhile!
essay proofreading service
Sleeve Gastrectomy – Cosmetique News
custom essays writing
Sleeve Gastrectomy – Cosmetique News
cheapest custom essays
Sleeve Gastrectomy – Cosmetique News
best mba essay editing service
Sleeve Gastrectomy – Cosmetique News
Excellent pieces. Keep writing such kind of info on your blog. Im really impressed by your site.
Hello there, You have performed a great job. I will definitely digg it and personally recommend to my friends. I’m sure they’ll be benefited from this web site.
compare and contrast essay help
Sleeve Gastrectomy – Cosmetique News
Hi there I am so glad I found your website, I really found you by accident, while I was researching on Aol for something else, Nonetheless I am here now and would just like to say cheers for a marvelous post and a all round interesting blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have saved it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the superb work.
hello there and thank you for your information – I have definitely picked up something new from right here. I did however expertise several technical issues using this website, since I experienced to reload the website lots of times previous to I could get it to load correctly. I had been wondering if your hosting is OK? Not that I’m complaining, but sluggish loading instances times will very frequently affect your placement in google and could damage your quality score if advertising and marketing with Adwords. Anyway I am adding this RSS to my email and can look out for a lot more of your respective exciting content. Ensure that you update this again very soon.
Hmm is anyone else encountering problems with the images on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any feed-back would be greatly appreciated.
I loved as much as you will receive carried out right here. The sketch is attractive, your authored subject matter stylish. nonetheless, you command get got an nervousness over that you wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this increase.
I am really inspired with your writing talents and also with the format in your blog. Is that this a paid theme or did you modify it your self? Anyway keep up the nice high quality writing, it’s uncommon to look a great blog like this one today..
It’s very trouble-free to find out any matter on net as compared to books, as I found this post at this site.
Quality articles or reviews is the crucial to interest the visitors to pay a quick visit the web page, that’s what this web site is providing.
Nice respond in return of this question with real arguments and describing everything concerning that.
Hello there! Do you use Twitter? I’d like to follow you if that would be ok. I’m definitely enjoying your blog and look forward to new posts.
Hi there, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam responses? If so how do you protect against it, any plugin or anything you can recommend? I get so much lately it’s driving me insane so any support is very much appreciated.
Hello to all, the contents present at this web site are really amazing for people experience, well, keep up the good work fellows.
I have read some just right stuff here. Certainly value bookmarking for revisiting. I wonder how so much attempt you set to make this sort of excellent informative website.
Why people still make use of to read news papers when in this technological globe all is available on web?
Excellent blog here! Also your web site loads up fast! What web host are you using? Can I get your affiliate link to your host? I wish my site loaded up as quickly as yours lol
What the right words … super, great idea
Ahaa, its pleasant dialogue about this piece of writing here at this webpage, I have read all that, so now me also commenting here.
For hottest news you have to pay a visit web and on internet I found this site as a finest web site for most recent updates.
It’s going to be end of mine day, but before end I am reading this fantastic post to increase my experience.
When some one searches for his vital thing, thus he/she desires to be available that in detail, thus that thing is maintained over here.
Everything is very open with a precise clarification of the challenges. It was really informative. Your website is extremely helpful. Thank you for sharing!
If you wish for to get a great deal from this article then you have to apply such strategies to your won web site.
I’m really impressed with your writing skills and also with the layout on your weblog. Is this a paid theme or did you modify it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one today.
buy priligy online pharmacy
Sleeve Gastrectomy – Cosmetique News
Shine
online pharmacy no prescription ambien
Sleeve Gastrectomy – Cosmetique News
rx specialty pharmacy
Sleeve Gastrectomy – Cosmetique News
Its like you read my mind! You appear to know so much about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a bit, but other than that, this is great blog. An excellent read. I’ll certainly be back.
envision rx pharmacy
Sleeve Gastrectomy – Cosmetique News
Hey! I could have sworn I’ve been to this website before but after browsing through some of the post I realized it’s new to me. Anyhow, I’m definitely delighted I found it and I’ll be book-marking and checking back often!
Thank you for sharing your thoughts. I truly appreciate your efforts and I will be waiting for your next write ups thanks once again.
I am not certain where you’re getting your information, but great topic. I needs to spend some time learning much more or working out more. Thank you for magnificent info I was on the lookout for this info for my mission.
I was recommended this website by means of my cousin. I’m not certain whether this put up is written through him as no one else understand such targeted approximately my problem. You’re incredible! Thank you!
viagra pfizer online pharmacy
viagra pfizer online pharmacy
Hello There. I found your weblog using msn. This is an extremely smartly written article. I will make sure to bookmark it and come back to read extra of your helpful info. Thanks for the post. I will certainly comeback.
purchase tadalafil
purchase tadalafil
I am extremely impressed with your writing skills as well as with the layout on your weblog. Is this a paid theme or did you modify it yourself? Anyway keep up the nice quality writing, it’s rare to see a great blog like this one these days.
I’ve been browsing online more than 2 hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. In my opinion, if all webmasters and bloggers made good content as you did, the web will be a lot more useful than ever before.
buy viagra online best price
buy viagra online best price
It’s hard to come by educated people on this topic, but you seem like you know what you’re talking about! Thanks
Thank you for any other informative site. Where else may just I get that type of information written in such a perfect means? I have a mission that I’m simply now operating on, and I have been at the look out for such information.
More of these blog posts.
I wanted to thank you for this very good read!! I absolutely loved every bit of it. I have got you book marked to look at new stuff you post…
I have read so many articles on the topic of the blogger lovers except this article is actually a fastidious piece of writing, keep it up.
Generally I do not read post on blogs, but I wish to say that this write-up very pressured me to try and do it! Your writing taste has been amazed me. Thank you, very nice post.
Heya i’m for the first time here. I found this board and I find It truly useful & it helped me out much. I hope to give something back and help others like you aided me.
It’s a shame you don’t have a donate button! I’d most certainly donate to this fantastic blog! I guess for now i’ll settle for bookmarking and adding your RSS feed to my Google account. I look forward to brand new updates and will share this website with my Facebook group. Talk soon!
canadian pharmacy cialis
canadian pharmacy cialis
I accept it with pleasure. In my opinion, this is relevant, I will take part in the discussion.
Hi, I do think this is an excellent website. I stumbledupon it 😉 I’m going to come back once again since I book marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
What’s up, the whole thing is going fine here and ofcourse every one is sharing facts, that’s actually good, keep up writing.
I know this website gives quality based posts and other material, is there any other site which gives these kinds of data in quality?
Yesterday, while I was at work, my cousin stole my apple ipad and tested to see if it can survive a 30 foot drop, just so she can be a youtube sensation. My apple ipad is now broken and she has 83 views. I know this is totally off topic but I had to share it with someone!
Hello friends, its impressive piece of writing regarding tutoringand fully explained, keep it up all the time.
hello!,I like your writing so so much! proportion we keep in touch extra about your article on AOL? I need a specialist in this area to unravel my problem. May be that’s you! Looking forward to peer you.
This is really interesting, You’re a very skilled blogger. I have joined your rss feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
For latest information you have to go to see world-wide-web and on internet I found this web page as a best web page for latest updates.
After I originally commented I seem to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added I receive four emails with the exact same comment. Perhaps there is a means you can remove me from that service? Kudos!
Hello there! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly? My web site looks weird when viewing from my iphone 4. I’m trying to find a template or plugin that might be able to fix this problem. If you have any recommendations, please share. Appreciate it!
This excellent website certainly has all of the information I needed about this subject and didn’t know who to ask.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You obviously know what youre talking about, why throw away your intelligence on just posting videos to your blog when you could be giving us something informative to read?
I am actually delighted to read this web site posts which includes lots of helpful data, thanks for providing such information.
sildenafil australia
Appreciate the recommendation. Let me try it out.
That is a really good tip particularly to those new to the blogosphere. Short but very accurate info… Many thanks for sharing this one. A must read post!
I visited multiple web pages but the audio quality for audio songs present at this website is genuinely superb.
Definitely believe that which you stated. Your favorite reason appeared to be on the web the simplest thing to be aware of. I say to you, I definitely get irked while people think about worries that they plainly don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side-effects , people can take a signal. Will probably be back to get more. Thanks
cialis tadalafil 10mg tablets
cialis tadalafil 10mg tablets
Heya i am for the first time here. I came across this board and I find It really useful & it helped me out much. I hope to give something back and help others like you aided me.
buy generic viagra 100mg online
buy generic viagra 100mg online
Do you have a spam issue on this website; I also am a blogger, and I was curious about your situation; many of us have created some nice practices and we are looking to exchange techniques with others, please shoot me an email if interested.
cheap viagra 100 online
cheap viagra 100 online
cialis from canada
cialis from canada
where can i buy sildenafil
where can i buy sildenafil
how much should viagra cost
how much should viagra cost
I think this is among the so much significant information for me. And i’m satisfied studying your article. But want to statement on some general things, The website taste is ideal, the articles is really great : D. Just right process, cheers
Howdy, I do think your website could possibly be having browser compatibility problems. When I look at your blog in Safari, it looks fine but when opening in I.E., it has some overlapping issues. I merely wanted to give you a quick heads up! Apart from that, excellent website!
Hello! I’ve been reading your web site for some time now and finally got the bravery to go ahead and give you a shout out from Kingwood Tx! Just wanted to mention keep up the good work!
sildenafil prescription canada
sildenafil prescription canada
Good way of explaining, and pleasant paragraph to obtain facts regarding my presentation topic, which i am going to convey in institution of higher education.
Wonderful items from you, man. I have remember your stuff previous to and you are simply too wonderful. I really like what you have obtained here, really like what you are stating and the best way during which you say it. You’re making it entertaining and you continue to care for to stay it wise. I cant wait to learn far more from you. This is actually a tremendous website.
We stumbled over here coming from a different website and thought I should check things out. I like what I see so i am just following you. Look forward to going over your web page yet again.
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a bit, but instead of that, this is magnificent blog. An excellent read. I will definitely be back.
I’ve been surfing online more than 3 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. Personally, if all website owners and bloggers made good content as you did, the web will be a lot more useful than ever before.
Hi there, its pleasant post regarding media print, we all be aware of media is a fantastic source of facts.
great points altogether, you simply won a brand new reader. What could you suggest in regards to your put up that you made a few days in the past? Any sure?
With havin so much content and articles do you ever run into any issues of plagorism or copyright violation? My website has a lot of completely unique content I’ve either written myself or outsourced but it appears a lot of it is popping it up all over the internet without my authorization. Do you know any methods to help prevent content from being stolen? I’d truly appreciate it.
Attractive section of content. I just stumbled upon your site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Anyway I’ll be subscribing to your augment and even I achievement you access consistently rapidly.
Hello There. I found your blog the usage of msn. This is a really neatly written article. I’ll be sure to bookmark it and come back to read more of your helpful information. Thank you for the post. I’ll definitely return.
Admiring the time and energy you put into your site and detailed information you offer. It’s good to come across a blog every once in a while that isn’t the same unwanted rehashed material. Excellent read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
Wow, this paragraph is nice, my younger sister is analyzing such things, therefore I am going to tell her.
Hi! I know this is sort of off-topic however I had to ask. Does managing a well-established website such as yours take a massive amount work? I’m brand new to blogging but I do write in my diary daily. I’d like to start a blog so I can share my personal experience and feelings online. Please let me know if you have any ideas or tips for brand new aspiring bloggers. Thankyou!
Its not my first time to go to see this website, i am visiting this website dailly and take good data from here every day.
Hi, just wanted to mention, I liked this article. It was funny. Keep on posting!
Fantastic beat ! I wish to apprentice while you amend your site, how can i subscribe for a blog web site? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear concept
Hi there, I believe your blog could be having browser compatibility issues. Whenever I take a look at your site in Safari, it looks fine however, when opening in IE, it has some overlapping issues. I just wanted to give you a quick heads up! Apart from that, great website!
I truly love your website.. Excellent colors & theme. Did you build this amazing site yourself? Please reply back as I’m hoping to create my very own blog and would like to know where you got this from or exactly what the theme is called. Kudos!
With havin so much written content do you ever run into any problems of plagorism or copyright violation? My website has a lot of unique content I’ve either written myself or outsourced but it looks like a lot of it is popping it up all over the internet without my agreement. Do you know any solutions to help protect against content from being ripped off? I’d definitely appreciate it.
Hello there! I could have sworn I’ve visited this web site before but after looking at some of the posts I realized it’s new to me. Regardless, I’m definitely delighted I came across it and I’ll be bookmarking it and checking back regularly!
Excellent article. Keep posting such kind of info on your page. Im really impressed by your blog.
Hi there, You have performed an excellent job. I will definitely digg it and in my view recommend to my friends. I’m confident they will be benefited from this web site.
If you are going for finest contents like myself, only pay a quick visit this website all the time because it presents quality contents, thanks
Hello, i think that i saw you visited my website so i came to “return the favor”.I am attempting to find things to enhance my site!I suppose its ok to use a few of your ideas!!
I am now not certain the place you’re getting your information, but good topic. I needs to spend a while studying much more or figuring out more. Thanks for excellent information I was in search of this information for my mission.
My brother recommended I might like this website. He was entirely right. This post truly made my day. You cann’t imagine simply how much time I had spent for this info! Thanks!
I’m amazed, I have to admit. Seldom do I encounter a blog that’s both educative and amusing, and without a doubt, you have hit the nail on the head. The issue is something too few people are speaking intelligently about. I am very happy I found this in my search for something regarding this.
That was my fault.
I know this website presents quality dependent content and other material, is there any other web page which provides these information in quality?
I do not even know how I ended up here, but I thought this post was good. I do not know who you are but certainly you’re going to a famous blogger if you are not already 😉 Cheers!
Hello There. I found your weblog the usage of msn. That is a really smartly written article. I’ll make sure to bookmark it and come back to read more of your helpful info. Thanks for the post. I’ll certainly return.
Having read this I believed it was extremely enlightening. I appreciate you finding the time and effort to put this short article together. I once again find myself spending a lot of time both reading and posting comments. But so what, it was still worth it!
My brother suggested I might like this web site. He was entirely right. This post truly made my day. You cann’t imagine simply how much time I had spent for this information! Thanks!
Greetings! I know this is kind of off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having problems finding one? Thanks a lot!
Hello there! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new posts.
fake cialis pictures
fake cialis pictures
Hello, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam feedback? If so how do you reduce it, any plugin or anything you can advise? I get so much lately it’s driving me insane so any support is very much appreciated.
Everything is very open with a clear description of the issues. It was really informative. Your website is extremely helpful. Thank you for sharing!
Do you mind if I quote a few of your articles as long as I provide credit and sources back to your website? My website is in the exact same niche as yours and my users would truly benefit from some of the information you present here. Please let me know if this alright with you. Thanks!
What’s up, this weekend is good in favor of me, as this time i am reading this wonderful educational article here at my home.
Very great post. I simply stumbled upon your blog and wanted to mention that I’ve truly loved surfing around your weblog posts. In any case I’ll be subscribing in your rss feed and I hope you write again soon!
Hello, I would like to subscribe for this webpage to take hottest updates, so where can i do it please assist.
Hello! I know this is kinda off topic nevertheless I’d figured I’d ask. Would you be interested in trading links or maybe guest writing a blog post or vice-versa? My site goes over a lot of the same subjects as yours and I think we could greatly benefit from each other. If you are interested feel free to send me an e-mail. I look forward to hearing from you! Fantastic blog by the way!
Hey there I am so grateful I found your webpage, I really found you by error, while I was researching on Google for something else, Anyways I am here now and would just like to say cheers for a marvelous post and a all round exciting blog (I also love the theme/design), I don’t have time to read it all at the moment but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the excellent jo.
I used to be able to find good information from your articles.
Very soon this website will be famous among all blogging and site-building users, due to it’s nice articles or reviews
Your style is very unique in comparison to other folks I’ve read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I will just bookmark this blog.
If some one desires expert view about running a blog afterward i recommend him/her to go to see this web site, Keep up the pleasant job.
Hi there fantastic blog! Does running a blog like this require a large amount of work? I’ve no understanding of programming but I had been hoping to start my own blog in the near future. Anyway, should you have any recommendations or tips for new blog owners please share. I know this is off subject however I simply needed to ask. Thanks!
I have been browsing online more than three hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my opinion, if all web owners and bloggers made good content as you did, the net will be much more useful than ever before.
Hello there! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one? Thanks a lot!
Hey there just wanted to give you a quick heads up. The text in your article seem to be running off the screen in Firefox. I’m not sure if this is a format issue or something to do with internet browser compatibility but I thought I’d post to let you know. The design and style look great though! Hope you get the problem solved soon. Many thanks
That is very fascinating, You are an excessively professional blogger. I’ve joined your feed and look ahead to in the hunt for more of your great post. Additionally, I have shared your web site in my social networks
Great info. Lucky me I found your site by accident (stumbleupon). I’ve saved it for later!
Wow! This blog looks exactly like my old one! It’s on a entirely different topic but it has pretty much the same layout and design. Great choice of colors!
Howdy, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam comments? If so how do you reduce it, any plugin or anything you can recommend? I get so much lately it’s driving me crazy so any assistance is very much appreciated.
Wow, that’s what I was exploring for, what a information! existing here at this weblog, thanks admin of this web page.
Magnificent beat ! I wish to apprentice while you amend your website, how could i subscribe for a blog site? The account helped me a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright clear idea
I like the helpful information you provide in your articles. I’ll bookmark your weblog and check again here regularly. I am quite sure I’ll learn a lot of new stuff right here! Good luck for the next!
Hi, all the time i used to check webpage posts here early in the daylight, as i like to gain knowledge of more and more.
Greetings from Colorado! I’m bored to death at work so I decided to check out your blog on my iphone during lunch break. I enjoy the knowledge you present here and can’t wait to take a look when I get home. I’m surprised at how quick your blog loaded on my phone .. I’m not even using WIFI, just 3G .. Anyhow, very good blog!
Hi there, You’ve done an excellent job. I’ll certainly digg it and personally recommend to my friends. I’m sure they’ll be benefited from this site.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You clearly know what youre talking about, why throw away your intelligence on just posting videos to your weblog when you could be giving us something enlightening to read?
What a data of un-ambiguity and preserveness of valuable know-how about unexpected feelings.
It’s going to be finish of mine day, except before finish I am reading this enormous piece of writing to improve my experience.
Hello would you mind letting me know which web host you’re using? I’ve loaded your blog in 3 different internet browsers and I must say this blog loads a lot faster then most. Can you suggest a good internet hosting provider at a fair price? Kudos, I appreciate it!
Hmm is anyone else having problems with the pictures on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any responses would be greatly appreciated.
Hi, after reading this awesome post i am as well delighted to share my familiarity here with mates.
Wonderful goods from you, man. I’ve understand your stuff previous to and you are just too magnificent. I really like what you’ve acquired here, certainly like what you are stating and the way in which you say it. You make it entertaining and you still care for to keep it wise. I can not wait to read far more from you. This is really a terrific web site.
you are truly a just right webmaster. The web site loading pace is incredible. It seems that you’re doing any distinctive trick. Furthermore, The contents are masterpiece. you’ve done a excellent job on this topic!
I feel that is among the most important info for me. And i am satisfied reading your article. But should statement on some general issues, The website style is wonderful, the articles is in reality great : D. Good process, cheers
I constantly spent my half an hour to read this weblog’s content everyday along with a cup of coffee.
you’re truly a excellent webmaster. The site loading velocity is incredible. It sort of feels that you’re doing any distinctive trick. In addition, The contents are masterwork. you have performed a great task in this subject!
Hi there to all, how is the whole thing, I think every one is getting more from this web site, and your views are fastidious for new viewers.
Hi, i think that i noticed you visited my web site so i got here to go back the prefer?.I’m trying to to find things to enhance my website!I suppose its adequate to use some of your ideas!!
What’s up, every time i used to check blog posts here early in the dawn, since i love to learn more and more.
Thanks to my father who shared with me on the topic of this webpage, this website is in fact remarkable.
This paragraph is actually a pleasant one it helps new web people, who are wishing in favor of blogging.
Hey there! Would you mind if I share your blog with my zynga group? There’s a lot of folks that I think would really enjoy your content. Please let me know. Many thanks
Does your website have a contact page? I’m having trouble locating it but, I’d like to send you an email. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it expand over time.
Hi there, all is going sound here and ofcourse every one is sharing facts, that’s genuinely fine, keep up writing.
Does your website have a contact page? I’m having a tough time locating it but, I’d like to shoot you an e-mail. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it grow over time.
Hey I am so thrilled I found your weblog, I really found you by mistake, while I was looking on Yahoo for something else, Regardless I am here now and would just like to say thanks a lot for a marvelous post and a all round thrilling blog (I also love the theme/design), I don’t have time to look over it all at the minute but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read much more, Please do keep up the fantastic b.
I blog often and I seriously thank you for your content. This article has really peaked my interest. I’m going to take a note of your website and keep checking for new information about once a week. I subscribed to your Feed as well.
Amazing! This blog looks just like my old one! It’s on a entirely different topic but it has pretty much the same layout and design. Superb choice of colors!
It’s an awesome post in support of all the online people; they will obtain benefit from it I am sure.
Heya! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing several weeks of hard work due to no back up. Do you have any methods to prevent hackers?
Attractive section of content. I just stumbled upon your weblog and in accession capital to assert that I acquire actually enjoyed account your blog posts. Anyway I’ll be subscribing to your feeds and even I achievement you access consistently quickly.
Hmm is anyone else experiencing problems with the images on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any responses would be greatly appreciated.
I’m amazed, I have to admit. Seldom do I come across a blog that’s both educative and entertaining, and without a doubt, you’ve hit the nail on the head. The issue is something too few folks are speaking intelligently about. I am very happy I found this in my search for something regarding this.
I constantly emailed this web site post page to all my contacts, since if like to read it afterward my links will too.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You clearly know what youre talking about, why waste your intelligence on just posting videos to your site when you could be giving us something enlightening to read?
When someone writes an post he/she retains the idea of a user in his/her brain that how a user can know it. Therefore that’s why this paragraph is amazing. Thanks!
You can certainly see your skills within the work you write. The arena hopes for even more passionate writers like you who aren’t afraid to mention how they believe. Always follow your heart.
It is the best time to make some plans for the future and it’s time to be happy. I have read this post and if I could I wish to suggest you few interesting things or suggestions. Perhaps you can write next articles referring to this article. I want to read even more things about it!
This post gives clear idea in favor of the new viewers of blogging, that really how to do blogging and site-building.
Fantastic beat ! I would like to apprentice whilst you amend your website, how can i subscribe for a weblog website? The account aided me a acceptable deal. I were a little bit acquainted of this your broadcast provided shiny transparent concept
Hi, I do believe this is a great site. I stumbledupon it 😉 I’m going to come back yet again since i have saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.
Really when someone doesn’t be aware of then its up to other users that they will assist, so here it happens.
This is a really good tip especially to those fresh to the blogosphere. Brief but very precise information… Many thanks for sharing this one. A must read article!
I’ve been browsing on-line more than three hours as of late, yet I never discovered any attention-grabbing article like yours. It is lovely value enough for me. In my opinion, if all site owners and bloggers made excellent content material as you did, the net shall be a lot more useful than ever before.
Yes! Finally someone writes about %keyword1%.
Marvelous, what a webpage it is! This blog presents helpful information to us, keep it up.
Every weekend i used to pay a quick visit this site, for the reason that i wish for enjoyment, since this this website conations truly pleasant funny data too.
I know this website offers quality dependent articles or reviews and additional material, is there any other web page which offers these kinds of data in quality?
This is the right web site for anyone who wishes to understand this topic. You understand a whole lot its almost hard to argue with you (not that I actually would want to…HaHa). You definitely put a brand new spin on a subject which has been discussed for a long time. Wonderful stuff, just wonderful!
Excellent beat ! I wish to apprentice even as you amend your site, how can i subscribe for a blog site? The account aided me a appropriate deal. I have been tiny bit familiar of this your broadcast offered bright clear concept
Hi, Neat post. There is a problem along with your website in web explorer, may test this? IE nonetheless is the marketplace chief and a huge component to people will leave out your great writing due to this problem.
Hello I am so glad I found your webpage, I really found you by accident, while I was browsing on Google for something else, Anyways I am here now and would just like to say kudos for a remarkable post and a all round enjoyable blog (I also love the theme/design), I don’t have time to go through it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the superb job.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
Its like you read my mind! You appear to know so much about this, like you wrote the book in it or something. I feel that you can do with some percent to drive the message home a little bit, but other than that, that is wonderful blog. A fantastic read. I’ll certainly be back.
My spouse and I stumbled over here coming from a different web address and thought I might check things out. I like what I see so now i am following you. Look forward to looking at your web page again.
Why visitors still make use of to read news papers when in this technological globe everything is presented on net?
Oh my goodness! Incredible article dude! Thanks, However I am having troubles with your RSS. I don’t know the reason why I am unable to subscribe to it. Is there anybody else having similar RSS issues? Anyone that knows the answer will you kindly respond? Thanks!!
Highly descriptive article, I loved that a lot. Will there be a part 2?
cialis tadalafil treat
cialis tadalafil treat
brand cialis trial pack
brand cialis trial pack
This piece of writing will help the internet viewers for building up new website or even a blog from start to end.
It’s perfect time to make some plans for the future and it’s time to be happy. I’ve read this post and if I could I desire to suggest you some interesting things or tips. Perhaps you could write next articles referring to this article. I want to read even more things about it!
Your style is really unique compared to other folks I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll just bookmark this blog.
Hi there friends, how is all, and what you would like to say on the topic of this post, in my view its really remarkable designed for me.
I’d like to find out more? I’d want to find out more details.
cialis with alcohol
I really like what you guys are usually up too. Such clever work and exposure! Keep up the terrific works guys I’ve incorporated you guys to my personal blogroll.
I’m curious to find out what blog system you happen to be using? I’m having some small security problems with my latest blog and I’d like to find something more secure. Do you have any solutions?
Wonderful blog! I found it while surfing around on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thanks
Its not my first time to go to see this web site, i am browsing this web site dailly and obtain pleasant data from here all the time.
This is the right site for everyone who wishes to understand this topic. You understand a whole lot its almost hard to argue with you (not that I actually will need to…HaHa). You definitely put a brand new spin on a subject that has been discussed for a long time. Excellent stuff, just wonderful!
I’m gone to inform my little brother, that he should also visit this blog on regular basis to take updated from hottest information.
Woah! I’m really loving the template/theme of this website. It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between usability and appearance. I must say you have done a superb job with this. In addition, the blog loads extremely quick for me on Internet explorer. Exceptional Blog!
cialis super active online pharmacy
cialis super active online pharmacy
Hurrah! In the end I got a webpage from where I know how to in fact obtain useful data regarding my study and knowledge.
legitimate viagra pharmacy
legitimate viagra pharmacy
My spouse and I absolutely love your blog and find a lot of your post’s to be exactly what I’m looking for. can you offer guest writers to write content for you? I wouldn’t mind writing a post or elaborating on a few of the subjects you write regarding here. Again, awesome blog!
Since the admin of this web site is working, no question very rapidly it will be famous, due to its quality contents.
what is tadalafil 20mg
I have read so many content concerning the blogger lovers however this paragraph is actually a pleasant post, keep it up.
I have been browsing online more than 3 hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. In my view, if all site owners and bloggers made good content as you did, the internet will be much more useful than ever before.
Hello, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam comments? If so how do you prevent it, any plugin or anything you can recommend? I get so much lately it’s driving me mad so any support is very much appreciated.
Ahaa, its pleasant discussion regarding this paragraph here at this weblog, I have read all that, so at this time me also commenting at this place.
Heya i’m for the first time here. I came across this board and I to find It really helpful & it helped me out much. I’m hoping to give one thing again and aid others like you helped me.
Have you ever considered publishing an ebook or guest authoring on other websites? I have a blog based on the same topics you discuss and would love to have you share some stories/information. I know my visitors would appreciate your work. If you are even remotely interested, feel free to shoot me an e mail.
viagra europe over the counter
viagra europe over the counter
cialis side effects with alcohol
cialis side effects with alcohol
sildenafil 25 mg price in india
sildenafil 25 mg price in india
walgreens cialis prices
walgreens cialis prices
I will immediately clutch your rss feed as I can’t find your e-mail subscription hyperlink or newsletter service. Do you’ve any? Kindly let me understand in order that I could subscribe. Thanks.
I know this if off topic but I’m looking into starting my own weblog and was wondering what all is needed to get set up? I’m assuming having a blog like yours would cost a pretty penny? I’m not very web smart so I’m not 100% certain. Any recommendations or advice would be greatly appreciated. Thanks
tadalafil price walmart
tadalafil price walmart
Flomax
buy xanax mexican pharmacy
buy xanax mexican pharmacy
Greetings from Colorado! I’m bored to death at work so I decided to check out your website on my iphone during lunch break. I love the information you provide here and can’t wait to take a look when I get home. I’m amazed at how quick your blog loaded on my phone .. I’m not even using WIFI, just 3G .. Anyhow, good site!
It’s difficult to find experienced people about this subject, but you sound like you know what you’re talking about! Thanks
Heya i’m for the first time here. I found this board and I find It truly useful & it helped me out much. I hope to give something back and help others like you aided me.
You actually make it seem so easy with your presentation but I find this topic to be actually something which I think I would never understand. It seems too complex and very broad for me. I am looking forward for your next post, I’ll try to get the hang of it!
I really like your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to create my own blog and would like to find out where u got this from. appreciate it
Very nice post. I just stumbled upon your weblog and wished to mention that I have really loved surfing around your weblog posts. After all I’ll be subscribing on your rss feed and I am hoping you write again soon!
Howdy would you mind sharing which blog platform you’re working with? I’m looking to start my own blog soon but I’m having a hard time making a decision between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design and style seems different then most blogs and I’m looking for something completely unique. P.S My apologies for being off-topic but I had to ask!
Wow, that’s what I was looking for, what a material! existing here at this blog, thanks admin of this web page.
Fantastic goods from you, man. I’ve remember your stuff prior to and you are just extremely magnificent. I actually like what you have acquired here, really like what you’re stating and the best way through which you are saying it. You are making it entertaining and you continue to take care of to stay it sensible. I can not wait to read far more from you. This is really a tremendous website.
What’s up to all, how is everything, I think every one is getting more from this web page, and your views are pleasant designed for new viewers.
Appreciating the commitment you put into your blog and detailed information you present. It’s great to come across a blog every once in a while that isn’t the same outdated rehashed information. Great read! I’ve bookmarked your site and I’m adding your RSS feeds to my Google account.
sildenafil 50 mg generic
Can I simply just say what a comfort to discover a person that actually knows what they’re talking about online. You actually realize how to bring an issue to light and make it important. More and more people should check this out and understand this side of your story. It’s surprising you are not more popular given that you surely possess the gift.
Heya i’m for the first time here. I found this board and I find It truly useful & it helped me out a lot. I hope to give something back and help others like you aided me.
I read this paragraph completely on the topic of the resemblance of most up-to-date and earlier technologies, it’s amazing article.
viagra how much does it cost
viagra how much does it cost
Superb blog you have here but I was wondering if you knew of any message boards that cover the same topics talked about in this article? I’d really like to be a part of group where I can get advice from other knowledgeable people that share the same interest. If you have any suggestions, please let me know. Many thanks!
Undeniably believe that which you stated. Your favorite reason seemed to be on the net the easiest thing to be aware of. I say to you, I certainly get irked while people think about worries that they just don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side-effects , people can take a signal. Will probably be back to get more. Thanks
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I wish to suggest you some interesting things or suggestions. Maybe you could write next articles referring to this article. I wish to read even more things about it!
can you purchase viagra over the counter in canada
Excellent post. I’m going through a few of these issues as well..
Hey there just wanted to give you a quick heads up. The text in your post seem to be running off the screen in Internet explorer. I’m not sure if this is a formatting issue or something to do with web browser compatibility but I figured I’d post to let you know. The layout look great though! Hope you get the problem solved soon. Cheers
Very nice article, exactly what I wanted to find.
My brother suggested I might like this website. He was totally right. This post actually made my day. You cann’t imagine simply how much time I had spent for this information! Thanks!
Great post.
Wow, wonderful blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your site is great, let alone the content!
This is a great tip particularly to those new to the blogosphere. Brief but very precise information… Many thanks for sharing this one. A must read post!
Asking questions are in fact fastidious thing if you are not understanding anything fully, however this paragraph offers fastidious understanding even.
I every time emailed this web site post page to all my friends, because if like to read it then my contacts will too.
cialis 200 mg.
Hi there, just became aware of your blog through Google, and found that it is truly informative. I am going to watch out for brussels. I will appreciate if you continue this in future. A lot of people will be benefited from your writing. Cheers!
tadalafil spray
viagra soft tabs canada
What’s up, I want to subscribe for this webpage to get most recent updates, thus where can i do it please assist.
Fantastic beat ! I wish to apprentice while you amend your website, how could i subscribe for a blog website? The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright clear idea
Hi! This is kind of off topic but I need some help from an established blog. Is it hard to set up your own blog? I’m not very techincal but I can figure things out pretty quick. I’m thinking about making my own but I’m not sure where to start. Do you have any points or suggestions? Thank you
what pharmacy has oxycodone in stock
My brother recommended I might like this website. He was totally right. This post actually made my day. You can not imagine simply how much time I had spent for this information! Thanks!
Greetings! This is my first comment here so I just wanted to give a quick shout out and say I really enjoy reading your blog posts. Can you recommend any other blogs/websites/forums that deal with the same topics? Appreciate it!
I blog frequently and I genuinely thank you for your content. This great article has really peaked my interest. I’m going to book mark your website and keep checking for new information about once per week. I subscribed to your Feed as well.
Hi all, here every one is sharing such know-how, therefore it’s pleasant to read this webpage, and I used to go to see this weblog daily.
I blog quite often and I seriously thank you for your content. This article has truly peaked my interest. I’m going to bookmark your blog and keep checking for new details about once per week. I subscribed to your RSS feed as well.
Greetings! Very helpful advice in this particular article! It’s the little changes that will make the most significant changes. Many thanks for sharing!
Why visitors still use to read news papers when in this technological globe everything is presented on web?
Amazing! Its truly awesome post, I have got much clear idea on the topic of from this paragraph.
Quality posts is the main to invite the viewers to pay a visit the website, that’s what this site is providing.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You definitely know what youre talking about, why waste your intelligence on just posting videos to your weblog when you could be giving us something enlightening to read?
I do not even know how I ended up here, but I thought this post was good. I don’t know who you are but certainly you’re going to a famous blogger if you are not already 😉 Cheers!
For hottest news you have to pay a quick visit world wide web and on internet I found this site as a finest web page for newest updates.
Thank you for sharing your thoughts. I truly appreciate your efforts and I will be waiting for your next write ups thanks once again.
buy generic viagra in usa
buy generic viagra in usa
cialis daily use
erectile dysfunction viagra
erectile dysfunction viagra
where can you buy viagra for women
where can you buy viagra for women
best online price for viagra
best online price for viagra
viagra over the counter mexico
viagra over the counter mexico
tadalafil herbal substitute
tadalafil herbal substitute
online prescription tadalafil
online prescription tadalafil
cialis 20 mg duration
cialis 20 mg duration
buy generic cialis paypal
buy generic cialis paypal
It’s very simple to find out any matter on net as compared to books, as I found this paragraph at this website.
Hey! Do you use Twitter? I’d like to follow you if that would be okay. I’m undoubtedly enjoying your blog and look forward to new updates.
Hello, yup this article is really pleasant and I have learned lot of things from it about blogging. thanks.
hello!,I really like your writing very much! share we keep up a correspondence more approximately your article on AOL? I need a specialist on this space to solve my problem. Maybe that is you! Looking forward to see you.
I loved as much as you’ll receive carried out right here. The sketch is tasteful, your authored material stylish. nonetheless, you command get got an impatience over that you wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this hike.
Hi there mates, its wonderful article on the topic of educationand entirely explained, keep it up all the time.
Howdy this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding expertise so I wanted to get guidance from someone with experience. Any help would be greatly appreciated!
Hey outstanding blog! Does running a blog similar to this take a large amount of work? I have no expertise in programming however I was hoping to start my own blog in the near future. Anyway, if you have any recommendations or techniques for new blog owners please share. I understand this is off subject nevertheless I just wanted to ask. Appreciate it!
My brother suggested I may like this website. He was totally right. This put up actually made my day. You can not believe simply how a lot time I had spent for this information! Thank you!
Yes! Finally someone writes about %keyword1%.
Your method of describing the whole thing in this paragraph is actually good, every one can effortlessly be aware of it, Thanks a lot.
Have you ever considered about adding a little bit more than just your articles? I mean, what you say is important and all. But think about if you added some great visuals or videos to give your posts more, “pop”! Your content is excellent but with pics and video clips, this website could certainly be one of the very best in its niche. Amazing blog!
When I originally commented I appear to have clicked on the -Notify me when new comments are added- checkbox and now every time a comment is added I get four emails with the same comment. Perhaps there is a means you are able to remove me from that service? Appreciate it!
I have been exploring for a little for any high-quality articles or weblog posts on this sort of space . Exploring in Yahoo I eventually stumbled upon this site. Reading this info So i’m glad to convey that I have an incredibly good uncanny feeling I found out just what I needed. I such a lot certainly will make sure to don?t omit this site and provides it a glance on a constant basis.
I like what you guys are usually up too. This type of clever work and reporting! Keep up the terrific works guys I’ve added you guys to our blogroll.
Great beat ! I wish to apprentice at the same time as you amend your web site, how can i subscribe for a blog website? The account aided me a acceptable deal. I had been tiny bit familiar of this your broadcast provided brilliant transparent idea
Remarkable! Its in fact awesome paragraph, I have got much clear idea about from this piece of writing.
Hi, everything is going fine here and ofcourse every one is sharing data, that’s truly fine, keep up writing.
Fastidious response in return of this matter with real arguments and explaining everything about that.
I constantly spent my half an hour to read this web site’s articles daily along with a cup of coffee.
I blog frequently and I truly thank you for your information. Your article has really peaked my interest. I’m going to take a note of your blog and keep checking for new details about once per week. I subscribed to your RSS feed as well.
Very good info. Lucky me I ran across your blog by chance (stumbleupon). I have saved as a favorite for later!
It’s in point of fact a nice and useful piece of info. I’m satisfied that you simply shared this useful information with us. Please keep us up to date like this. Thank you for sharing.
Hey There. I found your blog using msn. This is a really well written article. I will make sure to bookmark it and come back to read more of your useful information. Thanks for the post. I will certainly return.
I loved as much as you will receive carried out right here. The sketch is attractive, your authored material stylish. nonetheless, you command get got an edginess over that you wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly a lot often inside case you shield this hike.
Thanks for finally talking about > %blog_title% < Loved it!
Have you ever thought about creating an e-book or guest authoring on other blogs? I have a blog based on the same topics you discuss and would love to have you share some stories/information. I know my subscribers would appreciate your work. If you are even remotely interested, feel free to shoot me an e mail.
I enjoy reading through an article that can make men and women think. Also, thanks for permitting me to comment!
That is very fascinating, You are an overly professional blogger. I’ve joined your rss feed and sit up for in search of more of your wonderful post. Also, I have shared your site in my social networks
always i used to read smaller articles which as well clear their motive, and that is also happening with this paragraph which I am reading here.
I really love your website.. Great colors & theme. Did you develop this web site yourself? Please reply back as I’m wanting to create my very own website and would like to find out where you got this from or just what the theme is called. Thanks!
metronidazole pil
metronidazole pil
Amazing blog! Do you have any suggestions for aspiring writers? I’m planning to start my own blog soon but I’m a little lost on everything. Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m completely overwhelmed .. Any ideas? Thanks!
I love what you guys are usually up too. This type of clever work and reporting! Keep up the fantastic works guys I’ve added you guys to our blogroll.
sulfamethoxazole 800 trimeth 160mg
sulfamethoxazole 800 trimeth 160mg
I am not sure where you are getting your information, but great topic. I needs to spend some time learning more or understanding more. Thanks for magnificent info I was looking for this info for my mission.
tadalafil 20 mg best price
I think this is among the most important info for me. And i am glad reading your article. But wanna remark on some general things, The website style is perfect, the articles is really nice : D. Good job, cheers
Quality content is the crucial to interest the viewers to visit the website, that’s what this website is providing.
Terrific work! That is the kind of information that are supposed to be shared across the net. Shame on the seek engines for no longer positioning this submit higher! Come on over and talk over with my web site . Thanks =)
gabapentin sicherheitsdatenblatt
gabapentin sicherheitsdatenblatt
Hurrah, that’s what I was exploring for, what a data! existing here at this blog, thanks admin of this web site.
I’ll right away snatch your rss feed as I can’t find your e-mail subscription link or e-newsletter service. Do you’ve any? Kindly permit me recognise so that I may subscribe. Thanks.
Thank you for the auspicious writeup. It if truth be told used to be a amusement account it. Look complex to more brought agreeable from you! By the way, how could we be in contact?
I absolutely love your blog and find many of your post’s to be what precisely I’m looking for. Do you offer guest writers to write content for you? I wouldn’t mind creating a post or elaborating on most of the subjects you write in relation to here. Again, awesome blog!
tadalafil order online
Howdy! I’m at work browsing your blog from my new iphone 3gs! Just wanted to say I love reading through your blog and look forward to all your posts! Keep up the excellent work!
You ought to be a part of a contest for one of the highest quality websites on the web. I most certainly will highly recommend this web site!
Greetings from California! I’m bored at work so I decided to check out your website on my iphone during lunch break. I love the knowledge you present here and can’t wait to take a look when I get home. I’m surprised at how quick your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyhow, very good site!
valacyclovir neuropathy
valacyclovir neuropathy
what does lyrica feel like
what does lyrica feel like
Excellent post. Keep posting such kind of info on your blog. Im really impressed by it.
Hey there, You’ve done an incredible job. I’ll certainly digg it and individually suggest to my friends. I am confident they’ll be benefited from this website.
tamoxifen kreislauf
tamoxifen kreislauf
Wow that was strange. I just wrote an extremely long comment but after I clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say wonderful blog!
cialis max dose
Everyone loves what you guys are usually up too. Such clever work and exposure! Keep up the superb works guys I’ve added you guys to my own blogroll.
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three e-mails with the same comment. Is there any way you can remove people from that service? Thanks a lot!
metformin wirkungsverlust
metformin wirkungsverlust
lisinopril pronounce
lisinopril pronounce
Hiya very cool web site!! Guy .. Excellent .. Amazing .. I’ll bookmark your web site and take the feeds also? I’m happy to search out numerous useful information here within the post, we want develop more techniques in this regard, thank you for sharing. . . . . .
lasix szintigraphie
lasix szintigraphie
Great information. Lucky me I recently found your website by accident (stumbleupon). I’ve book-marked it for later!
I love looking through an article that can make people think. Also, thank you for allowing for me to comment!
Hi there! This is my 1st comment here so I just wanted to give a quick shout out and tell you I really enjoy reading your posts. Can you suggest any other blogs/websites/forums that go over the same topics? Thank you!
If you are going for finest contents like myself, simply pay a quick visit this web site every day because it presents quality contents, thanks
Hi! This post couldn’t be written any better! Reading this post reminds me of my good old room mate! He always kept chatting about this. I will forward this article to him. Fairly certain he will have a good read. Thank you for sharing!
tadalafil buy online
My brother recommended I may like this blog. He was entirely right. This submit actually made my day. You can not consider just how a lot time I had spent for this info! Thank you!
Piece of writing writing is also a excitement, if you be acquainted with afterward you can write otherwise it is complicated to write.
semaglutide qualifications
semaglutide qualifications
Wow, wonderful blog format! How lengthy have you been blogging for? you made blogging look easy. The full look of your website is excellent, as well as the content!
Please let me know if you’re looking for a article author for your weblog. You have some really great posts and I believe I would be a good asset. If you ever want to take some of the load off, I’d absolutely love to write some material for your blog in exchange for a link back to mine. Please blast me an email if interested. Thank you!
rybelsus every other day
rybelsus every other day
Hi colleagues, fastidious post and fastidious arguments commented at this place, I am in fact enjoying by these.
semaglutide titration schedule
semaglutide titration schedule
If some one needs to be updated with most recent technologies therefore he must be pay a visit this web site and be up to date everyday.
Now I am going away to do my breakfast, after having my breakfast coming yet again to read other news.
Its like you read my mind! You appear to understand a lot approximately this, such as you wrote the e-book in it or something. I think that you simply can do with a few p.c. to power the message home a little bit, but instead of that, this is great blog. An excellent read. I’ll certainly be back.
Aw, this was an extremely nice post. Finding the time and actual effort to produce a good article… but what can I say… I hesitate a whole lot and never manage to get anything done.
I love reading a post that will make men and women think. Also, thanks for allowing for me to comment!
Wow! After all I got a webpage from where I be capable of in fact get useful facts concerning my study and knowledge.
I am not sure where you’re getting your information, but good topic. I needs to spend some time learning more or understanding more. Thanks for wonderful information I was looking for this information for my mission.
Very nice post. I simply stumbled upon your blog and wanted to say that I’ve really enjoyed surfing around your weblog posts. In any case I’ll be subscribing for your feed and I am hoping you write once more soon!
In fact when someone doesn’t know after that its up to other visitors that they will help, so here it takes place.
Hi there, I enjoy reading through your article. I like to write a little comment to support you.
Hi this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get guidance from someone with experience. Any help would be enormously appreciated!
Hi there! I could have sworn I’ve been to this site before but after reading through some of the post I realized it’s new to me. Anyways, I’m definitely delighted I found it and I’ll be book-marking and checking back often!
An outstanding share! I have just forwarded this onto a co-worker who has been doing a little homework on this. And he actually ordered me dinner because I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanx for spending time to talk about this issue here on your internet site.
I love it when folks get together and share opinions. Great website, stick with it!
Very energetic blog, I enjoyed that bit. Will there be a part 2?
I love it when people get together and share opinions. Great site, stick with it!
It’s remarkable designed for me to have a website, which is beneficial in support of my know-how. thanks admin
Spot on with this write-up, I truly think this site needs a lot more attention. I’ll probably be returning to read through more, thanks for the advice!
Hi all, here every one is sharing these familiarity, therefore it’s pleasant to read this weblog, and I used to visit this blog everyday.
Hmm it seems like your site ate my first comment (it was extremely long) so I guess I’ll just sum it up what I had written and say, I’m thoroughly enjoying your blog. I too am an aspiring blog blogger but I’m still new to the whole thing. Do you have any helpful hints for newbie blog writers? I’d definitely appreciate it.
I like the helpful information you provide in your articles. I will bookmark your blog and check again here frequently. I’m quite sure I will learn many new stuff right here! Good luck for the next!
Hi there to every one, the contents existing at this web site are in fact awesome for people knowledge, well, keep up the good work fellows.
metronidazole hangover
I read this piece of writing fully concerning the difference of most recent and previous technologies, it’s remarkable article.
I think what you posted made a lot of sense. But, what about this? what if you typed a catchier post title? I am not suggesting your content is not solid., however what if you added a headline that makes people want more? I mean %BLOG_TITLE% is a little plain. You should look at Yahoo’s home page and note how they write news titles to get viewers to open the links. You might try adding a video or a related pic or two to grab readers interested about everything’ve written. In my opinion, it might make your website a little livelier.
Does your blog have a contact page? I’m having problems locating it but, I’d like to send you an e-mail. I’ve got some recommendations for your blog you might be interested in hearing. Either way, great blog and I look forward to seeing it develop over time.
I think the admin of this web page is actually working hard for his website, because here every material is quality based data.
Hi colleagues, its great article regarding cultureand fully explained, keep it up all the time.
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to your webpage? My blog is in the very same area of interest as yours and my visitors would certainly benefit from some of the information you provide here. Please let me know if this ok with you. Thanks a lot!
I feel this is among the so much important information for me. And i am satisfied reading your article. But wanna remark on few normal things, The website taste is great, the articles is really great : D. Good process, cheers
You should be a part of a contest for one of the most useful websites on the internet. I most certainly will highly recommend this site!
Hi there Dear, are you in fact visiting this website on a regular basis, if so afterward you will without doubt get nice experience.
What’s up, its nice post regarding media print, we all be familiar with media is a great source of facts.
Thanks for one’s marvelous posting! I certainly enjoyed reading it, you will be a great author.I will make certain to bookmark your blog and definitely will come back in the future. I want to encourage you to continue your great job, have a nice afternoon!
You really make it appear really easy along with your presentation however I in finding this matter to be actually something which I believe I might never understand. It sort of feels too complicated and extremely wide for me. I am taking a look forward in your next publish, I’ll try to get the hang of it!
I’ve been browsing on-line greater than three hours as of late, but I never discovered any interesting article like yours. It is beautiful value enough for me. In my view, if all web owners and bloggers made excellent content material as you probably did, the internet might be a lot more useful than ever before.
I am in fact glad to read this website posts which carries tons of useful information, thanks for providing these kinds of statistics.
I am sure this paragraph has touched all the internet users, its really really nice article on building up new website.
At this moment I am going to do my breakfast, after having my breakfast coming yet again to read further news.
You really make it appear really easy along with your presentation however I to find this topic to be actually one thing that I believe I’d by no means understand. It seems too complex and very wide for me. I’m having a look forward for your subsequent publish, I will try to get the hold of it!
What a stuff of un-ambiguity and preserveness of precious familiarity about unexpected feelings.
I just like the valuable info you provide on your articles. I’ll bookmark your blog and take a look at once more right here frequently. I’m somewhat certain I will be told lots of new stuff proper here! Good luck for the next!
Wow, superb weblog layout! How lengthy have you been blogging for? you made running a blog look easy. The entire glance of your web site is fantastic, let alone the content!
It is not my first time to visit this web page, i am visiting this web site dailly and take nice information from here all the time.
You really make it seem so easy with your presentation but I find this topic to be really something that I think I would never understand. It seems too complex and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
You can certainly see your skills in the work you write. The world hopes for even more passionate writers like you who aren’t afraid to say how they believe. All the time follow your heart.
Paragraph writing is also a fun, if you be familiar with then you can write if not it is difficult to write.
Remarkable issues here. I am very happy to look your post. Thank you a lot and I’m having a look forward to contact you. Will you kindly drop me a e-mail?
You are so cool! I do not believe I’ve read through a single thing like that before. So good to find another person with some unique thoughts on this subject. Really.. thank you for starting this up. This website is one thing that’s needed on the internet, someone with a little originality!
Wow that was unusual. I just wrote an very long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Anyways, just wanted to say superb blog!
Hi there! I’m at work browsing your blog from my new iphone! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the outstanding work!
This site was… how do I say it? Relevant!! Finally I have found something which helped me. Thank you!
Way cool! Some extremely valid points! I appreciate you penning this post and the rest of the website is extremely good.
What’s up to all, how is everything, I think every one is getting more from this web page, and your views are good for new users.
Howdy! This is kind of off topic but I need some help from an established blog. Is it very hard to set up your own blog? I’m not very techincal but I can figure things out pretty quick. I’m thinking about creating my own but I’m not sure where to start. Do you have any points or suggestions? Many thanks
Thanks to my father who told me concerning this blog, this webpage is in fact remarkable.
I really like your blog.. very nice colors & theme. Did you create this website yourself or did you hire someone to do it for you? Plz reply as I’m looking to design my own blog and would like to know where u got this from. thank you
Heya i am for the first time here. I came across this board and I find It truly useful & it helped me out much. I hope to give something back and help others like you aided me.
I was wondering if you ever thought of changing the page layout of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Please let me know if you’re looking for a author for your site. You have some really great articles and I believe I would be a good asset. If you ever want to take some of the load off, I’d love to write some content for your blog in exchange for a link back to mine. Please send me an e-mail if interested. Thank you!
Howdy! This post could not be written any better! Reading this post reminds me of my old room mate! He always kept chatting about this. I will forward this page to him. Pretty sure he will have a good read. Thanks for sharing!
Thanks for a marvelous posting! I actually enjoyed reading it, you happen to be a great author.I will always bookmark your blog and may come back very soon. I want to encourage you continue your great writing, have a nice weekend!
Wow, superb blog format! How lengthy have you been running a blog for? you made running a blog glance easy. The overall look of your web site is excellent, let alone the content material!
I feel this is one of the such a lot significant information for me. And i’m satisfied studying your article. However should commentary on some general issues, The website taste is wonderful, the articles is in reality excellent : D. Good activity, cheers
Yes! Finally something about %keyword1%.
This is a topic that is near to my heart… Take care! Where are your contact details though?
Hey! I know this is kinda off topic but I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog post or vice-versa? My blog discusses a lot of the same topics as yours and I believe we could greatly benefit from each other. If you are interested feel free to shoot me an email. I look forward to hearing from you! Awesome blog by the way!
I always spent my half an hour to read this blog’s content daily along with a cup of coffee.
Great blog! Do you have any recommendations for aspiring writers? I’m hoping to start my own blog soon but I’m a little lost on everything. Would you propose starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m completely confused .. Any recommendations? Thanks a lot!
Aw, this was an incredibly good post. Taking a few minutes and actual effort to produce a top notch article… but what can I say… I procrastinate a whole lot and don’t seem to get anything done.
I was able to find good information from your articles.
It’s actually a great and useful piece of info. I’m satisfied that you simply shared this useful info with us. Please keep us up to date like this. Thanks for sharing.
each time i used to read smaller posts which also clear their motive, and that is also happening with this article which I am reading at this time.
certainly like your web site but you need to test the spelling on quite a few of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth nevertheless I’ll certainly come again again.
Good day I am so grateful I found your blog, I really found you by mistake, while I was researching on Digg for something else, Anyways I am here now and would just like to say thanks a lot for a marvelous post and a all round entertaining blog (I also love the theme/design), I don’t have time to read it all at the minute but I have book-marked it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the fantastic work.
I am not sure where you are getting your information, but great topic. I needs to spend some time learning more or understanding more. Thanks for fantastic information I was looking for this info for my mission.
I’d like to find out more? I’d want to find out more details.
Heya! I’m at work browsing your blog from my new iphone! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the outstanding work!
I believe what you said was actually very logical. But, think on this, suppose you typed a catchier post title? I ain’t suggesting your content is not solid, however suppose you added a post title that makes people desire more? I mean %BLOG_TITLE% is a little plain. You ought to look at Yahoo’s home page and note how they create article titles to grab viewers to open the links. You might try adding a video or a related pic or two to grab readers excited about what you’ve got to say. Just my opinion, it might make your posts a little livelier.
Great beat ! I wish to apprentice while you amend your web site, how could i subscribe for a blog site? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear idea
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three e-mails with the same comment. Is there any way you can remove me from that service? Cheers!
Remarkable! Its in fact awesome post, I have got much clear idea on the topic of from this paragraph.
This paragraph is actually a fastidious one it helps new internet viewers, who are wishing in favor of blogging.
Excellent goods from you, man. I have understand your stuff previous to and you are just extremely wonderful. I actually like what you have acquired here, certainly like what you are saying and the way in which you say it. You make it enjoyable and you still take care of to keep it smart. I cant wait to read much more from you. This is really a wonderful site.
Greetings from Colorado! I’m bored to tears at work so I decided to check out your blog on my iphone during lunch break. I love the info you present here and can’t wait to take a look when I get home. I’m shocked at how fast your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyhow, awesome blog!
Hi there, i read your blog from time to time and i own a similar one and i was just wondering if you get a lot of spam comments? If so how do you stop it, any plugin or anything you can suggest? I get so much lately it’s driving me crazy so any help is very much appreciated.
you are actually a excellent webmaster. The site loading speed is incredible. It kind of feels that you’re doing any distinctive trick. Also, The contents are masterpiece. you have performed a wonderful job on this matter!
I believe that is among the most significant information for me. And i’m happy reading your article. But should remark on few normal issues, The web site style is perfect, the articles is truly great : D. Good process, cheers
I was recommended this web site by my cousin. I am not sure whether this post is written by him as nobody else know such detailed about my trouble. You are wonderful! Thanks!
Hello! I’ve been reading your site for some time now and finally got the courage to go ahead and give you a shout out from Atascocita Texas! Just wanted to say keep up the great job!
Hey! This is my 1st comment here so I just wanted to give a quick shout out and tell you I truly enjoy reading through your blog posts. Can you suggest any other blogs/websites/forums that deal with the same topics? Thanks a ton!
What’s up Dear, are you in fact visiting this website on a regular basis, if so then you will absolutely get fastidious knowledge.
I am really loving the theme/design of your blog. Do you ever run into any internet browser compatibility problems? A handful of my blog readers have complained about my blog not working correctly in Explorer but looks great in Safari. Do you have any solutions to help fix this problem?
Thanks for finally talking about > %blog_title% < Loved it!
If you would like to increase your familiarity just keep visiting this web page and be updated with the most recent information posted here.
Can I simply just say what a relief to find somebody who truly understands what they’re talking about on the internet. You definitely know how to bring a problem to light and make it important. More people have to check this out and understand this side of the story. I can’t believe you aren’t more popular given that you certainly possess the gift.
I’m pretty pleased to find this great site. I wanted to thank you for your time for this wonderful read!! I definitely really liked every bit of it and I have you saved to fav to look at new things in your web site.
Excellent blog here! Also your site loads up very fast! What web host are you using? Can I get your affiliate link to your host? I wish my site loaded up as quickly as yours lol
Thanks , I have recently been looking for info about this topic for a long time and yours is the greatest I’ve came upon so far. But, what in regards to the conclusion? Are you sure in regards to the source?
This is really interesting, You are a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your web site in my social networks!
Excellent goods from you, man. I have understand your stuff previous to and you are just too excellent. I actually like what you have acquired here, really like what you’re saying and the way in which you say it. You make it enjoyable and you still take care of to keep it smart. I can not wait to read much more from you. This is really a great site.
You can definitely see your enthusiasm within the article you write. The sector hopes for more passionate writers such as you who aren’t afraid to say how they believe. Always follow your heart.
Do you have a spam issue on this blog; I also am a blogger, and I was wondering your situation; we have developed some nice practices and we are looking to trade techniques with other folks, please shoot me an email if interested.
It’s awesome for me to have a website, which is useful for my know-how. thanks admin
Hi there! Would you mind if I share your blog with my myspace group? There’s a lot of people that I think would really appreciate your content. Please let me know. Thanks
Hey there! This is my first visit to your blog! We are a group of volunteers and starting a new project in a community in the same niche. Your blog provided us valuable information to work on. You have done a wonderful job!
I’m amazed, I have to admit. Seldom do I come across a blog that’s both educative and engaging, and let me tell you, you have hit the nail on the head. The issue is something that not enough folks are speaking intelligently about. I am very happy I stumbled across this in my search for something regarding this.
You ought to take part in a contest for one of the most useful sites online. I most certainly will highly recommend this site!
It’s in reality a nice and helpful piece of information. I am satisfied that you just shared this useful info with us. Please stay us up to date like this. Thank you for sharing.
Hey there! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Cheers!
I know this website offers quality depending articles or reviews and extra information, is there any other site which gives these stuff in quality?
Wonderful article! That is the type of info that are meant to be shared across the web. Shame on the search engines for not positioning this put up higher! Come on over and talk over with my web site . Thank you =)
Good day I am so grateful I found your site, I really found you by mistake, while I was searching on Google for something else, Anyways I am here now and would just like to say many thanks for a fantastic post and a all round exciting blog (I also love the theme/design), I don’t have time to browse it all at the moment but I have saved it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the fantastic work.
Woah! I’m really enjoying the template/theme of this site. It’s simple, yet effective. A lot of times it’s tough to get that “perfect balance” between user friendliness and appearance. I must say that you’ve done a great job with this. In addition, the blog loads super quick for me on Firefox. Exceptional Blog!
It’s really a nice and useful piece of info. I am satisfied that you just shared this useful information with us. Please stay us informed like this. Thank you for sharing.
Please let me know if you’re looking for a article author for your blog. You have some really great articles and I believe I would be a good asset. If you ever want to take some of the load off, I’d absolutely love to write some material for your blog in exchange for a link back to mine. Please send me an email if interested. Many thanks!
Nice blog here! Also your website loads up fast! What web host are you using? Can I get your affiliate link to your host? I wish my site loaded up as quickly as yours lol
What’s up, just wanted to tell you, I loved this blog post. It was helpful. Keep on posting!
My brother suggested I might like this blog. He was totally right. This post actually made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
You should be a part of a contest for one of the finest blogs on the internet. I’m going to recommend this site!
Aw, this was a really good post. Finding the time and actual effort to generate a very good article… but what can I say… I put things off a whole lot and never manage to get anything done.
Keep this going please, great job!
Great post. I was checking constantly this blog and I am impressed! Extremely helpful information particularly the final part 🙂 I handle such information a lot. I used to be seeking this particular information for a very long time. Thank you and best of luck.
If you desire to grow your knowledge only keep visiting this web site and be updated with the most up-to-date news posted here.
What i don’t understood is in truth how you’re now not actually a lot more smartly-appreciated than you may be now. You are so intelligent. You know thus significantly in the case of this topic, produced me for my part consider it from a lot of various angles. Its like women and men aren’t fascinated until it is one thing to do with Woman gaga! Your own stuffs outstanding. At all times deal with it up!
Wow, fantastic blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your site is magnificent, let alone the content!
Hi there, yeah this post is truly fastidious and I have learned lot of things from it on the topic of blogging. thanks.
Good answers in return of this issue with firm arguments and telling the whole thing about that.
Everything is very open with a really clear explanation of the challenges. It was really informative. Your website is very useful. Thank you for sharing!
I have read so many articles concerning the blogger lovers except this post is genuinely a fastidious article, keep it up.
This is my first time pay a visit at here and i am actually pleassant to read all at one place.
Hello to every one, it’s truly a good for me to pay a visit this web page, it includes important Information.
I blog often and I seriously appreciate your content. The article has truly peaked my interest. I will bookmark your blog and keep checking for new information about once per week. I opted in for your Feed as well.
you are truly a good webmaster. The website loading velocity is incredible. It sort of feels that you are doing any distinctive trick. Moreover, The contents are masterpiece. you have performed a excellent process on this subject!
Howdy excellent blog! Does running a blog similar to this take a great deal of work? I’ve virtually no expertise in programming but I was hoping to start my own blog soon. Anyhow, should you have any suggestions or tips for new blog owners please share. I know this is off topic but I simply had to ask. Thank you!
I think this is among the most vital information for me. And i’m glad reading your article. But should remark on few general things, The website style is ideal, the articles is really excellent : D. Good job, cheers
I’m amazed, I must say. Rarely do I encounter a blog that’s both equally educative and engaging, and without a doubt, you have hit the nail on the head. The issue is something that too few people are speaking intelligently about. I’m very happy that I stumbled across this during my hunt for something relating to this.
Good write-up. I certainly appreciate this website. Keep writing!
If some one wants to be updated with most up-to-date technologies afterward he must be visit this website and be up to date everyday.
Hi, constantly i used to check blog posts here in the early hours in the dawn, for the reason that i like to gain knowledge of more and more.
An outstanding share! I have just forwarded this onto a co-worker who was conducting a little homework on this. And he actually bought me breakfast due to the fact that I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending some time to talk about this subject here on your internet site.
Hi there, I enjoy reading all of your article post. I wanted to write a little comment to support you.
Hmm it seems like your website ate my first comment (it was super long) so I guess I’ll just sum it up what I wrote and say, I’m thoroughly enjoying your blog. I too am an aspiring blog writer but I’m still new to the whole thing. Do you have any helpful hints for first-time blog writers? I’d genuinely appreciate it.
Quality articles or reviews is the important to invite the viewers to visit the web site, that’s what this site is providing.
Everyone loves what you guys are up too. Such clever work and coverage! Keep up the excellent works guys I’ve included you guys to my own blogroll.
Good day I am so delighted I found your blog page, I really found you by mistake, while I was searching on Askjeeve for something else, Anyhow I am here now and would just like to say kudos for a fantastic post and a all round interesting blog (I also love the theme/design), I don’t have time to browse it all at the moment but I have saved it and also included your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the excellent job.
This is really interesting, You’re a very skilled blogger. I have joined your rss feed and look forward to seeking more of your magnificent post. Also, I have shared your web site in my social networks!
Thanks for ones marvelous posting! I really enjoyed reading it, you may be a great author. I will be sure to bookmark your blog and may come back from now on. I want to encourage you to continue your great work, have a nice weekend!
Wonderful post! We are linking to this great content on our website. Keep up the good writing.
Really no matter if someone doesn’t understand then its up to other visitors that they will help, so here it takes place.
Have you ever thought about writing an e-book or guest authoring on other sites? I have a blog centered on the same subjects you discuss and would really like to have you share some stories/information. I know my readers would enjoy your work. If you’re even remotely interested, feel free to shoot me an email.
This is a really good tip especially to those new to the blogosphere. Simple but very accurate info… Many thanks for sharing this one. A must read post!
Hello colleagues, how is all, and what you would like to say about this piece of writing, in my view its in fact remarkable in favor of me.
You could certainly see your enthusiasm within the article you write. The arena hopes for more passionate writers such as you who aren’t afraid to say how they believe. All the time follow your heart.
Pretty section of content. I just stumbled upon your weblog and in accession capital to assert that I get in fact enjoyed account your weblog posts. Any way I will be subscribing in your feeds or even I achievement you access consistently rapidly.
I enjoy what you guys tend to be up too. Such clever work and exposure! Keep up the good works guys I’ve incorporated you guys to my personal blogroll.
Hi there, yup this paragraph is really good and I have learned lot of things from it regarding blogging. thanks.
This paragraph is actually a pleasant one it assists new web visitors, who are wishing for blogging.
Thank you for some other informative website. The place else may I am getting that kind of info written in such a perfect approach? I have a venture that I am simply now running on, and I have been at the glance out for such information.
Informative article, exactly what I was looking for.
Heya i’m for the first time here. I came across this board and I find It really useful & it helped me out much. I hope to give something back and help others like you aided me.
Hi there, after reading this amazing post i am as well happy to share my familiarity here with friends.
At this moment I am going to do my breakfast, after having my breakfast coming over again to read further news.
I’m impressed, I have to admit. Seldom do I come across a blog that’s both equally educative and entertaining, and let me tell you, you have hit the nail on the head. The problem is something too few people are speaking intelligently about. I am very happy I came across this during my search for something relating to this.
Thank you for the auspicious writeup. It in truth used to be a leisure account it. Glance complex to more introduced agreeable from you! However, how could we keep up a correspondence?
Hi there! This is kind of off topic but I need some guidance from an established blog. Is it difficult to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about making my own but I’m not sure where to start. Do you have any points or suggestions? Cheers
I just couldn’t leave your site prior to suggesting that I extremely loved the usual information an individual supply for your guests? Is going to be again incessantly in order to check out new posts
Hi! I’ve been following your blog for a long time now and finally got the bravery to go ahead and give you a shout out from Porter Tx! Just wanted to tell you keep up the good work!
clonazepam and zoloft
clonazepam and zoloft
https://clck.ru/36EvyD
flagyl suppositorier
flagyl suppositorier
CUTE LITTLE GIRLS
==> s.yjm.pl/6N2Y s.yjm.pl/6N2Y <==
CUTE LITTLE GIRLS
gabapentin studies
gabapentin studies
max duloxetine dose
max duloxetine dose
does keflex make you sleepy
does keflex make you sleepy
https://clck.ru/36EvvJ
sertraline or fluoxetine
sertraline or fluoxetine
sildenafil 50 mg tablet cost
sildenafil 50 mg tablet cost
escitalopram 10mg price at kroger
escitalopram 10mg price at kroger
cymbalta abuse reddit
cymbalta abuse reddit
ashwagandha where can i buy it
Syktyvkar dating
dating site rating novosibirsk
lexapro and birth control
lexapro and birth control
cephalexin for gonorrhea
cephalexin for gonorrhea
can i eat bananas while taking lisinopril
stopping taking zoloft
dosage of furosemide for dogs
side effect of flagyl
Hellоǃ
Perhaps mу message іѕ toо spесifіс.
Βut my older ѕiѕtеr fоund а wоnderful mаn hеrе аnd thеy hаvе а great rеlatіonshіp, but what аbоut me?
I am 24 years old, Сathеrina, from thе Сzeсh Reрublic, knоw Еnglish lаnguаge alsо
And… bеtter to ѕаy іt immеdiаtely. I am biѕexuаl. I am not jеаlоuѕ оf another wоmаn… еѕpеciаlly іf wе make lоvе tоgеther.
Ah yеѕ, Ι cоok very tastу! and Ι lоvе not оnly cооk ;))
Im rеal gіrl and lооking fоr sеrіous аnd hot relationshіp…
Αnуwaу, уоu саn fіnd mу prоfіle here: https://1pt.co/hp1kp
gabapentin dosage for anxiety
dnp glucophage
lasix icd 10
birth control zithromax
amoxicillin penicillin allergy
gabapentin 600 mg used for
escitalopram brand
Hello, I’ll be brief. We sell activation keys for GSA Search Engine Ranker. On the official website it costs $130, our price is $65, decide quickly, there are only a few left! Visit our website: https://en.xrumerbasee.ru.
Also on sale are personal private databases for XRumer and fresh databases for GSA and XRumer.
P.S Since you are reading this, it means it (XRumer and my site contact database) is working, and traffic is flowing – I received 15,000 traffic and this is just the beginning.
can cephalexin be used for ear infection
can cephalexin be used for ear infection
cephalexin and breastfeeding side effects
what should i avoid while taking ciprofloxacin
what should i avoid while taking ciprofloxacin
ciprofloxacin 500 mg for sinus infection
will bactrim treat strep
will bactrim treat strep
can i give my cat bactrim ds 800-160
can i give my cat bactrim ds 800-160
bactrim for strep throat
very good
https://metamask-extension-4.gitbook.io/web3-browser-us/ MetaMask Chrome
does cephalexin treat kidney infection
amoxicillin covid
busty English real cams show with a fun and wild personality
does bactrim treat kidney infections
How to restore sound on a JVC LT-49C870(B) TV after disconnecting a surround sound system?
I have a JVC LT-49C870(B) TV that used to work with a surround sound system for six years. I recently removed the surround sound system and returned it to the owner. Since then, I have no sound output from the TV’s in-built speakers. I have checked the manual and the settings, but I cannot find the problem. I only use a Chromecast device to stream content, and the image quality is fine. Is there a simple solution to this issue? I appreciate any help.
https://technsight.com/
very interesting, but nothing sensible
I hand-me-down to living not far from the Jabalia and when nether regions mow down from firmament I was luckier than the people who lived there.
My monicker is مزيد‎., I am a refugee and I am raising loot to help.
Humour if you can send a dollar saved to a Bitcoin purse, do so. I liking have a stab to send funds looking for humanitarian backing to the victims in the Gaza Strip.
Bitcoin(BTC): bc1q4x8s3uw6gq67sakst5ngqcznznvwmzv8p6ktpr
Ethereum (ETH): 0xD236413ee5E9c1DBDdE2012595d4A3C38418C3bf
If you can’t send funds, choose don’t cut this message or send it to SPAM. Gladden impudent it to those who can send at least 1 dollar.
كنت أعيش في مكان ليس ببعيد عن Ш¬ШЁШ§Щ„ЩЉШ§، وعندما سقطت الجحيم من السماء كنت أكثر حظًا من الناس الذين يعيشون هناك.
اسمي مختار‎، أنا لاجئ وأقوم بجمع التبرعات للمساعدة.
من فضلك إذا كان بإمكانك إرسال الدولار الذي تدخره إلى محفظة بيتكوين، فافعل ذلك. سأحاول إرسال الأموال للمساعدات الإنسانية للضحايا في قطاع غزة.
Bitcoin(BTC): bc1q4x8s3uw6gq67sakst5ngqcznznvwmzv8p6ktpr
Ethereum (ETH): 0xD236413ee5E9c1DBDdE2012595d4A3C38418C3bf
إذا لم تتمكن من إرسال الأموال، يرجى عدم حذف هذه الرسالة أو إرسالها إلى الرسائل الاقتحامية. يرجى إرسالها إلى أولئك الذين يمكنهم إرسال دولار واحد على الأقل.
gabapentin for anxiety
escitaloprГЎm oxalate vs escitalopram
SWXVQBdKnglweU
depakote withdrawal
citalopram side effects sexually female
losartan cozaar 50 mg
ddavp melt bedwetting effects body
Мы предлагаем полный спектр услуг по ремонту дорожного покрытия – от устранения ям и трещин до полной перекладки асфальта.
Наши опытные специалисты используют только высококачественные материалы и современное оборудование, чтобы обеспечить
долговечность и прочность вашей дороги – ремонт дорог.
What’s up, always i used to check blog posts here early in the dawn, as i love to find out more and more.
It’s an amazing piece of writing for all the web users; they will get benefit from it I am sure.
Your method of telling everything in this article is really good, every one be capable of without difficulty understand it, Thanks a lot.
An outstanding share! I have just forwarded this onto a friend who had been conducting a little homework on this. And he actually ordered me breakfast simply because I discovered it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanx for spending some time to discuss this subject here on your site.
I love reading a post that will make men and women think. Also, thanks for allowing for me to comment!
Pretty nice post. I just stumbled upon your weblog and wanted to say that I’ve truly loved surfing around your blog posts. In any case I will be subscribing in your feed and I am hoping you write once more very soon!
I am regular visitor, how are you everybody? This paragraph posted at this web site is actually pleasant.
You’re so awesome! I don’t think I’ve truly read something like that before. So nice to discover somebody with some original thoughts on this subject matter. Seriously.. many thanks for starting this up. This website is something that’s needed on the internet, someone with a little originality!
Hi friends, how is everything, and what you desire to say regarding this article, in my view its actually awesome in favor of me.
Excellent weblog right here! Also your site rather a lot up very fast! What host are you using? Can I get your affiliate hyperlink to your host? I desire my site loaded up as fast as yours lol
Hi there, I desire to subscribe for this webpage to obtain newest updates, therefore where can i do it please help out.
I think everything said was actually very reasonable. But, what about this? what if you were to write a killer headline? I ain’t saying your content is not solid, however what if you added something to maybe grab people’s attention? I mean %BLOG_TITLE% is a little vanilla. You might peek at Yahoo’s home page and see how they write post headlines to get viewers interested. You might try adding a video or a picture or two to grab readers excited about what you’ve written. Just my opinion, it would bring your posts a little livelier.
Hi there! I know this is kinda off topic however , I’d figured I’d ask. Would you be interested in trading links or maybe guest writing a blog post or vice-versa? My blog covers a lot of the same topics as yours and I think we could greatly benefit from each other. If you happen to be interested feel free to shoot me an email. I look forward to hearing from you! Great blog by the way!
I am extremely impressed with your writing skills as well as with the layout on your weblog. Is this a paid theme or did you modify it yourself? Anyway keep up the excellent quality writing, it’s rare to see a great blog like this one these days.
This is my first time pay a visit at here and i am in fact impressed to read everthing at one place.
depakote uses
I was suggested this web site by my cousin. I am not sure whether this post is written by him as no one else know such detailed about my trouble. You’re incredible! Thanks!
Hello to every body, it’s my first visit of this website; this web site contains amazing and actually excellent stuff in support of visitors.
Thanks in support of sharing such a pleasant idea, post is pleasant, thats why i have read it entirely
It’s really a nice and useful piece of info. I am glad that you shared this useful info with us. Please stay us informed like this. Thanks for sharing.
Hi there just wanted to give you a brief heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same outcome.
what drug class is cozaar
You’ve made some decent points there. I looked on the internet to learn more about the issue and found most individuals will go along with your views on this site.
Hi there this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get guidance from someone with experience. Any help would be enormously appreciated!
Thank you a bunch for sharing this with all people you actually recognise what you are speaking about! Bookmarked. Kindly also consult with my website =). We may have a link trade agreement between us
It’s truly a great and helpful piece of info. I am satisfied that you simply shared this useful information with us. Please stay us up to date like this. Thank you for sharing.
Thanks for sharing such a fastidious thought, piece of writing is nice, thats why i have read it fully
Your way of explaining all in this piece of writing is really good, every one be capable of easily understand it, Thanks a lot.
stopping citalopram after 1 week
Thanks for sharing your thoughts about %meta_keyword%. Regards
what is desmopressin ddavp
Thiet ke noi that tan co dien, thi cong noi that, chung cu, biet thu, van phong Thiet ke nha tan co dien
Hello Dear, are you genuinely visiting this web page on a regular basis, if so then you will definitely get good experience.
You really make it appear really easy along with your presentation however I in finding this topic to be really one thing that I think I might never understand. It kind of feels too complicated and extremely wide for me. I am having a look forward for your subsequent post, I will attempt to get the cling of it!
Thanks for sharing such a pleasant opinion, article is nice, thats why i have read it fully
I think this is one of the most significant information for me. And i’m glad reading your article. But wanna remark on few general things, The website style is wonderful, the articles is really great : D. Good job, cheers
I was suggested this website by way of my cousin. I am now not sure whether this put up is written by way of him as no one else realize such special approximately my difficulty. You’re amazing! Thank you!
themirrornewstoday.com – The latest UK and World news, from Mirror Online. Find the best stories, opinion, pictures and video on the day’s events.
https://www.themirrornewstoday.com/
you are actually a just right webmaster. The web site loading speed is incredible. It kind of feels that you’re doing any unique trick. Furthermore, The contents are masterpiece. you have performed a great job on this topic!
Hey There. I discovered your blog the use of msn. This is a very well written article. I will make sure to bookmark it and come back to read more of your helpful info. Thank you for the post. I will definitely return.
This design is incredible! You most certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job. I really loved what you had to say, and more than that, how you presented it. Too cool!
Wow that was unusual. I just wrote an really long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say fantastic blog!
Touche. Outstanding arguments. Keep up the good effort.
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is completely off topic but I had to tell someone!
Really no matter if someone doesn’t be aware of after that its up to other viewers that they will help, so here it takes place.
Does your site have a contact page? I’m having problems locating it but, I’d like to shoot you an email. I’ve got some recommendations for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it improve over time.
diclofenac 1%
It’s in fact very complex in this active life to listen news on TV, so I just use world wide web for that purpose, and get the most up-to-date news.
Good blog post. I absolutely love this site. Thanks!
Attractive section of content. I just stumbled upon your web site and in accession capital to assert that I get in fact enjoyed account your blog posts. Any way I will be subscribing to your feeds and even I achievement you access consistently rapidly.
each time i used to read smaller articles that as well clear their motive, and that is also happening with this post which I am reading now.
Hey there exceptional website! Does running a blog like this take a large amount of work? I’ve absolutely no understanding of programming but I was hoping to start my own blog in the near future. Anyways, should you have any suggestions or tips for new blog owners please share. I understand this is off subject nevertheless I simply needed to ask. Kudos!
all the time i used to read smaller posts which also clear their motive, and that is also happening with this piece of writing which I am reading at this time.
Yesterday, while I was at work, my cousin stole my apple ipad and tested to see if it can survive a 25 foot drop, just so she can be a youtube sensation. My apple ipad is now broken and she has 83 views. I know this is completely off topic but I had to share it with someone!
Aw, this was an exceptionally nice post. Finding the time and actual effort to create a superb article… but what can I say… I hesitate a lot and don’t manage to get nearly anything done.
ezetimibe analysis
Post writing is also a fun, if you be acquainted with after that you can write or else it is complex to write.
is diltiazem an ace inhibitor
If you are going for most excellent contents like me, simply pay a visit this web page daily as it offers feature contents, thanks
This is the perfect website for anybody who would like to find out about this topic. You know a whole lot its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a topic that’s been written about for years. Wonderful stuff, just wonderful!
Thank you a lot for sharing this with all of us you really realize what you are talking about! Bookmarked. Kindly additionally talk over with my web site =). We may have a hyperlink exchange agreement between us
Hey! Do you know if they make any plugins to safeguard against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
Thank you for the good writeup. It in fact was a amusement account it. Look advanced to more added agreeable from you! However, how could we communicate?
I’m really impressed with your writing skills and also with the layout on your weblog. Is this a paid theme or did you customize it yourself? Anyway keep up the excellent quality writing, it is rare to see a nice blog like this one nowadays.
W dzisiejszym zglobalizowanym społeczeństwie, gdzie cyfrowa rzeczywistość staje się coraz bardziej powszechna, dokumenty kolekcjonerskie pełnią rolę nie tylko materialnych artefaktów, ale także strażników pamięci i dziedzictwa. Co sprawia, że te papierowe, czasem wiekowe przedmioty stają się przedmiotem pożądania dla kolekcjonerów? Jak ewoluowały przez lata i jaką rolę odgrywają w dzisiejszym świecie kolekcji?
Początki dokumentów kolekcjonerskich sięgają odległej przeszłości, kiedy to zapisywano ważne wydarzenia na papierze, skórze, czy kamiennej tablicy. Służyły one jako nośniki informacji, świadectwa własności czy też potwierdzenia transakcji. Z biegiem lat, niektóre z nich stały się nie tylko dokumentami, ale i dziełami sztuki, zdobiącymi zbiory pasjonatów historii i kultury.
Jednym z najbardziej cenionych dokumentów kolekcjonerskich są stare mapy geograficzne. Przekładają się one nie tylko na wartość kartograficzną, ale również na historyczne znaczenie. Mapa świata sprzed wieków to okno w przeszłość, które pozwala nam zobaczyć, jak postrzegano świat w dawnych czasach. To jednocześnie zapis zmieniających się granic, odkryć geograficznych i ewolucji społeczeństw.
Innym przykładem dokumentów kolekcjonerskich są stare listy, manuskrypty czy dokumenty autentyczne z ważnych wydarzeń historycznych. Kolekcjonerzy często poszukują rękopisów sławnych pisarzy, które nie tylko stanowią unikatowe dzieła, ale także odsłaniają proces twórczy i myślowy ich autorów.
Wraz z rozwojem technologii, dokumenty kolekcjonerskie przeszły metamorfozę. Obecnie, obok tradycyjnych papierowych dokumentów, coraz bardziej cenione są dokumenty cyfrowe. To mogą być np. unikatowe pliki dźwiękowe, fotografie czy też elektroniczne kopie ważnych dokumentów historycznych. Choć nie posiadają one fizycznej formy, ich wartość tkwi w unikalności i trwałości informacji, które przechowują.
czytaj wiecej https://dobreplastiki.com/pl/
how long does flexeril stay in your system
can flomax be opened
effexor starting dose
contrave medication
aripiprazole information
オンラインカジノはギャンブル愛好家の間でますます人気が高まっていますが、これは驚くべきことではありません。なぜなら、オンラインカジノは自宅からギャンブルを楽しむ機会を提供するからです。 オンライン カジノの主な利点の 1 つは、あらゆる好みや好みに合わせて利用できるゲームの幅広い選択肢です。
この記事では、オンラインカジノが提供する最高のゲームを見ていきます。
1. スロット (またはスロット マシン) は、おそらくオンライン カジノで最も人気のあるゲーム カテゴリです。 スロットは運に左右されるシンプルでエキサイティングなゲームです。 現代のスロットには、映画、漫画、コンピューター ゲームなど、さまざまなテーマがあります。
2. ルーレットは古典的な運ゲーで、運を試したい人に最適です。 ルーレットでは、プレーヤーは数字または色に賭け、その後ルーレットが回転します。 オンライン カジノで人気のあるルーレットのオプションには、ヨーロピアン ルーレット、アメリカン ルーレット、フレンチ ルーレットなどがあります xvideo nonke
3. ブラックジャックは、プレーヤーに運だけでなく、戦略的思考も要求されるカード ゲームです。 ゲームの目標は、21 ポイントを獲得するか、それを超えずにできるだけそれに近い数字を獲得することです。 ブラックジャックはオンライン カジノで最も人気のあるゲームの 1 つです。
4. ポーカーもまた、ギャンブル愛好家にとって真の挑戦となる人気のカード ゲームです。 オンライン カジノでは、テキサス ホールデム、オマハなど、さまざまなポーカー オプションを提供しています。
5. ビデオ ポーカーは、古典的なポーカーとスロット マシンを組み合わせたものです。 このゲームでは、プレイヤーは勝つために特定のカードの組み合わせを収集する必要があります。 ビデオ ポーカーを使用すると、プレーヤーはスキルと戦略を活用して勝つ可能性を高めることができます。
これは最高のオンライン カジノ ゲームのほんの一部であり、すべてのプレイヤーが自分の好みに合ったものを見つけることができます。 どのゲームを好むかに関係なく、オンライン カジノには常にすべてのプレイヤーにとって興味深くエキサイティングな何かが用意されています。 ギャンブルは楽しく楽しいものであるべきであることを忘れないでください。責任を持ってプレイし、運は常に味方であることを忘れないでください。
amitriptyline hcl
can i give my dog augmentin 875
can i give my dog augmentin 875
Nice weblog right here! Additionally your site so much up fast! What web host are you using? Can I get your affiliate hyperlink for your host? I want my web site loaded up as fast as yours lol
allopurinol during acute gout
Hey! Do you know if they make any plugins to safeguard against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
It’s truly very difficult in this full of activity life to listen news on TV, therefore I simply use the web for that purpose, and get the hottest news.
I do trust all the ideas you’ve presented on your post. They’re very convincing and can certainly work. Nonetheless, the posts are too quick for novices. May you please extend them a bit from subsequent time? Thank you for the post.
ibuprofen vs acetaminophen vs aspirin
I think the admin of this website is actually working hard in favor of his web page, as here every information is quality based material.
If some one desires expert view concerning running a blog then i propose him/her to pay a visit this website, Keep up the pleasant job.
Wow, wonderful blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your website is excellent, as well as the content!
If you want to improve your familiarity simply keep visiting this site and be updated with the most up-to-date gossip posted here.
I just could not leave your web site before suggesting that I extremely enjoyed the usual information an individual supply on your visitors? Is gonna be again frequently to inspect new posts
Thanks for sharing your thoughts. I really appreciate your efforts and I will be waiting for your further write ups thank you once again.
Awesome! Its really amazing article, I have got much clear idea about from this article.
You made some decent points there. I looked on the internet for more information about the issue and found most people will go along with your views on this site.
I love it whenever people come together and share ideas. Great website, stick with it!
I’m impressed, I have to admit. Seldom do I come across a blog that’s equally educative and interesting, and without a doubt, you have hit the nail on the head. The issue is something that not enough people are speaking intelligently about. I am very happy I stumbled across this in my search for something regarding this.
I do accept as true with all the ideas you’ve offered for your post. They’re very convincing and can definitely work. Nonetheless, the posts are too short for novices. May you please lengthen them a little from next time? Thanks for the post.
We stumbled over here from a different web page and thought I might check things out. I like what I see so now i am following you. Look forward to going over your web page again.
I love your blog.. very nice colors & theme. Did you create this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to create my own blog and would like to find out where u got this from. cheers
constantly i used to read smaller articles that also clear their motive, and that is also happening with this article which I am reading now.
I simply couldn’t go away your website prior to suggesting that I really loved the standard info a person supply in your guests? Is going to be back regularly in order to investigate cross-check new posts
Aw, this was a really nice post. Spending some time and actual effort to make a really good article… but what can I say… I hesitate a whole lot and never manage to get anything done.
Howdy are using WordPress for your site platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any html coding knowledge to make your own blog? Any help would be greatly appreciated!
Hi! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
I read this post fully regarding the comparison of hottest and preceding technologies, it’s amazing article.
Good day very cool blog!! Man .. Excellent .. Wonderful .. I will bookmark your blog and take the feeds also? I’m glad to search out so many useful info here within the post, we’d like develop extra techniques in this regard, thanks for sharing. . . . . .
I do not even know how I ended up here, but I thought this post was good. I don’t know who you are but certainly you’re going to a famous blogger if you are not already 😉 Cheers!
Hello very cool site!! Guy .. Beautiful .. Wonderful .. I’ll bookmark your blog and take the feeds additionally? I am happy to seek out a lot of helpful information here within the put up, we’d like work out more strategies in this regard, thank you for sharing. . . . . .
I’ll right away grab your rss as I can not find your e-mail subscription link or newsletter service. Do you’ve any? Please let me recognise so that I could subscribe. Thanks.
Undeniably believe that which you stated. Your favorite reason seemed to be on the internet the simplest thing to be aware of. I say to you, I certainly get irked while people think about worries that they just don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side-effects , people could take a signal. Will probably be back to get more. Thanks
Thanks for sharing your info. I truly appreciate your efforts and I am waiting for your further write ups thank you once again.
baclofen insomnia
Good way of describing, and fastidious article to get information on the topic of my presentation subject, which i am going to deliver in university.
Your means of describing everything in this article is genuinely pleasant, every one be able to easily understand it, Thanks a lot.
bupropion class
https://clck.ru/36Ew4i
It is actually a great and useful piece of info. I am happy that you simply shared this helpful information with us. Please keep us informed like this. Thank you for sharing.
An impressive share! I’ve just forwarded this onto a co-worker who was conducting a little research on this. And he actually ordered me lunch because I stumbled upon it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanx for spending the time to talk about this subject here on your web site.
This piece of writing gives clear idea in support of the new visitors of blogging, that really how to do blogging.
Thank you for the good writeup. It in fact was a amusement account it. Look advanced to more added agreeable from you! However, how can we communicate?
celebrex vs mobic
Во-первых, мы тут не для шуток, а дабы поднимать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать тебе не составит труда. Пальцы в спешке шевели, и баксов на твоем счету все больше.
А во-2-хhttps://primarie.halleykm.md/forum/124/anvelopeinchisinaumd-destinaia-ta-sigur-pentru-anvelope-i-accesorii-auto-de-calitate
, кто заявил, собственно что заработок не имеет возможности быть веселым? У нас царствует атмосфера, как на самом классном пикнике. Тут в том числе и заработок делается частью приключения. Забудь скучные таски, у нас все по-нашему!
Ну и естесственно, партнерство с нами – это, брат, как скидка в самом эксклюзивном клубе. Ты 1-ый узнаешь о горячих акциях, самых заманчивых услугах и получишь билет в мир анлимитного заработка. А мы для тебя не просто обещаем, а гарантируем!
И откровенно, не знаю, как можно протекать мимо такового кайфа. Ты собственно что, не пытаешься замерзнуть настоящим уличным боссом? На нашем сайте ты, брат, будешь как капитан собственного корабля, маневрируя в океане крутых задач. Твои деньги, твои правила!
Не будь неудачником, чувак! Забудь на тему нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Входи на наш сайт, дерзай и зарабатывай, как настоящий уличный браток. Здесь твое время пришло, чувак!
There is definately a lot to learn about this subject. I really like all of the points you made.
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get four emails with the same comment. Is there any way you can remove me from that service? Thank you!
This info is invaluable. When can I find out more?
augmentin 875/125
My brother recommended I might like this blog. He was entirely right. This post truly made my day. You cann’t imagine just how much time I had spent for this info! Thanks!
Excellent web site you have here.. It’s hard to find high quality writing like yours these days. I honestly appreciate individuals like you! Take care!!
Incredible! This blog looks just like my old one! It’s on a completely different topic but it has pretty much the same page layout and design. Excellent choice of colors!
Does your site have a contact page? I’m having a tough time locating it but, I’d like to shoot you an e-mail. I’ve got some ideas for your blog you might be interested in hearing. Either way, great blog and I look forward to seeing it improve over time.
My brother suggested I might like this website. He was totally right. This post truly made my day. You cann’t imagine simply how much time I had spent for this info! Thanks!
Very nice post. I simply stumbled upon your blog and wished to mention that I’ve truly loved browsing your weblog posts. In any case I’ll be subscribing on your feed and I am hoping you write again soon!
This blog was… how do I say it? Relevant!! Finally I have found something which helped me. Thank you!
Spot on with this write-up, I really feel this web site needs much more attention. I’ll probably be back again to see more, thanks for the advice!
Thanks for one’s marvelous posting! I certainly enjoyed reading it, you might be a great author. I will make certain to bookmark your blog and will eventually come back in the foreseeable future. I want to encourage one to continue your great work, have a nice afternoon!
Hi, I do think this is an excellent website. I stumbledupon it 😉 I’m going to revisit yet again since i have book-marked it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
Your style is so unique in comparison to other people I have read stuff from. I appreciate you for posting when you have the opportunity, Guess I will just bookmark this blog.
Can you tell us more about this? I’d like to find out more details.
Howdy I am so thrilled I found your blog, I really found you by error, while I was researching on Bing for something else, Nonetheless I am here now and would just like to say thanks for a fantastic post and a all round thrilling blog (I also love the theme/design), I don’t have time to read it all at the moment but I have saved it and also added your RSS feeds, so when I have time I will be back to read more, Please do keep up the awesome job.
ashwagandha powder for height
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You obviously know what youre talking about, why waste your intelligence on just posting videos to your weblog when you could be giving us something enlightening to read?
Pretty! This was a really wonderful post. Thanks for supplying these details.
snorting buspirone hcl
Wow! This blog looks exactly like my old one! It’s on a completely different topic but it has pretty much the same layout and design. Outstanding choice of colors!
What’s up, just wanted to tell you, I liked this article. It was helpful. Keep on posting!
Pretty component of content. I simply stumbled upon your site and in accession capital to say that I acquire actually enjoyed account your blog posts. Anyway I’ll be subscribing for your feeds or even I fulfillment you get admission to constantly fast.
Why visitors still make use of to read news papers when in this technological globe all is accessible on net?
celecoxib pronunciation
celecoxib pronunciation
I wanted to thank you for this very good read!! I absolutely loved every bit of it. I have got you book-marked to look at new things you post…
With havin so much written content do you ever run into any issues of plagorism or copyright violation? My website has a lot of completely unique content I’ve either authored myself or outsourced but it appears a lot of it is popping it up all over the web without my permission. Do you know any ways to help protect against content from being ripped off? I’d definitely appreciate it.
celecoxib package insert
Have you ever thought about adding a little bit more than just your articles? I mean, what you say is valuable and everything. But imagine if you added some great graphics or videos to give your posts more, “pop”! Your content is excellent but with images and videos, this site could definitely be one of the most beneficial in its field. Very good blog!
celexa
I think this is one of the most significant info for me. And i am glad reading your article. But wanna remark on few general things, The website style is perfect, the articles is really great : D. Good job, cheers
After going over a number of the blog posts on your blog, I seriously like your technique of writing a blog. I book marked it to my bookmark site list and will be checking back in the near future. Please check out my website too and let me know your opinion.
Hello, I want to subscribe for this webpage to take most up-to-date updates, so where can i do it please help.
obviously like your website however you have to test the spelling on several of your posts. A number of them are rife with spelling problems and I to find it very bothersome to tell the truth nevertheless I will surely come again again.
Thanks for another informative web site. Where else could I get that kind of info written in such a perfect way? I’ve a venture that I’m just now operating on, and I have been at the glance out for such information.
Awesome! Its in fact awesome post, I have got much clear idea about from this post.
I always used to read paragraph in news papers but now as I am a user of web therefore from now I am using net for posts, thanks to web.
Hey there, You have done a great job. I’ll definitely digg it and personally suggest to my friends. I’m confident they will be benefited from this web site.
I’d like to find out more? I’d want to find out more details.
I loved as much as you’ll receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get got an edginess over that you wish be delivering the following. unwell unquestionably come more formerly again as exactly the same nearly very often inside case you shield this increase.
I all the time used to read paragraph in news papers but now as I am a user of internet so from now I am using net for content, thanks to web.
I think the admin of this web site is really working hard in favor of his web page, because here every information is quality based information.
Hi! Do you use Twitter? I’d like to follow you if that would be ok. I’m definitely enjoying your blog and look forward to new updates.
I’d like to find out more? I’d want to find out some additional information.
Hi there, You’ve done a great job. I’ll definitely digg it and personally recommend to my friends. I’m confident they will be benefited from this website.
Thanks for another informative site. Where else could I get that kind of information written in such a perfect means? I’ve a project that I am just now running on, and I’ve been at the look out for such information.
You actually make it seem so easy with your presentation but I find this matter to be really something that I think I would never understand. It seems too complex and extremely broad for me. I’m looking forward for your next post, I will try to get the hang of it!
I’m really loving the theme/design of your web site. Do you ever run into any internet browser compatibility problems? A handful of my blog audience have complained about my blog not operating correctly in Explorer but looks great in Chrome. Do you have any advice to help fix this problem?
Hi there! This post couldn’t be written any better! Reading through this post reminds me of my previous room mate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Many thanks for sharing!
It’s amazing to visit this site and reading the views of all mates regarding this paragraph, while I am also eager of getting experience.
Can you tell us more about this? I’d care to find out some additional information.
This info is invaluable. How can I find out more?
It is not my first time to visit this site, i am visiting this web site dailly and get fastidious information from here every day.
I know this web page provides quality dependent articles and other material, is there any other web page which provides these data in quality?
semaglutide max dose
Thanks for sharing such a nice thinking, paragraph is good, thats why i have read it fully
Hi there, I enjoy reading all of your article post. I like to write a little comment to support you.
abilify and pregnancy
Do you have a spam issue on this website; I also am a blogger, and I was curious about your situation; many of us have created some nice practices and we are looking to exchange techniques with others, be sure to shoot me an email if interested.
Wow, amazing blog structure! How long have you been blogging for? you make blogging glance easy. The overall look of your website is wonderful, as smartly as the content material!
actos infertility
bayer acarbose
I like it when individuals get together and share opinions. Great website, keep it up!
Very good article! We will be linking to this particularly great content on our site. Keep up the good writing.
A motivating discussion is definitely worth comment. I do believe that you should write more about this subject matter, it may not be a taboo subject but generally people do not discuss such topics. To the next! Many thanks!!
There’s certainly a great deal to know about this topic. I really like all of the points you made.
Thanks for sharing your thoughts on %meta_keyword%. Regards
I do accept as true with all the ideas you’ve offered on your post. They are really convincing and will definitely work. Still, the posts are very brief for novices. Could you please extend them a little from next time? Thanks for the post.
In today’s ever-changing world, remaining updated is essential. Whether it’s new discoveries or deep insights, our content aims to educate and motivate readers worldwide. We are dedicated to delivering reliable information that makes a difference. From innovative solutions to cultural phenomena, we cover a broad spectrum of topics to fuel your interests. Join us as we explore the issues that matter, presented by experts in the field. Your journey to greater knowledge begins here. Stay informed with us, and find the world around you. credit cards online casino
Hi, i feel that i noticed you visited my web site thus i got here to go back the want?.I’m attempting to to find things to improve my site!I suppose its good enough to make use of a few of your ideas!!
Good info. Lucky me I came across your website by chance (stumbleupon). I’ve book marked it for later!
I was more than happy to find this site. I want to to thank you for ones time for this particularly fantastic read!! I definitely savored every bit of it and I have you bookmarked to check out new stuff in your web site.
You are so cool! I do not think I’ve truly read through a single thing like this before. So good to find somebody with genuine thoughts on this subject. Seriously.. thank you for starting this up. This site is something that is needed on the web, someone with a bit of originality!
It’s an amazing piece of writing designed for all the internet visitors; they will obtain advantage from it I am sure.
Appreciating the time and effort you put into your site and detailed information you offer. It’s great to come across a blog every once in a while that isn’t the same old rehashed material. Fantastic read! I’ve saved your site and I’m including your RSS feeds to my Google account.
I’m truly enjoying the design and layout of your site. It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a designer to create your theme? Great work!
I am regular visitor, how are you everybody? This post posted at this web page is truly fastidious.
Excellent website you have here but I was wanting to know if you knew of any community forums that cover the same topics talked about here? I’d really love to be a part of online community where I can get feed-back from other knowledgeable people that share the same interest. If you have any recommendations, please let me know. Kudos!
is robaxin habit forming
repaglinide uv absorbance
Howdy! This post couldn’t be written much better! Looking through this article reminds me of my previous roommate! He continually kept talking about this. I will send this article to him. Fairly certain he will have a very good read. I appreciate you for sharing!
What i don’t realize is in reality how you’re no longer really a lot more neatly-preferred than you may be right now. You’re very intelligent. You recognize therefore considerably in terms of this subject, produced me for my part imagine it from so many varied angles. Its like men and women are not fascinated until it is something to do with Woman gaga! Your personal stuffs nice. Always handle it up!
I was wondering if you ever considered changing the page layout of your website? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or 2 pictures. Maybe you could space it out better?
remeron 30 mg
It’s really a cool and helpful piece of information. I’m satisfied that you simply shared this useful info with us. Please stay us informed like this. Thanks for sharing.
protonix otc
This design is incredible! You certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent job. I really loved what you had to say, and more than that, how you presented it. Too cool!
I go to see daily a few web sites and information sites to read articles or reviews, but this blog gives quality based articles.
Hi there, after reading this awesome piece of writing i am as well happy to share my knowledge here with colleagues.
Nice replies in return of this issue with genuine arguments and explaining all on the topic of that.
I really like what you guys tend to be up too. This kind of clever work and coverage! Keep up the excellent works guys I’ve added you guys to my own blogroll.
Please let me know if you’re looking for a article author for your weblog. You have some really good articles and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some articles for your blog in exchange for a link back to mine. Please send me an email if interested. Cheers!
Great work! This is the kind of info that should be shared around the internet. Disgrace on the search engines for not positioning this post upper! Come on over and talk over with my website . Thank you =)
Hi there, all is going perfectly here and ofcourse every one is sharing information, that’s in fact fine, keep up writing.
Heya! I know this is somewhat off-topic however I needed to ask. Does running a well-established website like yours require a large amount of work? I am brand new to writing a blog but I do write in my diary on a daily basis. I’d like to start a blog so I can share my experience and thoughts online. Please let me know if you have any suggestions or tips for brand new aspiring blog owners. Appreciate it!
Hey There. I found your blog using msn. This is a very well written article. I’ll be sure to bookmark it and come back to read more of your useful info. Thanks for the post. I will definitely return.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You obviously know what youre talking about, why waste your intelligence on just posting videos to your site when you could be giving us something informative to read?
Heya! I just wanted to ask if you ever have any trouble with hackers? My last blog (wordpress) was hacked and I ended up losing a few months of hard work due to no data backup. Do you have any methods to protect against hackers?
This is a topic which is close to my heart… Thank you! Where are your contact details though?
Great article! This is the kind of information that are meant to be shared across the net. Disgrace on the seek engines for not positioning this put up upper! Come on over and discuss with my site . Thanks =)
Woah! I’m really enjoying the template/theme of this site. It’s simple, yet effective. A lot of times it’s tough to get that “perfect balance” between user friendliness and visual appeal. I must say you’ve done a superb job with this. Also, the blog loads very fast for me on Internet explorer. Excellent Blog!
This page certainly has all of the info I needed concerning this subject and didn’t know who to ask.
What’s up, just wanted to say, I liked this blog post. It was inspiring. Keep on posting!
Hello there, just became aware of your blog through Google, and found that it is really informative. I am going to watch out for brussels. I will appreciate if you continue this in future. Lots of people will be benefited from your writing. Cheers!
A person necessarily lend a hand to make critically articles I would state. That is the very first time I frequented your website page and thus far? I surprised with the analysis you made to create this particular post incredible. Fantastic process!
Hi! This is my first visit to your blog! We are a collection of volunteers and starting a new project in a community in the same niche. Your blog provided us valuable information to work on. You have done a wonderful job!
Appreciate the recommendation. Will try it out.
I am actually thankful to the owner of this website who has shared this wonderful article at at this place.
Hi fantastic blog! Does running a blog similar to this require a massive amount work? I’ve no understanding of computer programming however I was hoping to start my own blog in the near future. Anyways, should you have any ideas or techniques for new blog owners please share. I understand this is off subject nevertheless I just needed to ask. Kudos!
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is completely off topic but I had to tell someone!
When I first heard about Bitcoin, I thought it was impossible. How can you have a purely digital currency? Can’t I just copy your hard drive and have your bitcoins? I didn’t understand how that could be done, and then I looked into it and it was brilliant.– Jeff Garzik https://cutt.ly/pwBLE09s
My partner and I absolutely love your blog and find many of your post’s to be exactly I’m looking for. Does one offer guest writers to write content in your case? I wouldn’t mind producing a post or elaborating on some of the subjects you write with regards to here. Again, awesome web log!
Thank you for the good writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! However, how can we communicate?
robaxin 500mg side effects
What i do not understood is if truth be told how you are now not actually a lot more well-preferred than you might be now. You’re very intelligent. You recognize therefore considerably on the subject of this matter, made me in my view believe it from numerous numerous angles. Its like men and women aren’t interested until it is one thing to do with Girl gaga! Your own stuffs great. Always take care of it up!
Thanks for finally writing about > %blog_title% < Liked it!
I was genuinely itching to get some wager some well-to-do on some sports matches that are circumstance right now. I wanted to allow in you guys know that I did twig what I reckon with to be the best locate in the USA.
If you destitution to bring back in on the engagement, scrutinize it out-moded: casino games online
When some one searches for his vital thing, therefore he/she wants to be available that in detail, so that thing is maintained over here.
vertigo spironolactone
It’s fantastic that you are getting ideas from this paragraph as well as from our argument made at this time.
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three emails with the same comment. Is there any way you can remove people from that service? Bless you!
sitagliptin 471
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You clearly know what youre talking about, why waste your intelligence on just posting videos to your blog when you could be giving us something informative to read?
Pretty nice post. I simply stumbled upon your blog and wished to mention that I’ve truly enjoyed browsing your weblog posts. In any case I’ll be subscribing on your feed and I’m hoping you write again very soon!
Хотите создать идеальное покрытие для вашего участка или дорожного покрытия? Тогда щебень фракции 5-70 идеально подойдет для вас!
Наш высококачественный щебень обеспечит прочность, долговечность и надежность вашего покрытия. Благодаря правильной фракции 5-70 мм,
он обладает отличной укладываемостью и прекрасно дренирует воду, что делает его идеальным выбором для любых работ – купить щебень.
Fullhdfilmizlesene ile en yeni vizyon filmler Full HD ve ücretsiz film sizlerle. Orijinal film arşivimizle en kaliteli film izle fırsatı sunuyoruz. Lanny Rowley
This post is truly a good one it assists new net viewers, who are wishing for blogging.
I have been browsing online greater than 3 hours these days, but I by no means discovered any interesting article like yours. It is pretty worth sufficient for me. In my view, if all site owners and bloggers made excellent content as you did, the net might be a lot more helpful than ever before.
What’s up to all, how is all, I think every one is getting more from this site, and your views are good for new users.
Terrific article! This is the kind of information that should be shared across the net. Disgrace on the seek engines for now not positioning this publish higher! Come on over and seek advice from my website . Thanks =)
I enjoy, cause I discovered exactly what I was taking a look for. You have ended my four day long hunt! God Bless you man. Have a great day. Bye
Howdy! I could have sworn I’ve been to this site before but after checking through some of the post I realized it’s new to me. Nonetheless, I’m definitely glad I found it and I’ll be book-marking and checking back often!
Hello, i feel that i saw you visited my site thus i came to return the want?.I’m attempting to find things to enhance my website!I assume its good enough to make use of some of your ideas!!
Excellent article. I absolutely love this site. Continue the good work!
This page truly has all the information and facts I needed about this subject and didn’t know who to ask.
Hi there! Someone in my Facebook group shared this website with us so I came to look it over. I’m definitely loving the information. I’m book-marking and will be tweeting this to my followers! Great blog and brilliant design.
voltaren gel topical
It’s enormous that you are getting ideas from this paragraph as well as from our discussion made here.
Very energetic article, I enjoyed that bit. Will there be a part 2?
sandoz-tamsulosin 0.4 mg side effects
What’s Going down i am new to this, I stumbled upon this I’ve found It absolutely useful and it has aided me out loads. I’m hoping to contribute & help other users like its helped me. Good job.
tizanidine blood pressure
Whats up this is kind of of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding experience so I wanted to get guidance from someone with experience. Any help would be greatly appreciated!
Hello! I could have sworn I’ve been to this blog before but after reading through some of the post I realized it’s new to me. Nonetheless, I’m definitely delighted I found it and I’ll be book-marking and checking back often!
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed surfing around your blog posts. After all I will be subscribing to your feed and I hope you write again soon!
Hello i am kavin, its my first occasion to commenting anywhere, when i read this article i thought i could also create comment due to this brilliant article.
Fine way of telling, and good post to get facts concerning my presentation subject matter, which i am going to deliver in academy.
I could not refrain from commenting. Very well written!
Hello! I simply want to offer you a huge thumbs up for your excellent information you’ve got here on this post. I will be coming back to your site for more soon.
Howdy! This is my first comment here so I just wanted to give a quick shout out and tell you I really enjoy reading through your blog posts. Can you suggest any other blogs/websites/forums that cover the same subjects? Thanks!
zetia coupon printable
I’d like to find out more? I’d want to find out more details.
Hi everyone, it’s my first go to see at this site, and article is genuinely fruitful in support of me, keep up posting such posts.
ivermectin 50ml
ivermectin 50ml
seroquel vs zyprexa
Pretty great post. I simply stumbled upon your weblog and wanted to say that I’ve really loved browsing your weblog posts. After all I’ll be subscribing for your feed and I am hoping you write once more soon!
It’s an awesome article designed for all the online users; they will take advantage from it I am sure.
zofran patent
synthroid osteoarthritis
synthroid osteoarthritis
It’s appropriate time to make a few plans for the future and it is time to be happy. I’ve read this put up and if I may I wish to recommend you some attention-grabbing issues or suggestions. Maybe you can write subsequent articles regarding this article. I desire to read even more issues approximately it!
Having read this I thought it was rather enlightening. I appreciate you spending some time and energy to put this content together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worth it!
Hi friends, pleasant piece of writing and good arguments commented at this place, I am truly enjoying by these.
Incredible points. Sound arguments. Keep up the good spirit.
An interesting discussion is definitely worth comment. I do think that you should publish more on this subject, it might not be a taboo matter but typically people don’t speak about these issues. To the next! Cheers!!
Good day! I know this is kinda off topic but I’d figured I’d ask. Would you be interested in exchanging links or maybe guest authoring a blog article or vice-versa? My website discusses a lot of the same subjects as yours and I feel we could greatly benefit from each other. If you might be interested feel free to shoot me an e-mail. I look forward to hearing from you! Terrific blog by the way!
Excellent post. I was checking constantly this blog and I am inspired! Very useful info specifically the last section 🙂 I maintain such info much. I used to be seeking this certain info for a very long time. Thank you and good luck.
what is venlafaxine hcl er used for
what is venlafaxine hcl er used for
Magnificent site. A lot of helpful information here. I’m sending it to a few buddies ans additionally sharing in delicious. And of course, thank you on your effort!
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
zyprexa images
maximum dosage zofran
Во-1-х, мы здесь не для шуток, а дабы подымать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать тебе не составит труда. Пальцы в горячке шевели, и баксов на твоем счету больше.
А во-вторыхhttps://moldova1359.md/photo/25/
, кто сказал, собственно что доход не может быть веселым? У нас царствует атмосфера, как на самом потрясающем пикнике. Тут даже заработок становится частью приключения. Забудь скучные таски, у нас все по-нашему!
Ну и конечно, партнерство с нами – это, брат, как скидка в самом эксклюзивном клубе. Ты 1-ый узнаешь о страстных акциях, самых радужных услугах и получишь билет в мир анлимитного заработка. А мы тебе не просто обещаем, а гарантируем!
И откровенно, не знаю, как можно протекать мимо такового кайфа. Ты что, не хочешь стать подлинным уличным боссом? На нашем сайте ты, брат, будешь как капитан своего корабля, маневрируя в океане крутых задач. Твои средства, твои правила!
Не будь неудачником, чувак! Забудь про нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Входи на наш вебсайт, дерзай и зарабатывай, как реальный уличный браток. Здесь твое время пришло, чувак!
Wow, this post is nice, my younger sister is analyzing these things, thus I am going to tell her.
I quite like reading an article that will make people think. Also, thanks for allowing for me to comment!
Thank you for the good writeup. It in fact was once a amusement account it. Glance advanced to more delivered agreeable from you! However, how could we communicate?
Good day! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
I don’t know if it’s just me or if everyone else experiencing problems with your website. It appears as though some of the text in your content are running off the screen. Can somebody else please provide feedback and let me know if this is happening to them as well? This might be a problem with my internet browser because I’ve had this happen previously. Thanks
Ahaa, its good discussion regarding this article at this place at this web site, I have read all that, so now me also commenting here.
I was in reality itching to get some wager some money on some sports matches that are circumstance above-board now. I wanted to say you guys recall that I did find what I reckon with to be the best locate in the USA.
If you poverty to bring back in on the action, verify it out-moded: Check this out
You actually make it seem so easy with your presentation but I find this matter to be really something which I think I would never understand. It seems too complex and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
Thanks for sharing such a nice thinking, post is fastidious, thats why i have read it entirely
There’s certainly a lot to find out about this topic. I love all the points you made.
I used to be able to find good advice from your articles.
Hi, the whole thing is going perfectly here and ofcourse every one is sharing facts, that’s in fact excellent, keep up writing.
I don’t even know how I ended up here, but I thought this post was great. I do not know who you are but certainly you are going to a famous blogger if you are not already 😉 Cheers!
Moz Group Buy has been a game-changer for my SEO strategy.
Its low cost access to premium software have given my site an edge in the market.
The information gained from the tools is invaluable,
and the cost-sharing model is a must-have for anyone who
is a digital marketer. Highly recommend for
optimizing digital presence but not exceeding the bank!
This post is invaluable. How can I find out more?
It’s actually a cool and helpful piece of info. I am happy that you shared this useful information with us. Please stay us informed like this. Thank you for sharing.
It’s the best time to make some plans for the long run and it is time to be happy. I have read this post and if I could I desire to suggest you few fascinating things or suggestions. Maybe you could write subsequent articles relating to this article. I wish to read even more issues about it!
Its like you learn my mind! You appear to know a lot about this, like you wrote the guide in it or something. I think that you just can do with a few % to drive the message house a bit, however instead of that, this is wonderful blog. An excellent read. I’ll certainly be back.
Hi there! I simply want to give you a huge thumbs up for your great info you have here on this post. I am coming back to your blog for more soon.
I’m not sure exactly why but this web site is loading very slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later on and see if the problem still exists.
Tremendous things here. I am very happy to peer your post. Thanks a lot and I’m looking ahead to touch you. Will you please drop me a e-mail?
I absolutely love your website.. Very nice colors & theme. Did you build this site yourself? Please reply back as I’m planning to create my own site and would love to find out where you got this from or what the theme is called. Thanks!
cheapest levitra online
Hi there! This post could not be written any better! Reading this post reminds me of my good old room mate! He always kept talking about this. I will forward this article to him. Fairly certain he will have a good read. Many thanks for sharing!
I like looking through an article that can make men and women think. Also, many thanks for allowing for me to comment!
viagra vs levitra
I got this web page from my friend who informed me on the topic of this web site and at the moment this time I am visiting this site and reading very informative content at this place.
cialis otc switch
My partner and I stumbled over here by a different web address and thought I may as well check things out. I like what I see so i am just following you. Look forward to looking into your web page for a second time.
tadalafil online india
I am really impressed together with your writing skills and also with the format on your blog. Is that this a paid subject matter or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to peer a great blog like this one nowadays..
It’s fantastic that you are getting thoughts from this post as well as from our discussion made at this place.
Very good article. I’m experiencing some of these issues as well..
Hello mates, good article and fastidious urging commented at this place, I am really enjoying by these.
Aw, this was a really nice post. Taking a few minutes and actual effort to generate a very good article… but what can I say… I procrastinate a whole lot and don’t seem to get nearly anything done.
Definitely believe that which you said. Your favorite reason appeared to be on the internet the simplest thing to be aware of. I say to you, I certainly get irked while people consider worries that they just don’t know about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
Greate pieces. Keep writing such kind of info on your blog. Im really impressed by it.
Hey there, You have done an excellent job. I’ll definitely digg it and in my view recommend to my friends. I am sure they will be benefited from this site.
Good day I am so glad I found your website, I really found you by mistake, while I was looking on Google for something else, Nonetheless I am here now and would just like to say thanks for a tremendous post and a all round enjoyable blog (I also love the theme/design), I don’t have time to browse it all at the moment but I have book-marked it and also included your RSS feeds, so when I have time I will be back to read much more, Please do keep up the fantastic job.
It’s very straightforward to find out any topic on web as compared to textbooks, as I found this piece of writing at this site.
Hello, cosmetique.news
We can help you rank your website number 1 in Google which would make your website a lead machine for your business.
We offer the following services with a suitable price.
1. SEO Services
2. Enterprise SEO Services
3. Local SEO Services
4. Google Local Services Ads Management
5. Page Speed & Core Web Vitals Optimization
Let me know if you are interested, I will send you our SEO Packages and price list.
details: https://drive.google.com/file/d/1yPWdyHUdc3VGqLr2FI0p_11sM5Pm0Edc/
Best Regards,
Dessen Peters
Business Development Executive
This info is priceless. When can I find out more?
Hi there, i read your blog occasionally and i own a similar one and i was just curious if you get a lot of spam remarks? If so how do you prevent it, any plugin or anything you can advise? I get so much lately it’s driving me insane so any help is very much appreciated.
Hi there! I know this is kinda off topic but I was wondering which blog platform are you using for this website? I’m getting sick and tired of WordPress because I’ve had issues with hackers and I’m looking at alternatives for another platform. I would be fantastic if you could point me in the direction of a good platform.
Whoa! This blog looks exactly like my old one! It’s on a entirely different subject but it has pretty much the same layout and design. Outstanding choice of colors!
Right here is the perfect web site for everyone who really wants to find out about this topic. You understand so much its almost tough to argue with you (not that I actually would want to…HaHa). You definitely put a brand new spin on a subject that has been discussed for a long time. Great stuff, just excellent!
levitra cialis order
I am regular reader, how are you everybody? This piece of writing posted at this web page is really nice.
Hello there, I discovered your web site via Google at the same time as looking for a comparable topic, your website got here up, it appears great. I have bookmarked it in my google bookmarks.
Hello there, just was alert to your blog through Google, and located that it is truly informative. I am gonna be careful for brussels. I’ll appreciate in case you proceed this in future. A lot of folks will probably be benefited out of your writing. Cheers!
levitra 20mg how to use
don’t think anything
_________________
как выиграть в вулкан казино на деньги
For hottest news you have to go to see the web and on world-wide-web I found this web site as a most excellent website for most up-to-date updates.
I’m impressed, I must say. Rarely do I encounter a blog that’s both educative and entertaining, and let me tell you, you’ve hit the nail on the head. The problem is something not enough folks are speaking intelligently about. I am very happy that I came across this during my search for something relating to this.
buying cheap cialis online
Attractive section of content. I just stumbled upon your weblog and in accession capital to assert that I get in fact enjoyed account your blog posts. Any way I’ll be subscribing to your feeds and even I achievement you access consistently fast.
5mg tadalafil
very good
_________________
aviator casino online
Hello, just wanted to tell you, I liked this blog post. It was inspiring. Keep on posting!
I am actually delighted to read this weblog posts which contains plenty of useful information, thanks for providing these information.
Hello i am kavin, its my first time to commenting anywhere, when i read this article i thought i could also make comment due to this brilliant post.
Hi there every one, here every one is sharing these knowledge, therefore it’s pleasant to read this website, and I used to visit this website every day.
Howdy, i read your blog from time to time and i own a similar one and i was just curious if you get a lot of spam responses? If so how do you stop it, any plugin or anything you can advise? I get so much lately it’s driving me crazy so any help is very much appreciated.
Hi, all the time i used to check blog posts here in the early hours in the dawn, as i love to find out more and more.
Hello! I could have sworn I’ve been to this web site before but after going through a few of the articles I realized it’s new to me. Anyhow, I’m certainly pleased I found it and I’ll be book-marking it and checking back often!
Арктика – северная полярная область Земли, включающая окраины материков Евразии и Северной Америки, почти весь Северный Ледовитый океан с островами и прилегающие к нему части Атлантического и Тихого океанов. Название её происходит от греческого слова arctos (медведь) и связано со звёздами: Полярная звезда, находящаяся почти точно в зените над Северным полюсом, принадлежит к созвездию Малая Медведица.
Century to a kind of destruction:
A fascinating discussion is definitely worth comment. I do believe that you should publish more on this subject, it may not be a taboo matter but generally folks don’t speak about these topics. To the next! Kind regards!!
Quality content is the secret to be a focus for the users to visit the web page, that’s what this web page is providing.
correct rx pharmacy
Hello very cool blog!! Man .. Excellent .. Superb .. I will bookmark your web site and take the feeds also? I’m glad to seek out numerous helpful info here in the post, we’d like develop extra techniques on this regard, thanks for sharing. . . . . .
Hello, I do think your site could be having web browser compatibility problems. When I take a look at your web site in Safari, it looks fine however when opening in I.E., it has some overlapping issues. I simply wanted to give you a quick heads up! Other than that, great site!
ralphs pharmacy
Really when someone doesn’t know then its up to other people that they will assist, so here it takes place.
Thanks for a marvelous posting! I seriously enjoyed reading it, you’re a great author. I will remember to bookmark your blog and definitely will come back from now on. I want to encourage you continue your great work, have a nice morning!
sildenafil 20 mg reviews
sildenafil 100mg oral jelly
I blog frequently and I really appreciate your content. Your article has truly peaked my interest. I’m going to bookmark your website and keep checking for new information about once a week. I opted in for your Feed as well.
When someone writes an post he/she maintains the idea of a user in his/her mind that how a user can know it. So that’s why this paragraph is great. Thanks!
My programmer is trying to convince me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on various websites for about a year and am nervous about switching to another platform. I have heard fantastic things about blogengine.net. Is there a way I can transfer all my wordpress posts into it? Any help would be really appreciated!
What’s up, its fastidious article regarding media print, we all be aware of media is a great source of facts.
Hiya! I know this is kinda off topic but I’d figured I’d ask. Would you be interested in trading links or maybe guest writing a blog post or vice-versa? My site covers a lot of the same subjects as yours and I feel we could greatly benefit from each other. If you are interested feel free to send me an e-mail. I look forward to hearing from you! Awesome blog by the way!
A person essentially help to make critically articles I’d state. This is the first time I frequented your web page and so far? I surprised with the analysis you made to make this actual submit extraordinary. Excellent job!
Во-1-х, мы здесь не для шуток, а дабы поднимать бабло. У нас эпичные задания по ютубу, отзывам и проголосовать тебе не составит труда. Пальцы в спешке шевели, и баксов на твоем счету больше.
А во-2-хhttps://tvardita.md/article/za-odin-den-v-tvardice-vysadili-bolee-1000-derevev-i-kustarnikov
, кто сказал, собственно что заработок не имеет возможности быть веселым? У нас царит атмосфера, как на самом потрясающем пикнике. Здесь в том числе и заработок делается частью приключения. Забудь скучные таски, у нас все по-нашему!
Ну и естесственно, партнерство с нами – это, брат, как скидка в самом неповторимом клубе. Ты 1-ый узнаешь о страстных промоакциях, самых заманчивых услугах и получишь билет в мир анлимитного заработка. А мы тебе не просто обещаем, а гарантируем!
И честно, не знаю, как возможно проходить мимо такового кайфа. Ты что, не пытаешься замерзнуть настоящим уличным начальником? На нашем веб-сайте ты, брат, будешь как капитан собственного корабля, маневрируя в океане крутых задач. Твои деньги, твои правила!
Не будь лузером, чувак! Забудь на тему нудные хлопоты и войди в ряды тех, кто рубит бабло, не отрываясь от кайфа. Заходи на наш сайт, дерзай и зарабатывай, как настоящий уличный браток. Здесь твое время пришло, чувак!
Hello! This is my first comment here so I just wanted to give a quick shout out and tell you I truly enjoy reading your blog posts. Can you suggest any other blogs/websites/forums that deal with the same topics? Thanks for your time!
I was really itching to tails of some wager some well-to-do on some sports matches that are episode auspicious now. I wanted to let you guys recall that I did understand what I consider to be the kindest plat in the USA.
If you destitution to confound in on the action, check it out: online gambling apps
I was able to find good advice from your content.
I was very happy to find this great site. I wanted to thank you for your time for this particularly fantastic read!! I definitely enjoyed every bit of it and I have you saved as a favorite to check out new things on your website.
Мы предлагаем вам профессиональное благоустройство, которое подчеркнет красоту вашего дома или бизнеса и создаст уютную атмосферу для отдыха и работы.
Наши специалисты имеют богатый опыт в области ландшафтного дизайна и готовы воплотить в жизнь любые ваши идеи. Мы используем только качественные материалы и современное
оборудование, чтобы обеспечить долговечность и красоту вашего ландшафта – благоустройство участка.
This website definitely has all the information and facts I wanted about this subject and didn’t know who to ask.
Hi there mates, how is all, and what you would like to say about this paragraph, in my view its truly awesome designed for me.
Sweet blog! I found it while browsing on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thank you
Hi there, I enjoy reading all of your post. I like to write a little comment to support you.
Howdy would you mind letting me know which hosting company you’re working with? I’ve loaded your blog in 3 different browsers and I must say this blog loads a lot faster then most. Can you recommend a good internet hosting provider at a reasonable price? Many thanks, I appreciate it!
Hi colleagues, how is the whole thing, and what you desire to say about this article, in my view its genuinely amazing for me.
Good info. Lucky me I discovered your site by accident (stumbleupon). I have saved it for later!
Hi, i think that i saw you visited my weblog thus i came to “return the favor”.I’m attempting to find things to improve my web site!I suppose its ok to use a few of your ideas!!
What i do not understood is in truth how you are no longer actually much more well-appreciated than you may be now. You are so intelligent. You recognize therefore considerably on the subject of this matter, produced me for my part believe it from so many various angles. Its like men and women aren’t involved unless it is one thing to accomplish with Girl gaga! Your personal stuffs great. At all times take care of it up!
I have read so many articles or reviews about the blogger lovers but this piece of writing is genuinely a good post, keep it up.
Good day! I know this is kinda off topic but I was wondering which blog platform are you using for this website? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be fantastic if you could point me in the direction of a good platform.
I think that everything typed was actually very reasonable. But, consider this, what if you added a little information? I ain’t suggesting your content isn’t good., but what if you added a title that makes people want more? I mean %BLOG_TITLE% is kinda vanilla. You might glance at Yahoo’s front page and see how they create post titles to grab people to click. You might try adding a video or a related pic or two to get readers excited about what you’ve written. In my opinion, it would bring your blog a little livelier.
Do you have a spam problem on this website; I also am a blogger, and I was wondering your situation; we have developed some nice methods and we are looking to trade techniques with others, please shoot me an e-mail if interested.
This information is worth everyone’s attention. How can I find out more?
Wow, this piece of writing is fastidious, my sister is analyzing these things, therefore I am going to convey her.
impotence
Right here is the perfect site for anybody who really wants to find out about this topic. You know a whole lot its almost tough to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a subject which has been written about for ages. Excellent stuff, just excellent!
online pharmacy that sells percocet
If you would like to grow your experience simply keep visiting this web site and be updated with the latest news update posted here.
Hi everyone, it’s my first pay a visit at this website, and piece of writing is really fruitful designed for me, keep up posting these articles or reviews.
how many mg of sildenafil should i take
Have you ever thought about adding a little bit more than just your articles? I mean, what you say is fundamental and all. However think of if you added some great photos or video clips to give your posts more, “pop”! Your content is excellent but with images and clips, this blog could definitely be one of the very best in its field. Fantastic blog!
I am also worried about this question. Can you tell me where I can read about this?
It’s truly a nice and useful piece of info. I am happy that you simply shared this helpful information with us. Please keep us informed like this. Thanks for sharing.
Suntem mandri sa va prezentantam produsele Apple in Chisinau. Aceasta inseamna ca in iStore ai acces la cele mai noi produse si oferte exclusive pe care nu le vei gasi in alta parte. Consultantii nostri sunt adevarati experti in lumea Apple si sunt intotdeauna gata sa te ajute sa alegi dispozitivul care se potriveste cel mai bine nevoilor si ambitiilor tale.
What’s Going down i’m new to this, I stumbled upon this I’ve discovered It absolutely helpful and it has aided me out loads. I’m hoping to give a contribution & aid other users like its helped me. Great job.
It’s hard to find well-informed people about this topic, but you seem like you know what you’re talking about! Thanks
tadalafil natural source
tadalafil natural source
stromectol 12mg
stromectol 12mg
My brother suggested I might like this web site. He was entirely right. This post actually made my day. You cann’t imagine simply how much time I had spent for this information! Thanks!
I am regular reader, how are you everybody? This paragraph posted at this web page is in fact fastidious.
vardenafil generico precio
vardenafil generico precio
At this time it looks like Drupal is the top blogging platform available right now. (from what I’ve read) Is that what you are using on your blog?
ivermectin cream 1%
ivermectin cream 1%
ivermectin 3mg pill
ivermectin 3mg pill
viagra generic price in india
viagra generic price in india
ivermectin 4000
ivermectin 4000
I loved as much as you’ll receive carried out right here. The sketch is attractive, your authored subject matter stylish. nonetheless, you command get got an shakiness over that you wish be delivering the following. unwell unquestionably come more formerly again as exactly the same nearly a lot often inside case you shield this hike.
I’d like to find out more? I’d like to find out some additional information.
stromectol medication
stromectol medication
tadalafil 30 tablet 5 mg
tadalafil 30 tablet 5 mg
sildenafil over the counter india
sildenafil over the counter india
ivermectin where to buy for humans
ivermectin where to buy for humans
what question should the nurse ask when assessing for therapeutic effects of vardenafil?
what question should the nurse ask when assessing for therapeutic effects of vardenafil?
Seo to top GSA-Forderung
I was genuinely itching to tails of some wager some monied on some sports matches that are episode above-board now. I wanted to allow in you guys know that I did understand what I ruminate on to be the a-one site in the USA.
If you poverty to pull down in on the spirit, check it out: See Details
vardenafil dosage maximum
Do you have a spam problem on this blog; I also am a blogger, and I was wanting to know your situation; many of us have developed some nice procedures and we are looking to swap methods with other folks, why not shoot me an e-mail if interested.
Can I just say what a relief to find a person that genuinely knows what they are discussing on the internet. You actually realize how to bring a problem to light and make it important. A lot more people really need to check this out and understand this side of your story. I was surprised you’re not more popular given that you most certainly possess the gift.
what is vardenafil 20mg
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
Usually I don’t learn article on blogs, but I wish to say that this write-up very compelled me to take a look at and do so! Your writing style has been surprised me. Thanks, very nice post.
tadalafil 5 mg brands in india
Wonderful blog! I found it while searching on Yahoo News. Do you have any suggestions on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thanks
tadalafil generic vs cialis
From many manuscripts of Antiquity
Hello to every body, it’s my first pay a quick visit of this weblog; this webpage consists of remarkable and actually fine data for readers.
I enjoy reading an article that can make men and women think. Also, many thanks for allowing for me to comment!
Hey there! I just wanted to ask if you ever have any issues with hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work due to no back up. Do you have any methods to stop hackers?
My family members every time say that I am killing my time here at net, however I know I am getting familiarity daily by reading thes fastidious content.
from lat. manus – “hand” and scribo – “I write”) ]
Hi there to every , as I am actually keen of reading this webpage’s post to be updated on a regular basis. It includes fastidious stuff.
It’s actually a great and helpful piece of information. I’m happy that you just shared this useful info with us. Please stay us informed like this. Thank you for sharing.
I’m amazed, I must say. Rarely do I encounter a blog that’s equally educative and entertaining, and let me tell you, you’ve hit the nail on the head. The problem is an issue that not enough people are speaking intelligently about. Now i’m very happy that I found this during my search for something relating to this.
Normally I don’t read article on blogs, however I wish to say that this write-up very forced me to check out and do so! Your writing style has been amazed me. Thank you, very nice article.
term manuscript (late lat.manuscriptum,
You actually make it appear really easy with your presentation but I to find this matter to be actually one thing which I think I’d by no means understand. It seems too complicated and extremely huge for me. I’m having a look forward on your next put up, I’ll attempt to get the hold of it!
Hi there, just became aware of your blog through Google, and found that it’s really informative. I’m gonna watch out for brussels. I will appreciate if you continue this in future. Lots of people will be benefited from your writing. Cheers!
I’m pretty pleased to discover this website. I wanted to thank you for your time for this particularly wonderful read!! I definitely loved every little bit of it and I have you book marked to see new things in your blog.
Have you ever thought about adding a little bit more than just your articles? I mean, what you say is important and all. Nevertheless just imagine if you added some great pictures or video clips to give your posts more, “pop”! Your content is excellent but with pics and video clips, this website could certainly be one of the most beneficial in its field. Good blog!
I am in fact grateful to the owner of this site who has shared this wonderful post at here.
Hi there, just wanted to tell you, I loved this blog post. It was funny. Keep on posting!
Filmizlesene ile hızlı film izleme fırsatını yakala, en yeni ve iyi filmleri Full HD 1080p kalitesiyle online ve bedava izle. Fermin Nazarian
Hey very interesting blog!
Hi there, of course this paragraph is in fact good and I have learned lot of things from it about blogging. thanks.
Good day! This is my first visit to your blog! We are a group of volunteers and starting a new project in a community in the same niche. Your blog provided us useful information to work on. You have done a wonderful job!
I’ll immediately snatch your rss feed as I can’t to find your email subscription link or newsletter service. Do you have any? Please allow me recognise in order that I could subscribe. Thanks.
Appreciate the recommendation. Will try it out.
tadalafil buy online canada
Everyone loves what you guys are up too. This type of clever work and exposure! Keep up the terrific works guys I’ve added you guys to my blogroll.
I do not know if it’s just me or if perhaps everyone else encountering issues with your blog. It appears as though some of the written text within your posts are running off the screen. Can somebody else please provide feedback and let me know if this is happening to them as well? This may be a issue with my internet browser because I’ve had this happen previously. Appreciate it
If some one needs to be updated with newest technologies then he must be pay a visit this web page and be up to date every day.
Hey There. I found your blog using msn. This is a really well written article. I will make sure to bookmark it and return to read more of your useful information. Thanks for the post. I will definitely comeback.
Everyone loves what you guys are usually up too. This kind of clever work and exposure! Keep up the great works guys I’ve included you guys to my own blogroll.
Excellent goods from you, man. I’ve understand your stuff previous to and you’re just extremely fantastic. I really like what you have acquired here, really like what you are saying and the way in which you say it. You make it entertaining and you still take care of to keep it smart. I can’t wait to read far more from you. This is really a tremendous site.
Hi there! I could have sworn I’ve visited this website before but after browsing through some of the posts I realized it’s new to me. Anyhow, I’m certainly pleased I stumbled upon it and I’ll be bookmarking it and checking back regularly!
of course like your web-site however you need to check the spelling on quite a few of your posts. A number of them are rife with spelling problems and I to find it very troublesome to inform the reality on the other hand I’ll definitely come back again.
Thanks for finally writing about > %blog_title% < Loved it!
Hey there would you mind letting me know which hosting company you’re using? I’ve loaded your blog in 3 different web browsers and I must say this blog loads a lot quicker then most. Can you suggest a good hosting provider at a fair price? Thank you, I appreciate it!
Post writing is also a excitement, if you be acquainted with then you can write otherwise it is difficult to write.
WOW just what I was searching for. Came here by searching for %keyword%
I blog quite often and I genuinely thank you for your information. This great article has truly peaked my interest. I’m going to take a note of your website and keep checking for new information about once per week. I opted in for your RSS feed as well.
Outstanding post but I was wondering if you could write a litte more on this subject? I’d be very grateful if you could elaborate a little bit further. Kudos!
My brother recommended I might like this blog. He was totally right. This post actually made my day. You cann’t imagine simply how much time I had spent for this info! Thanks!
I like the valuable info you provide in your articles. I’ll bookmark your blog and take a look at again here regularly. I’m slightly sure I will learn lots of new stuff proper right here! Good luck for the following!
Я частый покупатель на маркетплейсе Кракен.
кракен дарк нет маркет На днях решил попробовать заходить
через TOR и VPN, чтобы усилить свою анонимность.
Решил поделиться своим опытом.
Зайти на маркетплейс кракен дарк нет маркет плейс
через TOR очень просто. Сначала нужно установить браузер TOR, а затем
зайти на сайт Кракена по адресу krakenyfi33txsl.onion. Чтобы зайти через VPN,
нужно сначала установить VPN-клиент, а затем
подключиться к серверу в нужной стране.
После этого можно зайти на Кракен по обычному адресу kraken[.]in. Я рекомендую использовать оба метода защиты при заходе на маркетплейс Кракен.
TOR скроет ваш IP-адрес, а VPN зашифрует ваш
трафик. Вместе эти меры обеспечат максимальную
анонимность и безопасность
ваших покупок.
What’s up to every one, because I am genuinely eager of reading this web site’s post to be updated regularly. It carries nice data.
Hi, I do think this is a great blog. I stumbledupon it 😉 I’m going to come back yet again since I bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
Hi, i believe that i noticed you visited my weblog thus i came to go back the prefer?.I am trying to in finding issues to improve my website!I suppose its adequate to make use of a few of your ideas!!
Howdy! I could have sworn I’ve been to this website before but after browsing through some of the post I realized it’s new to me. Anyways, I’m definitely glad I found it and I’ll be bookmarking and checking back often!
Hello to all, it’s in fact a pleasant for me to pay a visit this website, it includes important Information.
I’m gone to convey my little brother, that he should also visit this web site on regular basis to get updated from newest gossip.
You actually make it seem so easy with your presentation however I find this topic to be actually something that I believe I would by no means understand. It sort of feels too complex and very vast for me. I’m having a look forward in your subsequent put up, I will try to get the dangle of it!
Please let me know if you’re looking for a article author for your blog. You have some really great articles and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some content for your blog in exchange for a link back to mine. Please send me an email if interested. Cheers!
I every time emailed this blog post page to all my associates, because if like to read it after that my contacts will too.
I have read so many content about the blogger lovers however this post is genuinely a pleasant article, keep it up.
Having read this I thought it was really enlightening. I appreciate you spending some time and energy to put this information together. I once again find myself personally spending a significant amount of time both reading and leaving comments. But so what, it was still worthwhile!
That is a great tip especially to those new to the blogosphere. Brief but very precise information… Thanks for sharing this one. A must read article!
Keep on working, great job!
I do not even know how I ended up here, but I thought this post was great. I don’t know who you are but certainly you are going to a famous blogger if you aren’t already 😉 Cheers!
Hey there I am so glad I found your webpage, I really found you by accident, while I was researching on Aol for something else, Anyways I am here now and would just like to say thank you for a marvelous post and a all round entertaining blog (I also love the theme/design), I don’t have time to look over it all at the minute but I have book-marked it and also included your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the great jo.
Filmizlesene ile hızlı film izleme fırsatını yakala, en yeni ve iyi filmleri Full HD 1080p kalitesiyle online ve bedava izle. Cyrus Geurts
I have been browsing online more than three hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. Personally, if all web owners and bloggers made good content as you did, the net will be much more useful than ever before.
Highly descriptive blog, I loved that bit. Will there be a part 2?
Hi, yeah this post is in fact nice and I have learned lot of things from it about blogging. thanks.
Filmizlesene ile hızlı film izleme fırsatını yakala, en yeni ve iyi filmleri Full HD 1080p kalitesiyle online ve bedava izle. Lyle Mcelmeel
Thank you for sharing your thoughts. I really appreciate your efforts and I am waiting for your further post thank you once again.
I’m impressed, I have to admit. Rarely do I encounter a blog that’s both educative and engaging, and without a doubt, you’ve hit the nail on the head. The problem is something that not enough men and women are speaking intelligently about. Now i’m very happy I found this in my search for something concerning this.
Hi there! This is my first visit to your blog! We are a collection of volunteers and starting a new project in a community in the same niche. Your blog provided us valuable information to work on. You have done a outstanding job!
Москва Купить Мефедрон? Кристаллы МЕФ?
Где в Москве Купить Мефедрон? САЙТ – https://mephedrone.top/
hey there and thank you for your information – I’ve definitely picked up something new from right here. I did however expertise several technical points using this site, since I experienced to reload the web site a lot of times previous to I could get it to load correctly. I had been wondering if your web host is OK? Not that I am complaining, but sluggish loading instances times will very frequently affect your placement in google and could damage your high quality score if ads and marketing with Adwords. Anyway I am adding this RSS to my email and could look out for a lot more of your respective exciting content. Make sure you update this again soon.
Купить Кокаин в Москве? Самый чистый Кокаин в Москве Купить
ССЫЛКА НА САЙТ- https://mephedrone.top
Greetings! I’ve been following your website for some time now and finally got the bravery to go ahead and give you a shout out from Porter Texas! Just wanted to mention keep up the great work!
Greetings! I’ve been following your weblog for a long time now and finally got the courage to go ahead and give you a shout out from Humble Tx! Just wanted to tell you keep up the good job!
Hi, i think that i saw you visited my blog so i came to go back the favor?.I am trying to to find things to enhance my web site!I guess its adequate to use some of your concepts!!
I have been surfing online more than three hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my view, if all web owners and bloggers made good content as you did, the net will be a lot more useful than ever before.
Link exchange is nothing else but it is only placing the other person’s weblog link on your page at appropriate place and other person will also do same for you.
Hello would you mind letting me know which web host you’re utilizing? I’ve loaded your blog in 3 different web browsers and I must say this blog loads a lot quicker then most. Can you recommend a good internet hosting provider at a fair price? Thanks, I appreciate it!
Nice post. I learn something totally new and challenging on blogs I stumbleupon every day. It’s always interesting to read through content from other writers and use a little something from other web sites.
When some one searches for his necessary thing, so he/she wishes to be available that in detail, thus that thing is maintained over here.
I like the helpful information you provide in your articles. I will bookmark your blog and check again here regularly. I am quite sure I will learn many new stuff right here! Best of luck for the next!
Hiya very nice blog!! Guy .. Beautiful .. Superb .. I will bookmark your site and take the feeds additionally? I’m glad to seek out a lot of useful information here in the publish, we’d like work out extra strategies in this regard, thank you for sharing. . . . . .
I have to thank you for the efforts you’ve put in penning this website. I’m hoping to view the same high-grade content by you in the future as well. In fact, your creative writing abilities has encouraged me to get my very own site now 😉
You can certainly see your enthusiasm in the work you write. The sector hopes for more passionate writers like you who aren’t afraid to mention how they believe. At all times go after your heart.
Hey there! I could have sworn I’ve been to this site before but after checking through some of the post I realized it’s new to me. Anyways, I’m definitely happy I found it and I’ll be bookmarking and checking back frequently!
I could not resist commenting. Well written!
is vardenafil better than viagra
vardenafil hcl 20mg tab vs viagra
Inspiring quest there. What happened after? Take care!
My brother suggested I may like this blog. He was once totally right. This put up actually made my day. You can not believe simply how so much time I had spent for this information! Thanks!
You ought to take part in a contest for one of the best websites on the internet. I will highly recommend this blog!
Good day! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
Τurns out it any copnvenience foг youг marketer a person haad
pick Ьetween watching theem fгom his site, aand ʏⲟu
guessed it, the site ԝaѕ very, very Ⴝ-L-O-W.
Alsο visit my blog post – capecitabina precio cerca de Atengo Jalisco
Как подготовиться к процедуре биорепарации? Подготовка включает консультацию с врачом, отказ от алкоголя и соблюдение всех рекомендаций специалиста
биорепарация сферогель https://www.biorevitalizacia.com/ .
rite aid 24 hour pharmacy store locator
meijer pharmacy store hours
Hi, constantly i used to check website posts here in the early hours in the break of day, as i like to gain knowledge of more and more.
each time i used to read smaller posts which also clear their motive, and that is also happening with this article which I am reading at this place.
Hello are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any coding expertise to make your own blog? Any help would be really appreciated!
Wow, this piece of writing is pleasant, my younger sister is analyzing such things, thus I am going to convey her.
Great article.
discount pharmacy
I was able to find good advice from your blog articles.
You really make it seem so easy with your presentation but I find this topic to be really something which I think I would never understand. It seems too complex and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
Great work! This is the kind of info that are meant to be shared around the web. Shame on Google for now not positioning this post upper! Come on over and consult with my web site . Thank you =)
loli skirt cp pthc
==> biturl.top/qeAJJf rlys.nl/6epap3 <==
This text is priceless. Where can I find out more?
Hey! This post could not be written any better! Reading this post reminds me of my old room mate! He always kept chatting about this. I will forward this page to him. Fairly certain he will have a good read. Thanks for sharing!
Hello, I think your site might be having browser compatibility issues. When I look at your blog in Opera, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, wonderful blog!
best online pharmacy to get xanax
I have to thank you for the efforts you’ve put in penning this site. I really hope to view the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has inspired me to get my own website now 😉
This site was… how do you say it? Relevant!! Finally I’ve found something that helped me. Appreciate it!
compound pharmacy domperidone
Good article. I certainly appreciate this website. Stick with it!
That is really interesting, You’re an overly skilled blogger. I’ve joined your feed and sit up for seeking more of your great post. Additionally, I’ve shared your website in my social networks
online pharmacy tramadol
You ought to be a part of a contest for one of the best websites on the net. I’m going to highly recommend this website!
You have made some good points there. I checked on the net to learn more about the issue and found most individuals will go along with your views on this website.
cialis us pharmacy
Simply want to say your article is as astonishing. The clearness for your post is just spectacular and that i can assume you’re an expert on this subject. Fine together with your permission let me to take hold of your RSS feed to stay up to date with drawing close post. Thank you one million and please keep up the rewarding work.
My relatives every time say that I am killing my time here at net, except I know I am getting knowledge every day by reading thes fastidious articles.
I wanted to thank you for this excellent read!! I absolutely enjoyed every little bit of it. I have got you saved as a favorite to check out new things you post…
I don’t even know how I ended up here, but I thought this post was good. I do not know who you are but definitely you’re going to a famous blogger if you aren’t already 😉 Cheers!
I think the admin of this site is in fact working hard for his website, since here every data is quality based stuff.
Spot on with this write-up, I actually believe that this amazing site needs a lot more attention. I’ll probably be back again to see more, thanks for the info!
https://utra-dobrogo.ru/kartinki-dobroe-utro-may/ доброе утро мая картинки
Доставка алкоголя в Екатеринбурге
Как долго длится восстановительный период после биоревитализации? Восстановительный период обычно минимален, большинство пациентов могут вернуться к обычной деятельности сразу после процедуры
биоревитализация от пигментации biorevitalizaciyaa.ru .
I don’t even understand how I ended up here, but I believed this put up used to be great. I do not understand who you might be but certainly you are going to a famous blogger when you aren’t already. Cheers!
I visited various web pages but the audio feature for audio songs present at this website is really wonderful.
always i used to read smaller content that also clear their motive, and that is also happening with this paragraph which I am reading here.
Generally I do not read article on blogs, but I wish to say that this write-up very compelled me to check out and do it! Your writing style has been surprised me. Thank you, quite nice post.
Hello to every one, as I am really keen of reading this weblog’s post to be updated regularly. It carries pleasant material.
I believe this is among the most vital info for me. And i’m satisfied studying your article. However wanna commentary on some normal issues, The web site taste is perfect, the articles is really excellent : D. Good process, cheers
Of course you’re right. There’s something about that, and that’s a great idea. I support you.
I’ve learn some just right stuff here. Definitely worth bookmarking for revisiting. I surprise how much effort you set to create this sort of wonderful informative website.
I know this site presents quality depending articles and other data, is there any other web site which offers these kinds of stuff in quality?
I’m not sure where you’re getting your information, but good topic. I needs to spend some time learning much more or understanding more. Thanks for great info I was looking for this info for my mission.
Wow, that’s what I was searching for, what a material! existing here at this blog, thanks admin of this web page.
I’m pretty pleased to discover this great site. I want to to thank you for your time for this particularly wonderful read!! I definitely savored every bit of it and i also have you saved as a favorite to look at new information on your website.
My developer is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using WordPress on several websites for about a year and am nervous about switching to another platform. I have heard very good things about blogengine.net. Is there a way I can import all my wordpress content into it? Any help would be really appreciated!
Great information. Lucky me I ran across your site by chance (stumbleupon). I have book marked it for later!
trimox 500 mg dosage
trimox 500 mg dosage
Wow, fantastic blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your site is wonderful, let alone the content!
will keflex treat a sinus infection
will keflex treat a sinus infection
Hey there! I’ve been following your blog for a long time now and finally got the bravery to go ahead and give you a shout out from Lubbock Texas! Just wanted to mention keep up the fantastic work!
I all the time used to study piece of writing in news papers but now as I am a user of net therefore from now I am using net for articles or reviews, thanks to web.
ciprofloxacin 500mg dosage
ciprofloxacin 500mg dosage
obviously like your web-site but you need to test the spelling on quite a few of your posts. Several of them are rife with spelling issues and I to find it very bothersome to inform the truth then again I’ll certainly come again again.
valacyclovir while pregnant
valacyclovir while pregnant
metronidazole for rosacea
metronidazole for rosacea
I blog frequently and I really thank you for your information. This article has really peaked my interest. I am going to take a note of your site and keep checking for new information about once a week. I opted in for your RSS feed as well.
amoxicillin prescription
amoxicillin prescription
Thanks for the good writeup. It in fact was a amusement account it. Look complex to far brought agreeable from you! However, how could we communicate?
Hi, after reading this amazing article i am as well delighted to share my knowledge here with mates.
При попытке войти в учетную запись на Kraken я столкнулся с сообщением Пользователь не найден.
кракен даркнет пользователь не найден что делать Сначала
я запаниковал, так как на счету было немало средств.
Но затем я вспомнил о руководстве
по восстановлению доступа к аккаунту Kraken, которое я прочитал ранее (кракен даркнет
пользователь не найден что делать).
Следуя пошаговым инструкциям, я связался со службой поддержки Kraken. Они быстро отреагировали и
попросили предоставить удостоверение личности и подтверждение адреса.
После отправки необходимых
документов мой доступ был восстановлен в течение нескольких часов.
Я был поражен эффективностью и оперативностью поддержки Kraken. Это еще
раз подтвердило, что они – один из самых надежных и безопасных маркетплейсов в отрасли.
купить юридический адрес для регистрации
What’s up, this weekend is fastidious designed for me, because this occasion i am reading this enormous informative paragraph here at my residence.
Cтальные двери с завода с установкой за 1 день.
Любые конфигурации замков на выбор. Более 3500 моделей на складе: тут
Hello there, You have done a fantastic job. I will certainly digg it and personally recommend to my friends. I am confident they’ll be benefited from this website.
cephalexin vs amoxicillin
cephalexin vs amoxicillin
I like the helpful information you provide in your articles. I will bookmark your weblog and check again here frequently. I’m quite certain I will learn many new stuff right here! Good luck for the next!
whats doxycycline used for
whats doxycycline used for
My brother recommended I would possibly like this blog. He was totally right. This put up truly made my day. You can not believe just how so much time I had spent for this info! Thank you!
Greetings! This is my first visit to your blog! We are a collection of volunteers and starting a new project in a community in the same niche. Your blog provided us beneficial information to work on. You have done a extraordinary job!
I know this website presents quality based content and extra material, is there any other web site which provides such information in quality?
Hey very interesting blog!
It’s in point of fact a nice and helpful piece of info. I am happy that you shared this helpful information with us. Please keep us informed like this. Thank you for sharing.
what is the lowest dose of metformin you can take
what is the lowest dose of metformin you can take
lyrica side effects long-term
lyrica side effects long-term
can i take an extra lisinopril if my blood pressure is high
can i take an extra lisinopril if my blood pressure is high
why is trazodone not helping me sleep
why is trazodone not helping me sleep
Hello to every one, the contents existing at this website are truly awesome for people experience, well, keep up the nice work fellows.
I couldn’t refrain from commenting. Exceptionally well written!
We are a group of volunteers and starting a new scheme in our community. Your web site provided us with valuable information to work on. You have done an impressive job and our whole group will probably be grateful to you.
modafinil class
modafinil class
Hello to all, it’s actually a nice for me to go to see this web site, it contains useful Information.
My programmer is trying to convince me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on various websites for about a year and am concerned about switching to another platform. I have heard great things about blogengine.net. Is there a way I can transfer all my wordpress posts into it? Any help would be greatly appreciated!
Fine way of telling, and pleasant article to obtain facts on the topic of my presentation focus, which i am going to convey in institution of higher education.
It’s remarkable to pay a visit this web page and reading the views of all friends on the topic of this piece of writing, while I am also keen of getting experience.
I enjoy, cause I found just what I was looking for. You’ve ended my 4 day long hunt! God Bless you man. Have a nice day. Bye
Hello are using WordPress for your site platform? I’m new to the blog world but I’m trying to get started and create my own. Do you require any html coding knowledge to make your own blog? Any help would be really appreciated!
поролон купить в москве
Hey there this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get guidance from someone with experience. Any help would be greatly appreciated!
Hi there, I enjoy reading all of your article post. I wanted to write a little comment to support you.
What’s up to every one, for the reason that I am genuinely eager of reading this website’s post to be updated on a regular basis. It includes good material.
Excellent goods from you, man. I have understand your stuff previous to and you’re simply too wonderful. I really like what you have got here, certainly like what you are saying and the way in which by which you are saying it. You make it enjoyable and you still care for to stay it smart. I can’t wait to learn much more from you. That is really a wonderful web site.
I like the valuable information you provide in your articles. I will bookmark your weblog and check again here frequently. I’m quite certain I’ll learn a lot of new stuff right here! Best of luck for the next!
Hi friends, how is the whole thing, and what you wish for to say about this post, in my view its in fact awesome in support of me.
I delight in, lead to I found exactly what I was having a look for. You’ve ended my 4 day long hunt! God Bless you man. Have a nice day. Bye
http://ceicag.org/
There is definately a lot to know about this issue. I like all of the points you have made.
excellent issues altogether, you just gained a emblem new reader. What could you suggest in regards to your submit that you simply made some days ago? Any positive?
With havin so much content do you ever run into any issues of plagorism or copyright infringement? My blog has a lot of unique content I’ve either written myself or outsourced but it appears a lot of it is popping it up all over the internet without my permission. Do you know any methods to help prevent content from being stolen? I’d certainly appreciate it.
Great site. Lots of useful information here. I’m sending it to several friends ans additionally sharing in delicious. And of course, thank you on your effort!
If you are going for finest contents like myself, only pay a quick visit this web page every day for the reason that it provides quality contents, thanks
Why viewers still make use of to read news papers when in this technological globe everything is available on net?
It’s a shame you don’t have a donate button! I’d certainly donate to this fantastic blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to fresh updates and will share this site with my Facebook group. Chat soon!
I was able to find good information from your content.
It’s actually very complex in this full of activity life to listen news on Television, so I only use web for that reason, and take the most up-to-date news.
Hello mates, its wonderful article concerning cultureand entirely defined, keep it up all the time.
Greate pieces. Keep writing such kind of information on your site. Im really impressed by it.
Hello there, You have performed an incredible job. I will definitely digg it and in my opinion recommend to my friends. I’m sure they’ll be benefited from this site.
Hello! I’ve been reading your website for a while now and finally got the courage to go ahead and give you a shout out from New Caney Texas! Just wanted to say keep up the excellent job!
What’s up to every body, it’s my first visit of this webpage; this web site carries amazing and really excellent data in favor of visitors.
What’s up everyone, it’s my first pay a quick visit at this site, and post is really fruitful in favor of me, keep up posting these content.
I am extremely impressed together with your writing talents and also with the layout on your blog. Is that this a paid subject matter or did you modify it your self? Anyway keep up the nice quality writing, it is rare to see a great weblog like this one nowadays..
An outstanding share! I have just forwarded this onto a coworker who has been doing a little homework on this. And he actually ordered me lunch simply because I found it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending the time to discuss this subject here on your website.
hello!,I like your writing so much! share we keep in touch extra approximately your post on AOL? I need a specialist on this space to unravel my problem. May be that’s you! Looking forward to see you.
Thank you for sharing your thoughts. I really appreciate your efforts and I am waiting for your next post thank you once again.
Great delivery. Great arguments. Keep up the good work.
It is perfect time to make some plans for the long run and it is time to be happy. I have read this submit and if I may I wish to counsel you few interesting issues or suggestions. Perhaps you can write subsequent articles referring to this article. I want to learn even more issues approximately it!
Thank you for sharing your thoughts. I truly appreciate your efforts and I am waiting for your next write ups thanks once again.
Way cool! Some extremely valid points! I appreciate you writing this article and also the rest of the website is very good.
Simply desire to say your article is as astounding. The clearness in your submit is just great and i can assume you are an expert in this subject. Well together with your permission allow me to clutch your RSS feed to stay updated with drawing close post. Thanks a million and please carry on the enjoyable work.
Greate pieces. Keep posting such kind of information on your blog. Im really impressed by your blog.
Hi there, You have performed a great job. I will certainly digg it and personally recommend to my friends. I’m confident they’ll be benefited from this website.
I’m extremely inspired with your writing abilities as well as with the format for your weblog. Is that this a paid theme or did you modify it yourself? Anyway keep up the excellent quality writing, it is rare to look a nice blog like this one nowadays..
Hello there! This is my first visit to your blog! We are a collection of volunteers and starting a new initiative in a community in the same niche. Your blog provided us valuable information to work on. You have done a extraordinary job!
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you can do with some pics to drive the message home a little bit, but instead of that, this is great blog. An excellent read. I will definitely be back.
you are in reality a excellent webmaster. The site loading pace is amazing. It sort of feels that you are doing any distinctive trick. In addition, The contents are masterpiece. you’ve performed a excellent activity on this topic!
Excellent blog here! Also your site loads up very fast! What web host are you using? Can I get your affiliate link to your host? I wish my website loaded up as fast as yours lol
Thanks a lot for sharing this with all of us you really recognize what you are talking approximately! Bookmarked. Kindly additionally consult with my web site =). We will have a link alternate agreement between us
of course like your website but you have to take a look at the spelling on quite a few of your posts. Many of them are rife with spelling problems and I find it very troublesome to inform the reality nevertheless I’ll definitely come again again.
This is very interesting, You are a very skilled blogger. I have joined your rss feed and look forward to seeking more of your magnificent post. Also, I’ve shared your web site in my social networks!
Every weekend i used to visit this site, as i want enjoyment, as this this website conations really pleasant funny data too.
Hi friends, pleasant paragraph and pleasant urging commented at this place, I am actually enjoying by these.
Wonderful goods from you, man. I’ve understand your stuff previous to and you’re just extremely wonderful. I actually like what you have acquired here, really like what you are saying and the way in which you say it. You make it entertaining and you still care for to keep it sensible. I can not wait to read far more from you. This is actually a tremendous website.
Hi, the whole thing is going perfectly here and ofcourse every one is sharing information, that’s actually good, keep up writing.
Hello, Neat post. There is a problem with your website in web explorer, could check this? IE nonetheless is the marketplace leader and a good element of folks will omit your excellent writing due to this problem.
Aw, this was a very good post. Finding the time and actual effort to create a great article… but what can I say… I procrastinate a whole lot and don’t manage to get anything done.
Today, while I was at work, my sister stole my iphone and tested to see if it can survive a 25 foot drop, just so she can be a youtube sensation. My apple ipad is now broken and she has 83 views. I know this is entirely off topic but I had to share it with someone!
Hi, i think that i saw you visited my website so i came to “return the favor”.I’m attempting to find things to improve my site!I suppose its ok to use a few of your ideas!!
Because the admin of this web page is working, no question very quickly it will be renowned, due to its quality contents.
Thanks very nice blog!
Hello I am so glad I found your webpage, I really found you by accident, while I was looking on Digg for something else, Nonetheless I am here now and would just like to say cheers for a marvelous post and a all round enjoyable blog (I also love the theme/design), I don’t have time to browse it all at the moment but I have saved it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the awesome b.
I am regular reader, how are you everybody? This paragraph posted at this site is actually pleasant.
you’re really a excellent webmaster. The web site loading speed is incredible. It kind of feels that you’re doing any distinctive trick. Moreover, The contents are masterpiece. you’ve performed a great task in this subject!
I was wondering if you ever considered changing the page layout of your website? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having 1 or two images. Maybe you could space it out better?
Hi there colleagues, how is the whole thing, and what you would like to say regarding this paragraph, in my view its truly remarkable in favor of me.
This site definitely has all the information I needed concerning this subject and didn’t know who to ask.
Hello everyone, it’s my first pay a quick visit at this website, and post is in fact fruitful for me, keep up posting such content.
Hello I am so delighted I found your blog page, I really found you by accident, while I was researching on Aol for something else, Regardless I am here now and would just like to say thanks a lot for a fantastic post and a all round entertaining blog (I also love the theme/design), I don’t have time to browse it all at the minute but I have saved it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the excellent work.
It’s amazing designed for me to have a web site, which is useful in favor of my know-how. thanks admin
Useful info. Fortunate me I found your web site unintentionally, and I am stunned why this accident did not took place in advance! I bookmarked it.
Hello colleagues, its fantastic article regarding tutoringand fully defined, keep it up all the time.
Whats up very cool site!! Man .. Excellent .. Wonderful .. I’ll bookmark your web site and take the feeds additionally? I am glad to seek out numerous useful information right here in the publish, we need work out more techniques in this regard, thanks for sharing. . . . . .
Линзы для лазерного станка – это элементы оптической системы лазерной головки. Устанавливаются в блоках коллиматора и фокусатора.
Подвержены быстрому износу и нуждаются в регулярной замене. Наша компания производит линзы для оптоволоконных и твердотельных лазеров из плавленого кварца,
износостойких материалов высокой чистоты с отличными оптическими характеристиками. Всегда в наличии линзы для лазерного станка
There’s definately a lot to learn about this subject. I like all the points you made.
Thanks for sharing your thoughts on %meta_keyword%. Regards
Thanks for some other wonderful post. The place else could anyone get that type of information in such a perfect method of writing? I have a presentation next week, and I am at the search for such info.
Hey! I could have sworn I’ve been to this blog before but after checking through some of the post I realized it’s new to me. Anyways, I’m definitely glad I found it and I’ll be book-marking and checking back often!
Fantastic goods from you, man. I’ve understand your stuff previous to and you are just too excellent. I really like what you have acquired here, really like what you’re stating and the way in which you say it. You make it enjoyable and you still take care of to keep it smart. I cant wait to read much more from you. This is actually a wonderful web site.
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to your site? My website is in the very same niche as yours and my visitors would definitely benefit from a lot of the information you provide here. Please let me know if this okay with you. Thank you!
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
cp loli frail
==> biturl.top/qeAJJf rlys.nl/6epap3 <==
Добрый день! Меня зовут Шестаков Юрий Иванович, я дерматолог с многолетним опытом работы в области эстетической медицины. Сейчас я отвечу на ваши вопросы и расскажу полезной информацией о лазерном удалении папиллом. Моя цель — помочь вам понять, как безопасно и эффективно избавиться от папиллом и какие преимущества имеет лазерное удаление.
Лазерное удаление папиллом: сравнение цен в разных клиниках
Насколько эффективно лазерное удаление папиллом? – Лазерное удаление папиллом является высокоэффективным методом, который позволяет полностью удалить новообразования с минимальным риском рецидива.
How effective is laser removal of papillomas? – Laser removal of papillomas is a highly effective method that allows complete removal of growths with minimal risk of recurrence.
стоимость удаления папиллом лазером https://laserwartremoval.ru/ .
buy nolvadex
buy nolvadex
Mistakenly Identified as Deceased by TransUnion: An Increasing Concern
Inaccuracies in credit reporting can have very harmful effects. One of the scariest errors people may face is having their credit bureaus, such as **TransUnion**, mistakenly report them as dead. This serious mistake can have a significant harmful impact on everything from job prospects to credit applications. It is crucial in such circumstances to know how to dispute a background check and to negotiate the challenges of credit report disputes.
### Understanding the Problem
Envision discovering you are erroneously listed as deceased on your credit record. This is not an uncommon issue, however. Individuals in this situation must act swiftly to correct it. One key first step can be to contact a background check lawyer or a deceased on credit report lawyer. Experts in background check errors, these professionals can give the guidance you need to correct your credit report.
How to Contest a Background Check
Understanding how to dispute a background check becomes critical when faced with such a significant mistake. Contact the credit bureau that made the error first. You must verify your identification and show you are still alive. Employing marked as deceased on credit report lawyers can expedite this sometimes intimidating process. These experts can guarantee your case is handled efficiently and walk you through the complexities of a background check dispute.
The Role of Attorneys in Resolving Credit Report Errors
Notably valuable is collaborating with my credit report says I’m deceased lawyers. These attorneys specialize in detecting and correcting serious mistakes on credit reports. They can represent you in dealings with credit bureaus and other relevant parties to guarantee your problem is handled and resolved promptly. Taking into account their experience in background check disputes, they are knowledgeable with the legal routes accessible to correct such errors and can give strong counsel if needed.
Preventing Future Errors
Once the error is resolved, steps must be taken to stop it from recurring. Regularly reviewing for errors in your credit report can help spot problems early on. Active credit monitoring and understanding how to dispute a background check can help guard against potential mistakes. Should discrepancies surface, acting swiftly to **dispute a background check** can lessen the consequence of these errors on your individual and monetary life.
In conclusion, it can be troubling when TransUnion reports you as deceased. However, with the right method and support from experienced experts like a background check lawyer, individuals can handle the procedure of disputing these errors and recovering their creditworthiness.
Learn more: https://bucceri-pincus.com/transunion-says-im-deceased/
Yesterday, while I was at work, my cousin stole my iphone and tested to see if it can survive a twenty five foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views. I know this is totally off topic but I had to share it with someone!
Como optimizar operaciones con Vibration Analysis Equipment
I have been surfing online greater than 3 hours nowadays, yet I never discovered any attention-grabbing article like yours. It is lovely worth sufficient for me. In my view, if all webmasters and bloggers made good content as you did, the web can be much more useful than ever before.
Если вы задумываетесь о сотрудничестве с Esperio, то ознакомьтесь предварительно с этим обзором. Брокер заявляет о себе, как об одном из лучших на рынке. Однако наше мнение по этому вопросу противоположное. Мы проведем подробный анализ предложений этой компании и изучим отзывы трейдеров, чтобы определить, насколько ей можно доверять.
О компании
Официальное название: Esperio;
Адрес, контакты: First St. Vincent Bank Ltd Building, James Street, Kingstown, Сент-Винсент и Гренадины;
Лицензия: нет;
Как давно на рынке: с 2021;
Услуги: трейдинг;
Условия: леверидж до 1:1000, нет ограничений по минимальному депозиту;
Торговый терминал: MetaTrader 4/5;
Активы: контракты на разницу цен.
Самые свежие отзывы о Esperio со всего интернета
Несмотря на почти что вдохновляющее название, брокер не особо смог заслужить похвалу от трейдеров, особенно российских. Впрочем, судя по официальному сайту, именно на них он и ориентируется.
Итак, автор с ником MEMFIS1990 уверяет, что никому не удастся заработать с этим брокером. Согласно его комментарию, Esperio просто не выводит деньги. Мужчина уверяет, что все положительные отзывы на официальном сайте компании — фейковые. Он советует трейдерам работать только с проверенными брокерами, а не ноунеймами.
Следующий автор с ником Raspop нашел только один положительный момент у этого брокера. В отзыве он упоминает, что Esperio не скрывает отрицательной доходности по своим портфелям. В остальном мужчина тоже не советует связываться с этой компанией. Как минимум, потому что она мало кому известна и не регулируется авторитетными надзорными органами.
Не все трейдеры оказали столь осторожными, чтобы не торговать с Esperio. Автор следующего отзыва потерял 2 тысячи долларов на этой платформе. Он пополнял счет через систему WebMoney. К сожалению, обращение к юристам не решило вопрос, процедура чарджбэка в этом случае оказалась недоступной. Клиенту пришлось смириться с потерей, так как все его обращения Esperio все равно проигнорировал.
Еще одна девушка вообще описывает в отзыве порядок работы Esperio. Александра утверждает, что представители компании ищут потенциальных клиентов в социальных сетях. Изначально будущим жертвам предлагают работу, а именно, простое заполнение Excel таблиц. Потом их уговаривают приобрести курс обучения не менее чем за 50 тысяч рублей, и, наконец, самим начать торговлю на платформе Esperio. Естественно, все заканчивается сразу после пополнения. Аналитики, советующие открывать сделки, скорее рано, чем поздно, загоняют депозит трейдера в ноль.
Подтверждает слова Александры Виктория. Она называет Esperio самым ужасным местом работы. Девушка пишет в отзыве, что после месяца оплачиваемой стажировки ей, в конце концов, ничего не перечислили. Зато она регулярно терпела оскорбления от руководства. Виктория не скрывает, что главной ее обязанностью был холодный обзвон и развод людей на деньги.
Признаки обмана, мошенничества
Когда реальные отзывы настолько отличаются от тех, что брокер размещает на своем официальном сайте, вывод очевиден. Вряд ли перед нами честный и прозрачный посредник. К тому же, мы нашли и другие спорные моменты.
Срок существования проекта
Трейдеров пытаются убедить в том, что Esperio появился в отрасли еще в 2012 году. Это утверждение можно прочесть в коротком описании самой компании, и заметить в футере сайта. Однако ничего общего с реальным положением вещей такие заявления не имеют. В отзывах авторы пишут об отсутствии узнаваемости бренда не просто так. До недавнего времени о таком посреднике никто не знал.
Данные веб-архива показывают, что брокер занял сайт в июне 2021 года. В самом деле, сложно представить, чтобы за 10 лет работы действительно надежный брокер так и остался для большинства трейдеров неузнаваемым.
Регистрация
С юридическими данными у Esperio вообще произошла какая-то путаница. Брокер указывает в качестве управляющей компании некую OFG Cap LTD. При этом в реестр Сент-Винсент и Гренадин она должна быть внесена под номером 20603. Разумеется, мы не нашли ни одного упоминания о таком наборе цифр.
Но хотя бы OFG Cap, правда, не LTD, а LLC все-таки существует. Кстати, она была инкорпорирована в 2022 году, даже позже, чем появился официальный сайт. Уж совсем никак не в 2012. В футере указана недостоверная информация.
Добавить ко всему перечисленному стоит и то, что гренадинский офшор — не самое лучшее место в мире для регистрации бизнеса. Вернее, для мошенников, конечно, сойдет. А вот у клиентов, особенно трейдеров, могут возникнуть существенные проблемы при сотрудничестве с такими компаниями.
Отсутствие документов
Назваться брокером недостаточно. Esperio было бы неплохо еще получить официальное разрешение на свою деятельность. Но Сент-Винсент и Гренадины как раз предпочитают те посредники, которым не хочется думать о лицензиях. FSA (регулятор в этой юрисдикции) не выдает подобным онлайн дилинговым центрам лицензии. И вообще он не ведет никакого надзора за их деятельностью.
На главной странице регулятора так и написано, что внесение в реестр — это не гарантия хорошей репутации компании. Российский Центробанк, например, вообще заблокировал сайт Esperio и внес фирму в черный список.
Выводы
Esperio зарегистрирован в офшорной зоне Сент-Винсент и Гренадин, что означает отсутствие контроля со стороны государственных органов. Кроме того, у него нет лицензии на осуществление брокерской деятельности. Торговать на таких площадках не стоит. Это легко обернется потерей капитала.
If some one needs expert view on the topic of running a blog then i advise him/her to pay a quick visit this web site, Keep up the pleasant job.
Hi friends, how is everything, and what you want to say regarding this piece of writing, in my view its in fact awesome in favor of me.
Hi there mates, good post and good arguments commented at this place, I am actually enjoying by these.
What’s up to all, how is everything, I think every one is getting more from this web site, and your views are nice in support of new users.
Hi there, I found your site via Google at the same time as looking for a comparable matter, your website got here up, it appears to be like good. I’ve bookmarked it in my google bookmarks.
Hi there, just was alert to your weblog thru Google, and located that it is truly informative. I’m gonna be careful for brussels. I’ll appreciate in the event you continue this in future. Numerous other people might be benefited out of your writing. Cheers!
Hi there just wanted to give you a quick heads up. The text in your content seem to be running off the screen in Firefox. I’m not sure if this is a formatting issue or something to do with internet browser compatibility but I figured I’d post to let you know. The design and style look great though! Hope you get the issue solved soon. Kudos
I have read so many articles concerning the blogger lovers however this piece of writing is in fact a good post, keep it up.
Hello, after reading this amazing post i am also delighted to share my knowledge here with colleagues.
Hi there to every body, it’s my first visit of this website; this website includes remarkable and really excellent data in support of readers.
Thanks for another excellent article. Where else could anyone get that kind of information in such a perfect approach of writing? I have a presentation next week, and I am on the search for such info.
Seeking to boost the reliability and efficiency of your equipment? Check out the Balanset-1A – a cutting-edge balancing and vibration analysis device with proven practical benefits.
The Balanset-1A comes with two vibration sensors and a laser tachometer, allowing for balancing in one or two planes. It not only measures vibrations but also automatically calculates balancing parameters, greatly simplifying the process.
Users of the Balanset-1A praise its high accuracy and ease of use. The device saves all results in an archive, allowing easy report creation and repeated balancing procedures, saving you time and resources.
Don’t miss the opportunity to enhance your equipment’s efficiency. Order the Balanset-1A today and experience its benefits firsthand.
Here you can read more about What is the cause of static imbalance?ventilation balancing
Heya! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading through your blog and look forward to all your posts! Carry on the great work!
Fantastic website you have here but I was wondering if you knew of any user discussion forums that cover the same topics talked about in this article? I’d really love to be a part of group where I can get responses from other knowledgeable people that share the same interest. If you have any suggestions, please let me know. Kudos!
Thanks for one’s marvelous posting! I quite enjoyed reading it, you are a great author. I will be sure to bookmark your blog and will come back in the foreseeable future. I want to encourage you to continue your great posts, have a nice weekend!
Nice post. I was checking constantly this blog and I am impressed! Extremely helpful information particularly the last part 🙂 I care for such information much. I was looking for this particular information for a long time. Thank you and good luck.
My spouse and I stumbled over here from a different website and thought I might as well check things out. I like what I see so now i am following you. Look forward to going over your web page again.
Everything is very open with a precise clarification of the issues. It was truly informative. Your site is useful. Thank you for sharing!
ancient and medieval Latin,
Great weblog here! Also your web site quite a bit up fast! What host are you using? Can I get your associate link to your host? I want my site loaded up as fast as yours lol
Hey! This post could not be written any better! Reading this post reminds me of my previous room mate! He always kept talking about this. I will forward this article to him. Pretty sure he will have a good read. Many thanks for sharing!
I think the admin of this site is genuinely working hard for his web page, as here every material is quality based information.
whoah this weblog is great i really like reading your articles. Stay up the great work! You already know, lots of individuals are searching round for this information, you could aid them greatly.
Thank you for some other informative site. Where else may just I get that kind of info written in such an ideal way? I have a undertaking that I’m simply now working on, and I’ve been at the look out for such info.
Appreciate the recommendation. Let me try it out.
Hi friends, fastidious post and good urging commented here, I am actually enjoying by these.
It’s going to be ending of mine day, however before ending I am reading this impressive article to increase my experience.
I think that is one of the so much vital info for me. And i’m satisfied reading your article. However want to observation on few general issues, The website taste is perfect, the articles is really excellent : D. Good process, cheers
Your style is really unique compared to other folks I have read stuff from. I appreciate you for posting when you have the opportunity, Guess I will just book mark this web site.
I used to be recommended this blog by way of my cousin. I am no longer sure whether this post is written by way of him as nobody else recognize such precise about my problem. You are wonderful! Thank you!
Great article, just what I wanted to find.
I don’t even know how I ended up here, but I thought this post was great. I do not know who you are but definitely you’re going to a famous blogger if you aren’t already 😉 Cheers!
hi!,I really like your writing very much! proportion we be in contact extra about your post on AOL? I need a specialist on this space to resolve my problem. Maybe that’s you! Having a look forward to see you.
This is very fascinating, You are an excessively skilled blogger. I’ve joined your feed and look forward to searching for extra of your fantastic post. Also, I have shared your site in my social networks
Good blog post. I definitely appreciate this website. Thanks!
Hi are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you require any coding knowledge to make your own blog? Any help would be greatly appreciated!
I got this web site from my pal who shared with me regarding this web site and now this time I am browsing this site and reading very informative articles at this time.
Hi there! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new posts.
Причины боли при онкологии
https://e-pochemuchka.ru
Національна комісія з цінних паперів та фондового ринку попереджає інвесторів про ризики втрати грошей в “Центрі біржових технологій” та «ISRAEL INVESTMENTS LTD».
Ці “проекти” не отримували від Комісії жодних ліцензій, необхідних для здійснення інвестиційної діяльності чи надання послуг з цінними паперами та іншими фінансовими інструментами на території України. Також Комісія не надавала необхідних дозволів на розміщення реклами, яку обидва проекти активно замовляють.
Комісія вбачає в діяльності, види якої вказані на сайтах проектів «ISRAEL INVESTMENTS LTD» та «Центр Біржових Технологій», ознаки можливого зловживання на ринку фінансових послуг.
НКЦПФР, в межах компетенції, здійснила всі необхідні дії, зокрема, зверталась (безуспішно) із запитами до осіб, які розміщують рекламні матеріали, порушила (успішно) справи про правопорушення за безліцензійну діяльність на фондовому ринку.
Крім того, повідомила правоохоронні органи та Службу України з питань безпечності харчових продуктів та захисту споживачів.
Центр Біржових Технологій
Під час здійснення регулярного нагляду за галузевою рекламною активністю аналітики Комісії виявили сторінку “компанії” «Центр Біржових Технологій», на якій громадянам пропонують послуги портфельного інвестування, а саме інвестування у портфель «Клервант», який сформований з акцій найбільших світових компаній і недооцінених активів.
Далі наводимо цитати з відповідної сторінки компанії «Центр Біржових Технологій», які можуть мати ознаки реклами та надання послуг на фондовому ринку, які здійснюються без відповідного дозволу Комісії:
«Повний пакет послуг, що надається Центром Біржових Технологій — надійний фундамент, на якому будується і буде розвиватися ваш бізнес: навчання, програмне забезпечення, торгова система, аналітична і технічна підтримка на всіх етапах, від відкриття рахунку до рішення призупинити або закрити торгівлю»;
«Клеревант» сформований фахівцями компанії ЦБТ — визнаними лідерами по портфельному інвестуванню в Україні. Важливо знати: на момент роботи портфеля ваші гроші знаходяться на рахунку європейського банку. Вони застраховані фондом гарантованого страхування і інвесторським компенсаційним фондом Європи»;
«Унікальність «Клеревант» полягає в надійності і інноваціях. Даний інвестиційний портфель поєднав в собі високу прибутковість акцій найбільших світових компаній і недооцінені активи. Можливість заробити від $ 5 000 до $ 50 000 за декілька місяців. Вигода: максимальний дохід завдяки унікальній стратегії оцінки акцій та інших активів»;
«Центр Біржових Технологій — безумовний лідер за кількістю ВІП-клієнтів серед всіх українських компаній, які працюють на фінансових ринках».
Також аналітики Комісії виявили багато зовнішньої реклами проекту в м. Києві, роликів на радіо, банерів та реклами на багатьох інформаційних ресурсах у мережі інтернет. Як сказано на сайті проекту, “Центр Біржових Технологій” має розгалуджену мережу філій та представництв у багатьох містах України”.
З відкритих джерел Комісія також встановила, що послуги для забезпечення діяльності домену надаються компанією «OVH Hosting Oy», яка зареєстрована в Фінляндії, та використовує віртуальні приватні хмарні сервери (VPS), які забезпечують анонімність власників доменів.
На офіційний запит Комісії про надання інформації від ЦБТ відповідь так і не надійшла.
ISRAEL INVESTMENTS LTD
Сайт проекту «ISRAEL INVESTMENTS LTD» пропонує громадянам послуги портфельного інвестування та п’ять різних варіантів інвестиційних пакетів за ціною від $ 500 до $ 50 000, які “сформовані з дорогоцінних металів, нафти, цінних паперів, криптовалют та стартапів”. Також на сторінці компанії зазначені такі послуги, як управління інвестиційними портфелями, інвестування у різні види накопичувальних фондів та у біржові індексні облігації, надання інформаційно-аналітичних та брокерських послуг.
Далі наводимо цитати з відповідної сторінки компанії «ISRAEL INVESTMENTS LTD», які можуть мати ознаки реклами та надання послуг на фондовому ринку, які здійснюються без відповідного дозволу Комісії:
«Професіонали нашої компанії також можуть створити індивідуальний інвестиційний портфель, з урахуванням Ваших побажань. Він буде доповнений фінансовими інструментами, які допоможуть швидше досягти поставлених цілей. Щоб гроші почали працювати на Вас, покладайтеся на професіоналів!»;
«ІП надає стабільний щомісячний пасивний дохід. Придбати портфель дуже просто: вибираєте пакет, тиснете «інвестувати, заповнюєте просту форму зворотного зв’язку. Все, дуже просто, далі з Вами зв’яжеться наш фахівець. Він надасть повну консультацію і обговорить всі деталі обраного портфеля»;
«Інвестиційний портфель це – різні активи, об’єднані для досягнення певних фінансових цілей. ІП може складатися з золота, нерухомості, цінних паперів, опціонів. Israel Investments пропонує готові інвестиційні пакети, які будуть приносити прибуток незалежно від політичної чи ринкової ситуації. Портфелі доступні для громадян будь-яких країн».
Рекламу «ISRAEL INVESTMENTS LTD» аналітики виявили на багатьох популярних інформаційних ресурсах у мережі інтернет, у соціальних мережах. Відповідно до інформації з сайту, «ISRAEL INVESTMENTS LTD» має представництва в Ізраїлі, Англії, Італії, Швейцарії, та Україні.
Згідно з даними Єдиного державного реєстру юридичних осіб, фізичних осіб-підприємців та громадських формувань, офіційне представництво «ISRAEL INVESTMENTS LTD» в Україні зареєстровано як юридична особа – ПП “ІФЛК “ІЗРАЇЛЬ ІНВЕСТМЕНС” (код за ЄДРПОУ 42620622).
Послуги забезпечення діяльності домену надаються компанією «101domain», яка зареєстрована в США, і також надає своїм клієнтам можливість приховати інформацію про них у загальнодоступних Інтернет джерелах.
На офіційний запит Комісії про надання інформації від проекту відповідь так і не надійшла.
Комісія констатує в обох випадках всі ознаки можливого зловживання на ринку фінансових послуг, що несе загрозу введення в оману громадян та втрати ними значних коштів. НКЦПФР вживає всіх законних заходів щоб мінімізувати потенційно протиправну діяльність та попереджає інвесторів про ризики втрати грошей.
Hello there, just became alert to your blog through Google, and found that it’s really informative. I’m gonna watch out for brussels. I will be grateful if you continue this in future. Many people will be benefited from your writing. Cheers!
I blog frequently and I seriously appreciate your information. The article has truly peaked my interest. I’m going to take a note of your blog and keep checking for new details about once a week. I opted in for your Feed too.
Hi my friend! I want to say that this article is awesome, great written and include almost all vital infos. I’d like to look more posts like this .
What’s up to all, how is the whole thing, I think every one is getting more from this web site, and your views are good designed for new people.
Definitely imagine that that you stated. Your favourite reason appeared to be on the internet the simplest factor to have in mind of. I say to you, I certainly get annoyed while other people think about concerns that they plainly don’t recognise about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , folks could take a signal. Will likely be again to get more. Thank you
Great post. I was checking continuously this blog and I’m impressed! Extremely helpful info specifically the last part 🙂 I care for such info a lot. I was seeking this certain information for a very long time. Thank you and good luck.
What’s up Dear, are you really visiting this site regularly, if so afterward you will definitely obtain nice experience.
Thanks for ones marvelous posting! I genuinely enjoyed reading it, you could be a great author. I will be sure to bookmark your blog and will come back sometime soon. I want to encourage you to ultimately continue your great job, have a nice weekend!
I think everything published made a lot of sense. However, what about this? suppose you added a little information? I ain’t saying your content is not good., but suppose you added a title that makes people want more? I mean %BLOG_TITLE% is kinda plain. You should look at Yahoo’s home page and see how they create post titles to grab people interested. You might add a related video or a related pic or two to get readers interested about everything’ve written. In my opinion, it could bring your blog a little livelier.
This is really interesting, You’re a very skilled blogger. I have joined your rss feed and look forward to seeking more of your great post. Also, I have shared your web site in my social networks!
I blog often and I truly thank you for your content. This article has really peaked my interest. I’m going to take a note of your site and keep checking for new details about once a week. I opted in for your Feed as well.
Wow, incredible blog structure! How long have you ever been running a blog for? you made running a blog glance easy. The total glance of your website is great, let alone the content!
Its such as you learn my mind! You appear to understand so much about this, such as you wrote the e-book in it or something. I believe that you can do with some p.c. to force the message house a bit, however instead of that, this is great blog. A fantastic read. I’ll certainly be back.
After looking at a number of the articles on your site, I really appreciate your technique of blogging. I book marked it to my bookmark site list and will be checking back soon. Please check out my web site as well and tell me what you think.
Почему нельзя брить кошек налысо? https://e-pochemuchka.ru/pochemu-nelzya-brit-koshek-nalyso/
I’m excited to discover this great site. I need to to thank you for ones time for this particularly wonderful read!! I definitely savored every part of it and I have you book marked to see new information in your site.
Appreciate the recommendation. Will try it out.
кредит под птс грузового автомобиля
http://www.hucellbio.com/bbs/board.php?bo_table=free&wr_id=456998
кредит под птс мотоцикла
https://progorodsamara.ru/interesnoe/view/zajm-pod-pts-v-avtolombarde-vygodnoe-resenie-finansovyh-problem
интимный магазин для взрослых
https://vkontakte.forum.cool/viewtopic.php?id=17332
It’s genuinely very complicated in this active life to listen news on Television, so I simply use world wide web for that purpose, and get the newest news.
автоломбард залог автомобиля
http://web.symbol.rs/forum/member.php?action=profile&uid=683640
I am extremely impressed with your writing skills as well as with the layout on your blog. Is this a paid theme or did you customize it yourself? Anyway keep up the excellent quality writing, it’s rare to see a great blog like this one nowadays.
автоломбард
https://50baksov.ru/kak-otkryt-avtolombard-poshagovoe-rukovodstvo/
интимные товары купить
https://asktourist.ru/viewtopic.php?id=5503
I really like reading a post that can make men and women think. Also, thanks for allowing for me to comment!
I do believe all of the ideas you’ve introduced on your post. They are very convincing and will certainly work. Still, the posts are too brief for beginners. May just you please prolong them a bit from subsequent time? Thanks for the post.
If you would like to get a good deal from this paragraph then you have to apply such techniques to your won website.
Appreciate this post. Will try it out.
рассчитать кредит под залог авто
http://misstres.ru/forum/profile.php?action=show&member=7311
кредит залог авто
https://www.smolnews.ru/news/750754
каталог товаров интим магазина
http://che.best-city.ru/forum/thread88974/
Thanks for the auspicious writeup. It in reality used to be a entertainment account it. Glance complicated to far added agreeable from you! By the way, how can we keep in touch?
автоломбард процент
http://www.daongil.com/bbs/board.php?bo_table=free&wr_id=306071
кредит под залог авто
https://remkam.ru/kredit-pod-zalog-avtomobilya-v-avtolombarde-vse-chto-vam-nuzhno-znat/
Hi are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and set up my own. Do you need any html coding expertise to make your own blog? Any help would be really appreciated!
магазин интим товаров в москве
https://asktourist.ru/viewtopic.php?id=5503
реалистичная секс кукла купить в москве
https://sex-shop-domzhelanij.ru
секс кукла купить цена
https://sexshop-domzhelnij.ru
купить секс куклу силикон
https://sexy-dolls-msk.ru
купить секс куклу для взрослых
https://sex-shop-domzhelanij.ru
купить секс куклу с доставкой
https://sexshop-domzhelnij.ru
купить секс куклу с доставкой
https://sexy-dolls-msk.ru
купить самую реалистичную секс куклу
https://sex-shop-domzhelanij.ru
купить секс куклу для взрослых
https://sexshop-domzhelnij.ru
реалистичная секс кукла купить в москве
https://sexy-dolls-msk.ru
Have you ever faced the issue of your credit report unexpectedly “declares” you dead? Encountering an erroneous death marker in your TransUnion credit report can be a significant ordeal for anyone. This mistake not only induces anxiety and stress but can also have long-term consequences for your financial life, affecting your ability to obtain loans, insurance, and even employment.
Grasping the Severity of the Situation
The erroneous listing of you as deceased in TransUnion’s databases is not just a small oversight. It’s a mistake that can block your access to the most critical financial tools and services. It’s crucial to realize that behind this “digital” problem lie real-life inconveniences and obstacles, such as issues with the social security administration death index and wrongful denial of coverage.
Overview of Statistics
Let’s consider some statistics that illustrate the prevalence of the problem. For instance, credit bureau reports deceased and social security administration death notification errors occur frequently. Experian death notification and Equifax death notice errors are also common.
These figures underscore the importance of timely detecting and correcting such errors. If you find your credit report says I am deceased or your credit report shows deceased, immediate action is required.
Benefits of Choosing Our Law Firm
Choosing our company to solve your problem with your credit report is a choice in favor of professionalism and reliability. Thanks to deep knowledge of the FCRA law and experience in handling similar cases, we offer you the following benefits:
Guarantee of no expenses on your part: the costs of our services are borne by the respondent.
Numerous satisfied clients and substantial compensations confirm our effectiveness.
We take on all the work of interacting with credit bureaus and protecting your interests.
Real-Life Problems Encountered by People
Mistakenly reported as deceased TransUnion – denials of credit and financial services.
Credit report is showing deceased TransUnion – problems with insurance applications and insurance company refusal to pay.
Flagging TransUnion account as deceased – difficulties with employment due to background check errors.
TransUnion deceased alert – inability to sign financial contracts, leading to insurance claim denial and long-term care claim lawyer consultations.
These issues not only create financial and emotional difficulties but also undermine your trust in the credit monitoring system. When errors like a deceased indicator on credit report occur, it’s essential to have an experienced insurance attorney on your side to navigate the complexities.
Have you been mistakenly reported as deceased on credit report? Are you dealing with a social security number reported as deceased or credit report deceased errors? Our firm specializes in resolving these issues, ensuring your records are corrected swiftly. Contact us to enforce insurance promises and get your financial life back on track.
If your credit report says I am deceased, don’t wait. Our experienced team can help you prove you are not deceased and address inaccuracies such as deceased indicator meaning and credit bureau reports deceased. Trust us to handle your case with the dedication of a skilled insurance lawyer.
https://bucceri-pincus.com/equifax-consumer-deceased/
товары взрослых эротические
https://otvet.mail.ru/answer/2057759557
There is many books and documentaries and information out there on how to prevent and treat cancer naturally.
VIPPS checks pharmacies for proper storage of their lyrica addiction less respected than men who don’t use it?
Infections caused by HSV1 are less likely to recur in the genital area than infections caused by HSV2.
Возможные причины проблемы с переходом по ссылкам в Telegram
https://imzhpro.ru
Почему работают только одни беспроводные наушники и как это исправить
https://insurance-direct.ru
Причины зависти к Тому Сойеру и Геку Финну
https://imzhpro.ru
The presence of persistent symptoms was evaluated in all individuals and a psychological assessment was performed.
You can always find it online and the price of prednisone for rash dosage isn’t working, should I quit taking the drug?
View all posts by John M.
Основные причины отсутствия звука ВКонтакте
https://insurance-direct.ru
Почему бьет током машина
https://imzhpro.ru
Путь очарованного странника: главные вехи судьбы Ивана Флягина
https://insurance-direct.ru
In many cases you may not know the name of the ailment and do not know where to look to find out about it.
providersPreventing errors is your responsibility when you glucophage smoking . Get one now! You can’t find more affordable prices.
The entire procedure is performed through four to five small incisions in the abdominal wall.
Hi i have irregular periods…i missed my period las mth d end of june…i had unprotected sex for the week from11th of july…i startd hvin cramps which i dont hav when i am on my periods, i am going off regular and sometimes constipated, my nipples hurt…am i pregnant?
There are several ways to buy ampicillin sulbactam spectrum of activity and manage your health problem
Even then, we focus mostly on the pain, not the internal healing process.
секс кукла купить цена
https://sex-shop-domzhelanij.ru
автоломбард птс https://avtolombard-novosibirsk.ru займ под птс
оформить кредит под залог авто https://avtolombard-pod-pts-nsk.ru деньги в кредит под залог машины
деньги под птс автомобиля новосибирск https://credit-pod-zalog-pts.ru кредит в залог автомобиля
оформить займ под птс https://novosib-zalog-pts.ru деньги в долг под залог машины
купить поролон для мебели
деньги в долг под птс https://zaim-pod-pts-nsk.ru кредит под залог машины не лишаясь ее
“Hi everyone! I’ve been thinking about getting my shaft balanced on my car. I found this post , and it got me questioning, should I bother?
It’s a costly service. Maybe it’s easier to just drive as is, and just change the shaft occasionally. Or is the vibration truly damaging that it’s worth the cost?”
Article : Shaft imbalance
займ под залог авто в новосибирске https://avtolombard-novosibirsk.ru деньги под птс круглосуточные
автоломбард залог птс новосибирск https://avtolombard-pod-pts-nsk.ru кредит в залог автомобиля
займ под птс без посещения офиса https://credit-pod-zalog-pts.ru взять деньги под птс
кредит под залог авто проценты https://novosib-zalog-pts.ru займ залог авто взять
деньги под птс круглосуточные https://zaim-pod-pts-nsk.ru деньги под залог птс автомобиля
получить займ под залог авто https://avtolombard-novosibirsk.ru кредит под залог авто новосибирск
займ под залог авто в новосибирске https://avtolombard-pod-pts-nsk.ru автоломбард залог
займ под залог кредитного авто https://credit-pod-zalog-pts.ru займ под залог птс авто
займ под залог авто круглосуточно https://novosib-zalog-pts.ru автоломбард под залог
деньги под залог авто птс https://zaim-pod-pts-nsk.ru кредит под птс с плохой кредитной
займ под залог птс новосибирск https://avtolombard-novosibirsk.ru взять займ под залог птс
займ под залог авто с правом пользования https://avtolombard-pod-pts-nsk.ru получить деньги под залог птс
кредит под птс новосибирск https://credit-pod-zalog-pts.ru кредит под залог кредитного авто
займ залог авто взять https://novosib-zalog-pts.ru кредит под птс мотоцикла
Personally I over it’s nonsense, my view of myself has no deportment on anything except for people trapped in a union that obsesses about relative rank.
But you can unendingly observant of new movies for free to the Internet.
кредит под залог машины не лишаясь ее https://zaim-pod-pts-nsk.ru займ под залог машины
I toughened to live not far from the Beit Hanoun and when infernal regions fell from happy isles I was luckier than the people who lived there.
My name is مجاهد‎., I am a fugitive and I am raising loot to help.
Please if you can send a dollar saved to a Bitcoin purse, do so. I require try to send funds for humanitarian uphold to the victims in the Gaza Strip.
Bitcoin(BTC): bc1q4x8s3uw6gq67sakst5ngqcznznvwmzv8p6ktpr
Ethereum (ETH): 0xD236413ee5E9c1DBDdE2012595d4A3C38418C3bf
If you can’t send funds, entertain don’t delete this declaration or send it to SPAM. Prefer forward it to those who can send at least 1 dollar.
كنت أعيش في مكان ليس ببعيد عن Ш№ШЁШіШ§Щ† Ш§Щ„ЩѓШЁЩЉШ±Ш©، وعندما سقطت الجحيم من السماء كنت أكثر حظًا من الناس الذين يعيشون هناك.
اسمي مهاجر‎، أنا لاجئ وأقوم بجمع التبرعات للمساعدة.
من فضلك إذا كان بإمكانك إرسال الدولار الذي تدخره إلى محفظة بيتكوين، فافعل ذلك. سأحاول إرسال الأموال للمساعدات الإنسانية للضحايا في قطاع غزة.
Bitcoin(BTC): bc1q4x8s3uw6gq67sakst5ngqcznznvwmzv8p6ktpr
Ethereum (ETH): 0xD236413ee5E9c1DBDdE2012595d4A3C38418C3bf
إذا لم تتمكن من إرسال الأموال، يرجى عدم حذف هذه الرسالة أو إرسالها إلى الرسائل الاقتحامية. يرجى إرسالها إلى أولئك الذين يمكنهم إرسال دولار واحد على الأقل.
рассчитать кредит под залог авто https://avtolombard-novosibirsk.ru кредит под залог авто документы
Алкоголь и боль в мышцах связаны! ?? Разбираемся, как спиртное влияет на мышечную ткань и почему после застолья все болит. ?? https://kladovaya-znanij-2.ru/pochemu-posle-alkogolya-bolyat-myshtsy/ Почему после алкоголя болят мышцы
Неужели до сих пор не ясно, как легко и быстро купить Apex Coins и боевой пропуск для различных популярных игр? Ведь на этом сайте предлагается простой и удобный процесс активации ключей, позволяющий вам получить желаемую игровую валюту даже без лишних усилий. Почему тратить время на долгие поиски, если всё, что вам нужно, уже собрано в одном месте?
Apex Legends — одна из лучших игр на рынке, и получить Apex Coins понятным и безопасным способом теперь проще простого. Никаких сложных шагов. Вам просто нужно активировать свой код в EA App и ваш аккаунт уже будет наполнен необходимыми монетами. Это не просто удобство — это ваша возможность одержать преимущества в игре без лишних затрат времени и нервов. Достаточно взять свой код, активировать его и начать пользоваться всеми преимуществами, которые вам дают эти монеты.
Обращаясь к многочисленным играм, таким как PUBG Mobile, Genshin Impact, Valorant и другим, заметно, что все они имеют свою систему внутриигровой валюты. Этот сайт призван решить проблему доступа к ней, предлагая вам выгодные скидки на популярные сервисы. Скидки в размере 5% на Zenless Zone Zero и до 14% на Steam USD — это реальная выгода. Зачем переплачивать, если есть возможность приобрести то, что вам нужно, за меньшие деньги?
Важно понимать, что сайт не просто поставщик игровых кодов. Он предоставляет гарантию безопасности и поддержку пользователям — это действительно важно. Каждый, кто сталкивался с проблемами активации или пополнением счёта, знает, насколько раздражающим это может быть. Но благодаря удобной форме техподдержки на сайте, ваши вопросы будут отвечены быстро и оперативно. Вы также можете следить за новостями через Telegram и ВК, что делает процесс максимально прозрачным и удобным.
Адекватный сервис пополнения аккаунтов в таких странах как Киргизия, где расположен данный бизнес, служит свидетельством того, что в сфере цифровых развлечений доверие и доступность имеют первостепенное значение. Не упустите свой шанс получить игровые ресурсы по выгодным ценам и без лишней головной боли. Разобраться со своим игровым аккаунтом, активировать код и насладиться игрой — это всё, что вам нужно. Избавьтесь от сомнений и воспользуйтесь предложением, которое явно выделяется на фоне множества посредников и услуг.
купить apex coins
Тянет или колет живот при беременности? ?? Разбираемся в причинах боли: от естественных процессов до поводов обратиться к врачу. Узнайте, когда это неопасно! https://kladovaya-znanij-3.ru/prichiny-boli-v-zhivote-pri-beremennosti/ Причины боли в животе при беременности
У кошки рвота желчью? Не паникуйте! Узнайте о причинах рвоты желтой жидкостью у кошек и получите советы по лечению. https://kladovaya-znanij-4.ru/pochemu-kota-rvet-zheltoy-zhidkostyu/ Почему кота рвет желтой жидкостью
Разбираемся в хитросплетениях русской пунктуации! Узнайте, как правильно ставить знаки и писать грамотно, чтобы ваши тексты всегда были понятны и приятны для чтения. https://kladovaya-znanij-2.ru/rol-i-znachenie-punktuatsii-v-russkom-yazyke/ Роль и значение пунктуации в русском языке
?? Не знаете, почему пропала тяга в печи? ?? Рассказываем о самых частых причинах, от засора дымохода до проблем с вентиляцией. ?? Вернём тепло в ваш дом! https://kladovaya-znanij-3.ru/prichiny-otsutstviya-tyagi-v-pechke/ Причины отсутствия тяги в печке
Узнайте о частых причинах низкого гемоглобина у мужчин, включая хронические желудочно-кишечные кровотечения. Не игнорируйте свое здоровье! https://kladovaya-znanij-4.ru/prichiny-nizkogo-gemoglobina-u-muzhchin/ Причины низкого гемоглобина у мужчин
Зачем переезжали столицы? Безопасность, экономика, символизм… История полна примеров от Рима до Бразилиа! Узнайте о самых ярких https://kladovaya-znanij-2.ru/prichiny-perenosa-stolits-v-istorii/ Причины переноса столиц в истории
Почему глаза двигаются во сне, особенно быстро и хаотично? Разгадаем загадку REM-фазы и узнаем, о чем говорят движения глаз под закрытыми веками. ?? https://kladovaya-znanij-3.ru/pochemu-glaza-dvigayutsya-vo-sne/ Почему глаза двигаются во сне
Узнайте о причинах образования камней в почках, таких как недостаток воды, и о том, как предотвратить их появление. Симптомы, диагностика и методы лечения. https://kladovaya-znanij-4.ru/prichiny-poyavleniya-kamney-v-pochkah/ Причины появления камней в почках
1win ставки
купить в москве силиконовую секс куклу
https://e-sex-blog-info.ru
купить в москве силиконовую секс куклу
секс куклы купить 18
https://infosex-blog-info.ru
купить секс куклу с доставкой
купить секс куклу с доставкой
https://plus-sex-blog-info.ru
купить секс куклу силикон
купить секс куклу dolls
https://sex-blog-info.ru
купить секс куклу с доставкой
купить секс куклу силикон
https://e-sex-blog-info.ru
купить секс куклу в полный рост
These biopsies are usually performed as an outpatient procedure.
You can easily go online to check the how quickly does lisinopril lower blood pressure at low prices from qualified pharmacies
You could be ovulating, but are you on bc?
секс куклы купить 18
https://infosex-blog-info.ru
секс кукла купить цена
Повысьте доверие и привлеките клиентов с нашим добровольным сертификатом соответствия! Наличие сертификата соответствия позволяет клиентам быть уверенными в том,
что они приобретают безопасный и надежный продукт – декларация соответствия гост р.
реалистичная секс кукла купить в москве
https://plus-sex-blog-info.ru
секс куклы купить 18
Содержание статьи
• Проверка информации о компании «Эсперио»
• Не дайте мошенникам присвоить свои деньги!
• Адрес и стаж как признаки мошенничества Esperio
• Чарджбэк для возврата средств на карту
• Отзывы о «Эсперио»
• Схема развода «Эсперио»
• Заключение
На первый взгляд у компании приличный мультиязычный сайт, а также достаточное количество юридической и прочей информации. Однако стоит начать всерьёз проверять легенду «Эсперио» — как она начинает рассыпаться на глазах.
«Вся Правда» приглашает разобрать компанию по косточкам, заодно потренировавшись выводить подобных лжеброкеров на чистую воду.
Проверка информации о компании «Эсперио»
Кладезем базовых юридических данных являются документы и футер сайта, заполненный очень мелким, слепым шрифтом. Поэтому удобнее обращаться к разделу «Правовая информация», который сослали на третий уровень интернет-ресурса, в категорию «О компании».
Первое, что бросается в глаза в этой самой правовой информации, это отсутствие обоих ключевых для каждого брокера документов:
1. скан-копии свидетельства о регистрации,
2. бланка лицензии на брокерскую деятельность.
Это настораживающий фактор, который сразу понижает степень доверия к Esperio. А ключевые сведения будем выяснять самостоятельно, перепроверяя отрывочную информацию из футера официального сайта и из шапки клиентского соглашения.
Итак, заявлено, что сайтом управляет компания OFG Cap. Ltd с регистрацией на Сент-Винсент и Гренадинах. Это островное офшорное государство давно является прибежищем сомнительных компаний, которые покупают местную регистрацию по вполне доступной цене. Однако для этого нужно предпринять хотя бы минимальный набор действий и подать скромный пакет документов.
Не дайте мошенникам присвоить свои деньги!
Узнайте, как обезопасить свои финансы
Подробнее
Проверить, было ли это сделано на самом деле, легко. Достаточно на сервисе info-clipper или подобном агрегаторе юридических лиц разных стран мира выбрать интересующее государство и ввести название компании. Если результат не найден, значит, такого юрлица в стране не зарегистрировано. Показываем на скриншоте, что брокер лжёт о своей якобы материнской компании (хотя формулировка про управление сайтом не тянет даже на подобный статус). Компания Esperio на островах также не зарегистрирована.
Далее, у брокера обязана быть лицензия на данный вид деятельности. Её выдают финансовые государственные регуляторы: подробнее об этой системе полезно прочитать в соответствующей статье нашего блога. В островном офшоре есть собственный финансовый госрегулятор под названием Financial Services Authority. Самый надёжный и при этом простой способ проверки наличия лицензии следующий: зайти на официальный сайт регулятора и ввести название компании в поиск. Результат отрицательный: ни OFG Cap. Ltd, ни Esperio в FSA не лицензировались. Так что компания не имеет разрешения на финансовую деятельность даже в заявленной стране регистрации, которая, впрочем, тоже оказалась фейковой.
Впрочем, даже в случае легального оформления юрлица и лицензирования по месту регистрации этого недостаточно для работы в правовом поле Российской Федерации. Оказывать брокерские услуги в стране можно исключительно по лицензии Центробанка РФ. Российский регулятор, как и все его иностранные коллеги, призван способствовать прозрачности рынка и ведёт открытые реестры держателей своих допусков и чёрные списки. Поиск по реестрам на сайте ЦБ РФ показывает, что брокер Esperio ему знаком. Он загремел в чёрный список компаний с признаками нелегального профучастника рынка ценных бумаг. Этот корректный термин обозначает лохоброкера: всё-таки не полагается почтенному государственному регулятору такую терминологию использовать.
Обратите внимание на сайты, перечисленные на скриншоте из чёрного списка Центробанка РФ. Видно, что мошенники часто запускают зеркала своего сайта. Этому может быть только одна причина: их блокировка за мошенничество для российских пользователей, которые являются основной целевой аудиторией лжеброкеров.
На момент написания обзора провайдеры РФ пока не перекрыли доступ к. Однако, судя по активности лохоброкера, и эта мера не за горами.
Адрес и стаж как признаки мошенничества Esperio
В ходе проверки информации о компании «Вся Правда» также рекомендует пробивать заявленный на её интернет-ресурсе адрес. Хотя бы через поисковые системы и, особенно, через Гугл-карты. Такой простой метод позволяет отсечь вымышленные координаты, которыми часто прикрываются мошенники, а также полюбоваться на заявленные места головных офисов. Этот простой метод не подвёл и с «Эсперио».
В футере сайта, а также в шапке клиентского договора указан один и тот же адрес на Сент-Винсент и Гренадинах: First Floor, First St. Vincent Bank Ltd Building, James Street, Kingstown. Здание действительно существует, и оно напрямую связано с финансовой системой. Находится в нём ровно то, что мошенники не удосужились вычистить из адреса: First St. Vincent Bank Ltd Building. То есть главный банк страны.
Несмотря на миниатюрность учреждения в карликовом государстве, офшорный банк не бедствует и уж точно не докатился до сдачи в аренду первого этажа здания всяческим проходимцам. Банкам по любым протоколам безопасности запрещается делить помещения с любыми арендаторами, поскольку это создаёт дополнительную уязвимость.
купить секс куклу dolls
https://prosex-blog-info.ru
купить секс куклу в полный рост
Nathan is a professor of medicine at Harvard Medical School and director of the General Clinical Research Center and of the Diabetes Center at Massachusetts General Hospital.
out the substantial discounts quoted through this site for doxycycline monohydrate 100mg remain in my system?
Pap tests are reported as no abnormal cells, abnormal cells of undetermined significance, low risk abnormal cells or high risk abnormal cells.
секс куклы купить 18
https://sex-blog-info.ru
купить секс куклу для взрослых
купить самую реалистичную секс куклу
https://e-sex-blog-info.ru
купить секс куклу силикон
купить в москве силиконовую секс куклу
https://infosex-blog-info.ru
купить секс куклу в полный рост
This opening often locks up soon after birth.
More offers at what is valtrex for at consistently low prices
David HP, Dytrych Z, Matecek Z, Schuller V eds : Born Unwanted: Developmental Effects of Denied Abortion.
Postmenopausal women — Postmenopausal women who develop recurrent bladder infections may benefit from using vaginal estrogen.
Amazing savings on flagyl tablet about your problem.
There are two three of radiation treatment:Radiation therapy might be used for the breast area, lymph nodes, or another part of the body and generally is used after breast cancer surgery.
купить силиконовую секс куклу
https://plus-sex-blog-info.ru
купить реалистическую секс куклу
купить силиконовую секс куклу
https://prosex-blog-info.ru
купить секс куклу dolls
купить секс куклу dolls
https://sex-blog-info.ru
купить недорогую силиконовую секс куклу
The experienced veterinarians at Germantown Vet can examine and diagnose your dog so a treatment plan can be created.
for your insurance problems.How can I tell if a clomid vs nolvadex pct at exceptionally low prices if you order from online pharmacies
The blood test that is mainly used to keep a check on your blood glucose level is called the HbA1c test.
Highly eenergetic post, I enjoyeed that a lot. Willl there bee
a part 2?
These statistics include adults and children and include renal cell carcinoma and transitional cell carcinoma of the renal pelvis.
Are men who use is cephalexin safe for pregnancy online.Easeus Deleted File Recovery – CNET Download. Disk
ResourcesResourcesNational Comprehensive Cancer NetworkThe National Comprehensive Cancer Network is a nonprofit alliance of 21 cancer centers throughout the U.
But many of those are pregnant women and those born with red blood cell diseases.
Be sensitive about ED patients. keflex medicine on the Internet.
Number of comorbid medical conditions was the independent variable, lifetime and 12-month MDD were dependent variables, and age, gender, education, marital status, employment, and body mass index were covariates.
But no symptom should be ignored or overlooked, especially if it has lasted a long time or is getting worse.
People with low incomes are likely to what is neurontin used for remains in my system too long, should I be worried?
OMG………………………………………your hard work is mmmmmmmmmmmmmmmmmuch appreciated Carl!!!!!!!!!!!!
I visited multiple web sites however the audio
quality for audio songs current at this web site is truly superb.
вакуумный помпа купить в москве
https://sex-blog-info.site
большие вагинальные шарики
анальная пробка
https://sex-blog-info.space
вагинальные вибрационные шарики
секс игрушка вагина
https://sex-blog-info.website
интим товары 18
интим товары сайт
https://sex-blog-info.fun
клиторальный стимулятор секс
вагинальные шарики 18
https://sex-blog-info.online
эротическое белье купить
лубрикант на водной основе купить москва
https://sex-blog-info.site
вакуумный помпа купить в москве
анальный вибратор массажер простаты
https://sex-blog-info.space
интим магазин для мужчин
вибратор купить интернет
https://sex-blog-info.website
интим товары 18
набор вагинальных шариков
https://sex-blog-info.fun
вакуумная помпа для полового члена купить
It’s actually a cool and helpful piece of information. I am happy that you simply shared this helpful info with us. Please stay us informed like this. Thanks for sharing.
Hey there! I just wanted to ask if you ever have any issues with hackers? My last blog (wordpress) was hacked and I ended up losing several weeks of hard work due to no backup. Do you have any solutions to prevent hackers?
фаллоимитатор купить цены
https://sex-blog-info.site
эрекционное кольцо
Hi, Neat post. There is a problem with your web site in web explorer, would check this? IE still is the market leader and a huge component to other folks will miss your magnificent writing due to this problem.
помпа для клитора
https://sex-blog-info.space
массажер простаты цена купить
купить реалистическую секс куклу
https://sex-blog-info.website
купить фаллоимитатор
секс кукла купить цена
https://sex-blog-info.fun
вагина купить 18
Oh my goodness! Incredible article dude! Thank you, However I am having troubles with your RSS. I don’t know why I am unable to subscribe to it. Is there anybody else having similar RSS issues? Anyone that knows the solution will you kindly respond? Thanks!!
безременной страпон купить
https://sex-blog-info.online
купить секс куклу для взрослых
интимные товары вибратор
https://sex-blog-info.site
женская анальная пробка
Great blog here! Also your website loads up fast! What web host are you using? Can I get your affiliate link to your host? I wish my website loaded up as fast as yours lol
анальные пробки вибратор бдсм
https://sex-blog-info.space
виброяйцо 18
секс-шоп
https://sex-blog-info.website
купить мини секс машину
Hello, yeah this piece of writing is actually good and I have learned lot of things from it regarding blogging. thanks.
Somebody essentially lend a hand to make severely posts I would state. This is the first time I frequented your web page and to this point? I surprised with the research you made to create this actual submit incredible. Wonderful process!
Howdy, I do believe your site might be having internet browser compatibility issues. Whenever I take a look at your blog in Safari, it looks fine however, when opening in IE, it has some overlapping issues. I simply wanted to give you a quick heads up! Besides that, excellent blog!
Hey there! Someone in my Facebook group shared this site with us so I came to give it a look. I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my followers! Excellent blog and amazing style and design.
Actually when someone doesn’t be aware off aftr thast its
uup tto other peoople thatt they wilpl help, so hesre it
taes place.
Oh my goodness! Incredible article dude! Many thanks, However I am going through difficulties with
your RSS. I don’t know the reason why I can’t join it.
Is there anyone else having the same RSS issues? Anybody who knows
the answer can you kindly respond? Thanx!!
And then the next morning the consultant came in and said, ‘We’re sorry we’ve, we know that your white count’s elevated but we don’t actually know what’s wrong.
Does a health problem need to be treated with sildenafil heartburn and save quite a bit of money
Red blood cells contain the protein hemoglobin, which is vital to carrying…
Ocular herpes is a recurrent infection that affects the eyes.
Wise people will purchase a canadian pharmacy sildenafil misconceptions about online ordering. Don’t be ignorant, read
After feeding her Beneful, she got sick, and she was unable to control her bowels.
Archetyp market
https://github.com/Archetyp-Market/Archetyp
Hi there it’s me, I am also visiting this web page regularly, this web site is actually fastidious and the visitors are actually sharing nice thoughts.
Hey there! I could have sworn I’ve been to this site before but after checking through some of the post I realized it’s new to me. Anyhow, I’m definitely happy I found it and I’ll be book-marking and checking back frequently!
глаз бога бот
https://glazb.me
глаз бога телеграмм
глаз бога
глаз бога телеграм
глаз бога тг бот
https://glazb.me
глаз бога телеграм
I was extremely pleased to uncover this site. I want to to thank you for your time due to this fantastic read!! I definitely loved every bit of it and I have you book-marked to look at new stuff in your site.
глаз бога телеграм
глаз бога бот
I don’t know if it’s just me or if everyone else experiencing issues with your website. It appears as if some of the text within your content are running off the screen. Can somebody else please provide feedback and let me know if this is happening to them as well? This may be a issue with my internet browser because I’ve had this happen before. Thanks
I think the admin of this site is truly working hard for his site, because here every data is quality based stuff.
Very nice article, totally what I wanted to find.
Fantastic blog! Do you have any helpful hints for aspiring writers? I’m planning to start my own website soon but I’m a little lost on everything. Would you recommend starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m completely overwhelmed .. Any ideas? Thanks!
I am genuinely happy to glance at this website posts which consists of plenty of useful data, thanks for providing such data.
I really like your blog.. very nice colors & theme. Did you create this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to create my own blog and would like to find out where u got this from. thanks a lot
thank you very much
_________________
как пишется рассказик
The spa center happy ending calls visit one of the ways massage, is what we do. What is an sports massage interested in everyone. Prostate massage it’s a craftsmanship of giving for bliss. You willextremely surprised to that,what ocean enjoyment can experience from adopting massage. In studio Workshop classical massage women will hold sexual swedish massage.
How is it done, and is there something exotic? We will tell you all about him that you wanted to know |Our Change roles massage is visited not only by men but also by women, and also by couples. You want to use only this infinitely … Our primary а task this is to please you wonderful sensual best massage. Individual approach to all yours requirements and conditions.
The beautiful girls our the spa salon will give you an unforgettable experience. The salon is a place of rest and relaxation. Like Bamboo Erotic Massage, as though, and relaxation, influences on specific area naked body, this allows clients gain strength. Stop your choice not on one masseuse, choose two girls! Choose for yourself massezha what I liked, both professional and professional abilities!
Our salon in New York we advise stunning premises with comfortable design. Data placement help be you you are staying with us not attracting the attention of other customers.
We have a showroom in Uptown Beauties Brooke :
sensual massage manhattan
He says there is no proof that they better your results, but does…
Everyone can lexapro drug class for serious help
The person is evaluated or referred to a health care provider within 1 month.
Добрый, посоветуйте покупать ли казино? Думаю или будет с сайта доход? Продают его на главной странице этого сайта
как работает поддержка на сайте казино
Показывают они как работать с админ панелью казино
Как считаете играть люди будут если открыть свое онлайн казино?
Warfarin is the foundation for long-term treatment of DVT and PE and is essential for the prevention of stroke from atrial fibrillation7 and for prevention of clotting in mechanical heart valves.
Wise people will purchase a does lasix increase bun and creatinine at a cheaper price?
Two types of radiotherapy are used for mouth cancer: external and internal.
Переходите на сайт с самым выгодным казино онлайн – https://bestslots-online777.com/
Sorry, there was a problem.
Has your stromectol uk at incredibly low prices when you purchase from discount
Sood said she recommends people who are diagnosed with Type 2 diabetes lose at least five to 10 percent of their current body weight.
It is a chronic medical condition, at which blood pressure in arteries are elevated.
When seeking a highly effective remedy, you always want to buying zithromax . ED problems quickly resolved!
Victorian Government Department of Health.
Signs of the illness usually appear between ages 40 to 60, but some people show symptoms as early as 20.
Pay lower prices when you bactrim in pregnancy at low prices, you need to compare online offers
It is a new way of losing weight, more notably losing that stubborn weight you can’t seem to get rid of.
I was diagnosed with Scleritis of both eyes in 1990.
Be sensitive about ED patients. amoxicillin over the counter brand and generic product?.
Now, medical experts have devised an online symptom checker to try and help the general public understand what their symptoms may indicate.
Thanks for finally talking about > %blog_title% < Liked it!
Everything is very open with a really clear clarification of the issues. It was really informative. Your website is very useful. Thank you for sharing!
Hi everyone, it’s my first go to see at this web site, and paragraph is really fruitful for me, keep up posting such articles.
Everything is very open with a clear explanation of the issues. It was truly informative. Your website is useful. Thanks for sharing!
Thanks you…
https://hop.cx/airdrop
I couldn’t refrain from commenting. Well written!
I take pleasure in, result in I found just what I used to be looking for. You have ended my 4 day lengthy hunt! God Bless you man. Have a nice day. Bye
This design is incredible! You definitely know how to keep a reader amused. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job. I really loved what you had to say, and more than that, how you presented it. Too cool!
With havin so much content do you ever run into any problems of plagorism or copyright infringement? My site has a lot of unique content I’ve either authored myself or outsourced but it seems a lot of it is popping it up all over the internet without my agreement. Do you know any ways to help protect against content from being ripped off? I’d definitely appreciate it.
I believe everything published made a great deal of sense. However, what about this? what if you were to write a awesome post title? I mean, I don’t wish to tell you how to run your website, but suppose you added a headline that grabbed a person’s attention? I mean %BLOG_TITLE% is kinda boring. You might peek at Yahoo’s front page and see how they write news headlines to get viewers to click. You might add a related video or a pic or two to grab people excited about everything’ve written. In my opinion, it might bring your posts a little bit more interesting.
Definitely believe that which you stated. Your favorite reason appeared to be on the web the simplest thing to be aware of. I say to you, I certainly get irked while people consider worries that they just don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side effect , people could take a signal. Will likely be back to get more. Thanks
Ваш лазерный принтера требует заправки картриджа? Превратите расходы на новые картриджи в экономию с нашей услугой по заправке картриджей лазерных принтеров в Киеве!
Наша команда мастеров гарантирует профессиональное обслуживание вашего принтера или МФУ, используя только высококачественные расходные материалы. Забудьте о незаконченных печатных заданиях и переплате за новые картриджи – с нашим сервисом вы экономите свои ресурсы!
Заправить картридж лазерного принтера Киев – https://printershub.com.ua/ru/zapravka-kartridzha
Не теряйте время и деньги – доверьтесь профессионалам от ПринтерсХаб!
Genuinely when someone doesn’t know after that its up to other users that they will assist, so here it takes place.
It’s appropriate time to make some plans for the long run and it’s time to be happy. I have read this publish and if I could I desire to suggest you few interesting issues or suggestions. Maybe you can write subsequent articles relating to this article. I desire to read more issues about it!
Little Restaurant Building Company
Our tiny dining establishment building and construction firm delivers high-grade building services tailored to your demands. We develop restaurants that attract customers and support your procedures.
I was wondering if you ever thought of changing the page layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two pictures. Maybe you could space it out better?
I think the admin of this site is genuinely working hard in favor of his website, since here every information is quality based stuff.
BE A MATCH FOR GRAPHICS CARDS AND PROCESSORS HEAD TO FACULTY! The impressive detestation is the following:
– Can GPU be adapted to for the sake of calculations?
– Is GPU calculate faster than CPU?
– Is a GPU peer to a CPU?
Also reckon in sight how to find unconfined if the processor is compatible with your GPU. Foremost specifications, results of lay benchmarks, scene rating and reviews on site CPUDebate.]
Darknet Market uk
https://medium.com/@alphabay30/best-dark-web-markets-2024-b331715a4a77
These medications are prescribed very frequently, and episodes of serious violence, although too common, still are rare compared with the number of people treated.
One of the most popular ways to ivermectin 6mg dosage by taking advantage of discounts
Delusions of being followed or watched are common, as are beliefs that comments, radio or TV programs, etc.
Don’t let stretch marks stand in the way of enjoying your pregnancy and the experienceof new motherhood.
And convenience are the main reasons for buying stromectol 3mg cost for details.
My Doctor swears I have anxiety and depression.
Hi! I understand this is somewhat off-topic but I had to ask. Does managing a well-established website like yours require a massive amount work? I am completely new to running a blog however I do write in my journal on a daily basis. I’d like to start a blog so I can share my own experience and views online. Please let me know if you have any kind of ideas or tips for brand new aspiring blog owners. Thankyou!
Hmm it seems like your website ate my first comment (it was extremely long) so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog. I too am an aspiring blog blogger but I’m still new to the whole thing. Do you have any tips and hints for novice blog writers? I’d definitely appreciate it.
I really like looking through a post that will make people think. Also, many thanks for permitting me to comment!
Hi, I read your new stuff like every week. Your story-telling style is witty, keep doing what you’re doing!
Searching for medical information?
Many pharmaceutical companies see online pharmacy exelon patch at low prices always available through this specialist site
You can help prevent type 2 diabetes by staying at a healthy body weight.
Hi there, its pleasant article on the topic of
media print, we all understand media is a great
source of information.
Nice blog here! Also your web site loads up fast! What host are you using? Can I get your affiliate link to your host? I wish my web site loaded up as quickly as yours lol
I am really impressed with your writing talents and also with the layout in your weblog. Is this a paid subject matter or did you modify it your self? Either way stay up the excellent quality writing, it is rare to look a great weblog like this one nowadays..
Individuals can experience different signs and symptoms of diabetes, and sometimes there may be no signs.
It is important to compare prices, weigh savings, and then british pharmacy online solutions, visit us today!
Psychol Sci 19 1 : 62—9.
For the first time, these products are being made available at nearly the same time that the research results are published in peer-reviewed journals, substantially reducing the gap between research and practice.
Prevention is better than cure for ED. Click this link online pharmacy ativan , is it dangerous for someone else to take my pills?Low rates
Learn to spot the signs of allergies in children to give treatment.
원자재 헬스케어 가격 급등으로 초콜릿이 12
Medical Education AdmissionsSuccessful Applicant ProfileUCSF School of Medicine Office of Admissions, Box 0408 533 Parnassus Avenue, Room U-426 San Francisco, CA 94143 415 476-4044 Office Hours: M-F 8 a.
Fast levitra online pharmacy review dosage isn’t working, should I quit taking the drug?
Dogs with food allergies may also have skin diseases resulting from flea allergies, mold allergies, or parasites.
Uprooting a weed will ensure that the particular weed will never return just as addressing the root of a disease will keep your dog healthy.
out the price reductions on offer when using this site for online mexican pharmacy from professional pharmacies
Where Do I Start??
ПринтСервис – ваш верный партнёр в мире качественной распечатки! Мы даем вам качественную заправку картриджей в Киеве и Вышгороде.
Наши специалисты используют только качественные компоненты для обеспечения оптимального качества печати. Звоните, чтобы наполнить картридж в Киеве и Вышгороде для того чтоб убедится в качестве наших услуг! Ваше удовлетворение – наш главный приоритет.
Заправка картриджей Киев – https://printer.org.ua/ru/zapravka-kartridzhej/
I am regular visitor, how are you everybody? This post posted at this web site is actually nice.
But my clinic did a few blood test 1 which was a BFR Test and my creatinine levels were high I just got the results back it was 160.
Enjoy great online deals and tadalafil 20mg side effects pills by mail or courier to your door. Great service!
Chronic blood loss may be a consequence of the following: cancer gastrointestinal tumors diverticulosis polyposis heavy or frequent menstrual flow hemorrhoids nosebleeds stomach ulcers long-standing alcohol abuse Acute blood loss may occur as a result of injury, a ruptured blood vessel, or a complication of surgery or childbirth.
More about the “The Ten Laws of the Pharmaceutical Industry.
Face off with ED problems and treatment. Contact tadalafil vs sildenafil dosage for all medications are available globallyIf not taken with
Mendel JG, Klein DF.
You’re so interesting! I do not think I’ve truly read anything like that before. So nice to find someone with a few genuine thoughts on this topic. Really.. many thanks for starting this up. This website is one thing that’s needed on the internet, someone with a bit of originality!
It’s remarkable for me to have a website, which is useful in support of my know-how. thanks admin
Stevens, your thyroid panel looks good, but you look awful.
Are men who use acyclovir cream online pharmacy at low prices, you’ll need to compare offers
The treatment team already has funding to treat up to 50 dogs.
I am wishing to treat a 5 year old tinea?
Treat ED now. More details and recommendations at levitra generic cheap , will my partner have any negative feelings?
This does not mean these drugs are causing the potentially violent behavior: People who are prone to acts of violence often are identified as mentally ill prior to the violent event, and often are treated with psychiatric medication.
which is carried out by the printing
малодечная ферма
from a printed book, reproduction
Our neurosurgery and neuroendocrine experts are world leaders in the treatment of pituitary diseases and tumors.
Many replace their trip to the pharmacy by buying buy sildenafil citrate . Also offer free shipping!
Science explains disease, while physicians treat patients.
Reply Cindy says: January 22, 2014 at 11:03 amHow long am i infectious.
Anybody can 50mg sildenafil website is licensed to sell products?
Supportive therapy is the mainstay of management and includes aggressive volume resuscitation and benzodiazepines to ameliorate symptoms.
Селаго.
Цветоводы, специализирующиеся на тепличном хозяйстве, занимаются выращиванием растений в закрытых помещениях – теплицах. Они контролируют идеальные условия для роста и развития растений, такие как температура, влажность, освещение и полив. Цветоводы в тепличном хозяйстве обычно работают с цветами, овощами и другими растениями, чтобы обеспечить их здоровье и оптимальное качество.
можно ли пересаживать цветы в воскресенье
— Евразийский степной пояс — Западная Европа — Центральная и Южная Азия — Северная Америка — Австралия.
Турецкая гвоздика не переносит частых поливов. Поэтому орошать грунтовый слой, на котором она растет, необходимо дважды в 7 дней при условии, что на дворе устойчивая жаркая погода. Полив нужно производить в утреннее и ночное время, используя на 1 м 2 до 20 л жидкости. Превышать рекомендуемый объем воды не стоит, потому что корни подвержены гниению.
Перспективы карьерного роста и возможности развития.
Спасти растение можно путём обработки корней специальными средствами. От тли, паутинного клеща помогает орошение надземной части инсектицидами.
Йеллоу.
It’s normal to worry and to sometimes feel stressed.
Keep saving money when you united healthcare online pharmacy . See how it works!
Electroencephalogram, electromyogram, and Tbr were recorded for 12 h.
Allentuck S, Bowman K.
Do I need a doctor’s prescription to buy viagra cialis levitra from respected online pharmacies if you’d prefer great deals
Influenza viruses are generally divided into three types: A, B and C, of which the two first are of more concern as they cause the most serious illnesses.
The spa center adult calls visit one of the ways massage techniques, is what we do. What is an Lingam massage or penis massage interested in everyone. Buttock Massage this is the gift of giving for enjoyment. You be surprised to that,what variety bliss can experience from adopting massage. In spa center exotic massage masseurs will make sexual adult massage.
How is it done, and is there something exotic? We will tell you all about him that you wanted to know |Our Buttock Massage is visited not only by men but also by women, and also by couples. You necessarily want to rejoice only this infinitely … Our intention this is to please customer awesome sexy relaxing massage. Personal approach to all yours needs and bids.
The amazing women our the spa center will give you an unforgettable experience. The salon is a place of rest and relaxation. The bodywork massage, as in principle, and relaxation, exert influence on some parts naked body, what helps ladies relax. Your best stop choice not on one masseuse, choose two girls! Choose for yourself masseur girl by appearance, both professional and professional proficiency!
Massage center in New York City are ready to provide gorgeous premises with convenient design. Data quarters apply be you you are staying with us incognito.
Our showroom works in Uptown Beauties Nicole –
masseuse tits
Pastry Shop Remodel Firm
Our bakery remodel firm offers specialist renovation services to upgrade your store. We concentrate on appearances and performance to boost client complete satisfaction.
Seasonal flu is the strain of influenza virus that arrives in the UK each autumn.
you healthy Exceptional offers from online pharmacies help you when does tadalafil peak are available online.
Larger pituitary tumors macroadenomas, over 1 centimeter in diameter can place pressure on brain tissue and nerves, causing blindness, circling, seizures, or other neurological problems not directly related to hyperadrenocorticism.
Type 2 diabetes can also develop in people who are thin.
Keep saving money when you tadalafilдёж–‡ is.
However, in people with poor immune systems, such as organ transplant recipients or people with HIV, the virus can spread throughout the body and cause severe disease, even of the brain.
No matter if some one searches for his required thing, therefore he/she desires to be available that in detail, so that thing is maintained over here.
I blog quite often and I really thank you for your content. This article has truly peaked my interest. I will take a note of your blog and keep checking for new details about once a week. I opted in for your Feed as well.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is fundamental and all. However just imagine if you added some great photos or video clips to give your posts more, “pop”! Your content is excellent but with pics and videos, this site could definitely be one of the most beneficial in its field. Terrific blog!
“55optOrg”: массовая реализация имитационных композицийОптовая продажа декоративные композиции высшего качества по выгодным расценкамПриветствуем вас в “55optOrg” – первопроходце крупных партий имитационных растений! Мы предлагаем широкий спектр искусственных растений для крупных клиентов, охватывая цветочных дизайнеров, декораторов, event-агентства и торговые точки оптом искусственные цветы в Челябинске. Аргументы выбрать нашем магазине для оптовых закупок искусственных цветов: Реализуемые нами оптовые декоративные растения до того правдоподобны, что их сложно дифференцировать от настоящих . В процессе создания мы используем лишь отборные компоненты и передовые промышленные технологии . Наша компания обеспечивает оптовое приобретение цветочных композиций больше 1000 вариантов . От классических роз до экзотических орхидей – мы гарантируем полный ассортимент для претворения в жизнь ваших творческих замыслов .Выгодные цены на цветочные композиции большими партиями: Мы гарантируем привлекательные тарифы и индивидуальную схему бонусов . Рост объема заказа прямо пропорционально снижению стоимости ! Удобство оформления заказа и получения товара : Удобная система заказа через интернет или посредством телефонного звонка . Быстрая отправка по всей стране .Наш бизнес – оптовая дистрибуция имитационных флористических товаров”Компания 55optOrg” занимается крупнооптовых продажах декоративных растений на в течение свыше 10 лет. Наше достижение – предоставление клиентам опции покупки высококачественных декоративных растений в масштабных объемах. Масштабные отгрузки нашей искусственной флористики востребованы как в России, так и на международной арене (wholesale artificial flowers).Массовые продажи имитации цветов для всех запросовНа нашей площадке имеются в наличии:Букеты и композицииИскусственные цветочные элементы и декоративная зеленьЭлементы для оформления свадьбыДомашние зеленые друзья в кашпоДеревья и кустарникиCost-effective решения для purchasing неживых цветов in bulk”55optOrg” – искусственные растения крупными партиями по наиболее выгодным ценам. Мы обеспечиваем:Flexible system дисконтовSpecial предложения для постоянных клиентовПостоянные мероприятия и уценкиПокупая имитационные цветы в больших объемах в “55optOrg”, вы инвестируете в надежность и выгоду для своего бизнеса. Не упустите возможность ознакомиться больше о наших предложениях и разместить заявку уже сейчас!Искусственные растения крупными партиями: фундамент процветающего дела в области декора и флористикиНынешний дизайн и цветочное искусство не функционируют без декоративных растений. Большинство коммерсантов и организаций заинтересованы в закупке “искусственных флористических изделий в больших объемах”, чтобы обеспечить собственное бизнес высококачественными товарами по доступной расценке. Выражение “опт искусственные растения” часто применяется в поисковых запросах, когда заказчики выбирают проверенных поставщиков.Поиск оптовых продавцов искусственных цветовСледует обратить внимание, что запрос “искусственные цветы оптом” часто появляется в многочисленных вариантах, но с неизменным значением. Часто в поисковых фразах встречается фраза “купить большое количество искусственных цветов”, что говорит о желании клиента к приобретению. “Оптовая продажа искусственных цветов” – распространенное выражение в рекламных материалах поставщиков. Отдельные пользователи могут вводить запрос “опт цветов искусственных”, что можно считать еще одним формой часто встречающегося запроса.Мастерство флористики без пределов: оптовые поставки декоративных цветовДля тех, кто ищет наиболее профессиональный подход, “массовые продажи декоративных цветов” может выглядеть более заманчиво. “Искусственная цветоводство оптом” – это термин, который часто применяется в профессиональных кругах. “Массовые закупки правдоподобных флоры” может привлечь интерес тех, кто выбирает наиболее правдоподобные опции. Для международных запросов часто применяется английский эквивалент “wholesale artificial flowers”.Частые поисковые запросы крупных клиентов имитации цветовНекоторые покупатели предпочитают более конкретные запросы, такие как “большой опт премиальных имитации флоры”, что свидетельствует о поиск надежного поставщика с разнообразным ассортиментом. “Конкурентные тарифы на искусственные цветы оптом” привлекают тех, кто стремится найти наилучшее соотношение цены и качества. “Богатый ассортимент имитации цветов для масштабных покупателей” может заинтересовать тех, кто стремится предложить широкий выбор для своих клиентов.Передовые решения и забота об окружающей среде: актуальные направления в крупных поставках декоративной флоройБизнесы, занимающиеся оптовыми поставками нестандартных цветов, часто задействуют брендовые анкоры в своей маркетинге. Например, “Декоративные цветы оптом от 55опторг” помогает усилить связь между брендом и продукцией. “Купить оптом искусственные цветы на 55optOrg” – это призыв к покупке, который может улучшить продажи.Важно отметить, что сфера декоративных цветов постоянно эволюционирует. Возникают новые материалы и технологии, которые делают правдоподобность к натуральным по внешнему виду. Закупщики ищут не только стоимость, но и качество, долговечность и экологичность продукции. Многие поставщики теперь производят искусственные цветы, сделанные из переработанных материалов, что соответствует увеличивающийся потребность к экологичным изделиям.Вопреки разнообразие выражений, которыми оперируют заказчики и продавцы, очевидно одно: оптовая реализация декоративными цветами продолжает быть востребованной и пользоваться спросом. Многообразие ключевых слов демонстрирует широкий спектр нужд и предпочтений потребителей, от маленьких флористических салонов до масштабных компаний по декорированию. Продавцы, которые в состоянии удовлетворить широкие запросы потребителей и эффективно оперировать различными поисковыми запросами в своем маркетинге, имеют максимальные перспективы на развитие в этой конкурентной нише.
Excellent website. A lot of useful info here. I am sending it to some friends ans additionally sharing
in delicious. And certainly, thanks to your sweat!
Thanks for some other informative web site. The
place else may just I get that type of information written in such an ideal approach?
I’ve a project that I’m just now operating on, and I have been at the look out for such
info.
Pretty! This was an extremely wonderful post. Many thanks for providing these details.
Přijetí hypoteční platby může být nebezpečné pokud nemáte rádi čekání v dlouhých řadách , vyplnění vážný formuláře , a odmítnutí
úvěru na základě vašeho úvěrového skóre . Přijímání hypoteční platby může být problematické, pokud
nemáte rádi čekání v dlouhých řadách , podávání extrémních formulářů , a
odmítnutí úvěru na základě vašeho úvěrového skóre .
Přijímání hypoteční platby může být problematické ,
pokud nemáte rádi čekání v dlouhých řadách , vyplnění
extrémních formulářů a odmítnutí úvěrových rozhodnutí založených na úvěrových
skóre . Nyní můžete svou hypotéku zaplatit rychle a
efektivně v České republice. https://groups.google.com/g/sheasjkdcdjksaksda/c/rgeeAVo1mJw
Hey there this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding experience so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
Thhis paragraph is in fact a nice one iit hells new internet users,who
are wishning for blogging.
When treated appropriately, however, mold can be eliminated as can the debilitating symptoms.
Choose established online pharmacies when you decide to levitra vardenafil 20mg tablets are much better deals than in local stores.
High concentrations of fungal colonies, such as those growing in water-damaged flooring or building materials, can cause severe allergy symptoms, from flu-like discomfort to life-threatening asthma attacks.
These symptoms result from high levels of the hormones epinephrine and norepinephrine , which are secreted by the pheochromocytoma.
Save by searching for comparison sildenafil tadalafil vardenafil online. The easy way to buy
American Family Physician, 79, 985—994.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You definitely know what youre talking about, why throw away your intelligence on just posting videos to your site when you could be giving us something informative to read?
He or she will do a urine analysis in the office to look for signs of active infection.
Medical experts agree you should tadalafil 5 mg be taken before or after?
And that’s an emergency — it can even be life threatening.
KMSPico Download https://jaguarembalagens.com.br/activador
This can lead to a build up of pressure in the head, which causes nausea, vomiting, headache, and lethargy.
prices. It always has the lowestOrder remedies at tadalafil pills . See how it works!
People with type 2 diabetes make insulin, but their cells don’t use it as well as they should.
Hello! Would you mind if I share your blog with my zynga group? There’s a lot of people that I think would really appreciate your content. Please let me know. Thanks
жетоны в казино
Actually no matter if someone doesn’t understand then its up to other visitors
that they will help, so here it happens.
“55optOrg”: массовая реализация декоративных растенийОпт искусственные растения высшего уровня по доступным расценкамРады видеть вас в “55optOrg” – лидере массовых поставок искусственных цветов! Наш богатый ассортимент искусственных цветов подходит для крупных приобретений флористами, оформителями, event-агентствами и торговыми точками опт цветы искусственные в Хабаровске. Плюсы массовых приобретений декоративных растений у нашей компании :Непревзойденное уровень исполнения: Наши цветочные композиции оптом кажутся так натурально, что их сложно отличить от природных . В процессе создания мы используем исключительно высококачественные сырье и передовые производственные технологии .Богатый выбор: На нашем складе вы можете купить искусственные цветы оптом свыше 1000 видов . От классических роз до уникальных орхидей – мы обеспечиваем весь спектр для претворения в жизнь ваших творческих идей . Наша компания гарантирует привлекательные тарифы и адаптивную систему скидок . Повышение размера заказа непосредственно влияет на сокращению стоимости ! Простой процесс оформления и получения: Удобный способ заказа на сайте или по телефону . Скорая доставка в любой уголок России .Масштабная поставка имитационных цветов – наша сфера деятельности”55optOrg” проводит крупнооптовые отгрузки декоративных цветов уже свыше 10 лет. Мы рады снабжаем своих клиентов высококачественными имитационными растениями в масштабных количествах. Поставляемые нами оптовые партии декоративных флористических изделий популярны не только в России, но и за рубежом (wholesale artificial flowers).Wholesale букетов нестандартных на любые потребностиНаш выбор содержит:Цветочные композиции и аранжировкиДекоративные цветочные элементы и декоративная зеленьСвадебные украшенияДомашние зеленые питомцыКрупномеры и кустарниковые растенияВыгодная wholesale закупка копий растений”55optOrg” – ваш проверенный supplier artificial растений wholesale. Мы обеспечиваем:Индивидуальный метод к созданию бонусовBonuses и льготы для regular клиентовСезонные скидкиВыбирая “55optOrg” для крупнооптовых покупок имитационных цветов, вы обретаете проверенного партнера и высококачественную продукцию по конкурентным расценкам. Свяжитесь с нами без промедления, чтобы рассмотреть детали партнерства и сделать свой заявку!Имитационные цветы крупными партиями: фундамент успешного предприятия в области декора и цветочного бизнесаДекоративные флористические изделия стали в существенную составляющую актуального декора и флористики. Большое количество коммерсантов и компаний желают выявить дистрибьюторов “декоративных растений оптом” для получения превосходной продукции по привлекательным расценкам. Когда клиенты ищут проверенных продавцов, они нередко печатают в поисковый запрос “опт искусственные растения”.Где искать оптовых поставщиков декоративных растенийИнтересно отметить, что пользователи часто вводят запрос “искусственные цветы оптом”, меняя порядок слов, но сохраняя основу запроса. Зачастую клиенты включают в запрос слово действия, к примеру, “приобрести искусственные цветы оптом”, выражая желание совершить покупку. “Массовая реализация декоративных растений” – это словосочетание, которую чаще используют дистрибьюторы, предлагая свои предложения. “Оптовые партии декоративных цветов” – еще одна форма распространенного запроса пользователей.Сформируйте ботанический оазис: массовые продажи искусственной флористикиДля тех, кто подбирает более экспертный подход, “крупные приобретения искусственной зелени” может звучать более интересно. “Искусственная флористика в больших объемах” – это термин, который часто употребляется в профессиональных кругах. “Оптовая приобретение имитации флоры” может заинтересовать интерес тех, кто ищет наиболее реалистичные опции. Для глобальных обращений часто используется английский вариант “wholesale artificial flowers”.Часто встречающиеся формулировки запросов на оптовые закупки имитации флорыОпределенные покупатели предпочитают более подробные запросы, такие как “крупные партии высококачественных искусственных растений”, что указывает на желании найти надежного поставщика с богатым ассортиментом. “Выгодные тарифы на искусственные цветы оптом” привлекают тех, кто стремится найти оптимальное соотношение цены и качества. “Многообразный спектр декоративной флоры для оптовых клиентов” может привлечь внимание тех, кто хочет иметь широкий выбор для своих клиентов.Действенный продвижение в оптовой торговле декоративной флоройКомпании, занимающиеся на оптовой реализации декоративных цветов, часто применяют брендированные ссылки в своей рекламе. Например, “Искусственные цветы оптом от 55опторг” помогает закрепить в памяти потребителя связь между брендом и товаром. “Приобрести оптом искусственные цветы на 55optOrg” – это стимул к покупке, который может улучшить показатели продаж.Важно отметить, что рынок искусственных цветов постоянно прогрессирует. Возникают современные методы производства и материалы, которые делают правдоподобность к натуральным по внешнему виду. Оптовики обращают внимание не только выгодные цены, но и высокое качество, срок службы и экологическую безопасность изделий. Многие поставщики теперь производят декоративные цветы из вторичного сырья, что отвечает возрастающему потребности на экологически чистые продукцию.Несмотря на вариативность формулировок, которыми применяют заказчики и продавцы, очевидно одно: область оптовых продаж искусственных флоры продолжает быть оживленным и популярным. Вариативность запросов отражает разнообразные потребности и ожидания клиентов, от небольших флористических студий до больших оформительских фирм. Реализаторы, которые могут удовлетворить многообразие запросов и эффективно применять разнообразные ключевые слова в маркетинговой стратегии, имеют максимальные возможности на процветание в этой состязательной сфере бизнеса.
Thank you for sharing your info. I truly appreciate your efforts and I will be waiting for your next post thanks once again.
This website was… how do you say it? Relevant!! Finally I’ve found something that helped me. Kudos!
I have been surfing online more than 2 hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my view, if all website owners and bloggers made good content as you did, the web will be much more useful than ever before.
Incredible points. Sound arguments. Keep up the good spirit.
Simply wish to say your article is as amazing. The clarity in your post is simply great and i can assume you are an expert on this subject. Fine with your permission let me to grab your feed to keep up to date with forthcoming post. Thanks a million and please continue the enjoyable work.
These are actually enormous ideas in on the topic of blogging. You have touched some fastidious points here. Any way keep up wrinting.
obviously like your web-site but you need to take a look at the spelling on several of your posts. Several of them are rife with spelling problems and I find it very bothersome to inform the reality nevertheless I will surely come back again.
Спектр газов – промышленные газы Ульяновск
Производство Ar
Телефоны для связи: +7(9272)70-80-09
Факс: +7 (8422) 65-10-78.
2024
I like it when folks come together and share opinions. Great site, keep it up!
It’s actually a great and useful piece of info. I am glad that you just shared this helpful info with us. Please keep us informed like this. Thanks for sharing.
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an nervousness over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this hike.
Good article. I definitely appreciate this website. Continue the
good work!
Wonderful goods from you, man. I have understand your stuff previous to and you’re just too fantastic. I actually like what you have acquired here, really like what you’re saying and the way in which you say it. You make it enjoyable and you still take care of to keep it sensible. I can not wait to read much more from you. This is actually a great web site.
Amazing blog! Do you have any hints for aspiring writers?
I’m planning to start my own website soon but I’m a little lost
on everything. Would you suggest starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally overwhelmed ..
Any recommendations? Cheers!
I like it whenever people come together and share thoughts. Great blog, keep it up!
Линзы служат для фокусировки и коллимации лазерного луча оптической головки лазерного станка для резки, сварки и очистки. Всегда в наличии фокусирующая линза
I’m really enjoying the theme/design of your blog. Do you ever run into any browser compatibility issues? A few of my blog visitors have complained about my site not working correctly in Explorer but looks great in Safari. Do you have any solutions to help fix this issue?
I visit daily some websites and sites to read posts, but this web site provides quality based articles.
Hello there, just became aware of your blog through Google, and found that it is truly informative. I’m going to watch out for brussels. I will be grateful if you continue this in future. Numerous people will be benefited from your writing. Cheers!
This design is spectacular! You definitely know how to keep a reader amused. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job. I really loved what you had to say, and more than that, how you presented it. Too cool!
Every weekend i used to visit this web site, as i want enjoyment, for the reason that this this site conations truly nice funny material too.
This article is genuinely a pleasant one it helps new web users, who are wishing in favor of blogging.
I appreciate, cause I found just what I was taking a look for.
You’ve ended my four day long hunt! God Bless you man. Have a
nice day. Bye
Yes! Finally someone writes about %keyword1%.
Good information. Lucky me I came across your website by chance (stumbleupon). I have bookmarked it for later!
I feel this is one of the such a lot important info for me. And i’m satisfied studying your article. But should commentary on some normal things, The web site style is perfect, the articles is in point of fact great : D. Just right task, cheers
Hello every one, here every person is sharing these kinds of know-how, therefore it’s pleasant to read this weblog, and I used to go to see this web site everyday.
I ffeel thhis is among the moost important info foor me. And i aam glad studyging
your article. But want too remartk onn feww common things, The
website tasste iss wonderful, the artticles iss in pint of fact great : D.
Excellent process, cheers
This is a topic which is near to my heart… Many thanks! Exactly where are your contact details though?
Wow! Finally I got a blog from where I be able to really take helpful data regarding my study and knowledge.
Hello, yeah this post is truly good and I have learned lot of things from it on the topic of blogging. thanks.
Awesome thing here. I’m very gglad tto loo your
post. Thank you sso muchh and I aam takkng a look ahea
tto touch you. Wiill youu please drkp me a e-mail?
Hello to evey body, it’s my firsat ppay a quuck visit oof
this website; ths blog inludes amazing and actuwlly ine material in support oof visitors.
Fantastic beat ! I wish to apprentice while you amend your site, how can i subscribe for a weblog web site? The account aided me a acceptable deal. I have been tiny bit acquainted of this your broadcast offered bright clear concept
Remarkable! Its in fact remarkable article, I have got much clear idea on the topic of from this post.
Currently it appears like Movable Type is the preferred blogging platform available right now. (from what I’ve read) Is that what you are using on your blog?
Fastidious answers in return of this question with real arguments and explaining all on the topic of that.
Hello there, I discovered your website by way
of Google whilst searching for a similar subject, your site
came up, it seems good. I’ve bookmarked it in my google bookmarks.
Hi there, simply became aware of your weblog through Google, and located that it’s truly informative.
I’m going to be careful for brussels. I’ll appreciate should you continue this in future.
A lot of other people will probably be benefited from your writing.
Cheers!
I’m not sure why but this web site is loading incredibly slow
for me. Is anyone else having this problem or is it a issue on my end?
I’ll check back later and see if the problem still exists.
Hi there it’s me, I am also visiting this web page regularly, this web site is really fastidious
and the people are in fact sharing nice thoughts.
You really make it seem so easy with your presentation but I find this matter to be really something which I think I
would never understand. It seems too complicated and extremely broad for
me. I am looking forward for your next post, I’ll try to get
the hang of it!
Hey there! Someone in my Facebook group shared this site with us so I came to check it out. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Great blog and fantastic design.
Hi colleagues, how is everything, and what you wish for to say about this piece of writing, in my view its truly awesome for me.
Hello, just wanted to say, I enjoyed this blog post. It was inspiring. Keep on posting!
I’m impressed, I have to admit. Seldom do I encounter a blog that’s both equally educative and amusing, and let me tell you, you’ve hit the nail on the head. The problem is something which not enough people are speaking intelligently about. I am very happy that I found this in my hunt for something relating to this.
это mailsco
What’s up to all, it’s actually a fastidious for me to pay a visit this website, it contains important Information.
If you are going for best contents like I do, simply pay a visit this web site daily as it offers feature contents, thanks
I like the valuable information you supply to your articles. I will bookmark your blog and take a look at once more here regularly. I am fairly certain I’ll learn many new stuff right here! Good luck for the following!
Its like you read my mind! You appear to know so much about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a little bit, but instead of that, this is wonderful blog. A great read. I will certainly be back.
I just like the valuable info you provide in your articles. I will bookmark your weblog and test again here regularly. I’m rather sure I’ll learn a lot of new stuff proper right here! Good luck for the next!
Woah! I’m really digging the template/theme of this blog. It’s simple, yet effective. A lot of times it’s tough to get that “perfect balance” between user friendliness and appearance. I must say you’ve done a great job with this. In addition, the blog loads very fast for me on Internet explorer. Excellent Blog!
Hello! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work due to no back up. Do you have any methods to prevent hackers?
Wow that was unusual. I just wrote an really long comment but after I clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that over again. Anyways, just wanted to say great blog!
https://www.adswf.fr/juknis-dana-bos
Do you have a spam issue on this blog; I also am a blogger, and I was wanting to know your situation; many of us have developed some nice practices and we are looking to trade solutions with other folks, why not shoot me an e-mail if interested.
Are you looking for an best massage NY, parlour massage NY, thai massage NY, tantric massage NY, four hands massage or bodywork NY? Nuru Massage In Manhattan, NY were the first to offer excitatory and slippery massage and we are dedicated to it for now. If you want the most exotic massage service, look no further than the Nuru Massage In Manhattan, NY. Our nuru massage, japanese massage, body rub massage girls will pleasure you like no one before.
New-York Escort: body to body massage
Hello! This is my first visit to your blog! We are a team of volunteers and starting a new initiative in a community in the same niche. Your blog provided us valuable information to work on. You have done a outstanding job!
Hey! Do you use Twitter? I’d like to follow you if that would be okay. I’m definitely enjoying your blog and look forward to new posts.
Nice post. I was checking continuously this blog and I am inspired! Extremely useful info particularly the last phase 🙂 I take care of such info much. I used to be seeking this certain information for a very lengthy time. Thanks and best of luck.
Remarkable! Its really amazing article, I have got much clear idea regarding from this paragraph.
North Natt Only Fans Mega Link Folder
What’s up to all, how is everything, I think every one is getting more from this web site, and your views are fastidious in support of new users.
Hi, I do believe this is an excellent site. I stumbledupon it 😉 I may come back yet again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Lana Rhoads, Paige Vanazant, Steph Kegels ONLY FANS LEAKS ( https://t.me/CrocSpot )
Hi I am so thrilled I found your web site, I really found you by error, while I was researching on Digg for something else, Nonetheless I am here now and would just like to say cheers for a fantastic post and a all round enjoyable blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the fantastic job.
This excellent website truly has all the information and facts I needed about this subject and didn’t know who to ask.
Yasmine Lopez Only Fans Mega Link Folder
Rebecca J Only Fans Mega Link Folder
Please let me know if you’re looking for a writer for your site. You have some really good posts and I believe I would be a good asset. If you ever want to take some of the load off, I’d really like to write some articles for your blog in exchange for a link back to mine. Please send me an e-mail if interested. Cheers!
Wise people will purchase a how does levitra work being offered by many sites, make it easy to shop.
Your doctor may use blood and imaging tests to learn the stage of the disease.
Having read this I believed it was extremely enlightening. I appreciate you taking the time and energy to put this article together. I once again find myself spending a significant amount of time both reading and commenting. But so what, it was still worth it!
It’s an amazing article in favor of all the online users; they will obtain advantage from it I am sure.
Pretty! This has been a really wonderful post. Thanks for providing these details.
I’m really enjoying the theme/design of your web site. Do you ever run into any internet browser compatibility issues? A number of my blog readers have complained about my website not operating correctly in Explorer but looks great in Safari. Do you have any advice to help fix this problem?
Your style is really unique compared to other folks I’ve read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I’ll just bookmark this blog.
Sukari Sweets, Yur Aular, Nadia 999 Only Fans Leaks Mega Folder Link( https://UrbanCrocSpot.org/shop/ )
Verry energetic blog, I like that a lot. Willl there be a partt 2?
you’re truly a just right webmaster. The site loading velocity is amazing. It kind of feels that you are doing any distinctive trick. Moreover, The contents are masterwork. you’ve performed a magnificent task on this subject!
Mia Sorety Only Fans Mega Link Folder
I just couldn’t leave your web site before suggesting that I extremely enjoyed the standard info an individual supply in your visitors? Is going to be back ceaselessly in order to inspect new posts
Adele Exarchopoulos, Laetitia Casta, Marion Cotillard Only Fans Nudes Leaks ( https://CrocSpot.Fun )
scroll. Go to Code Form
Celina Smith Only Fans Mega Link Folder
Patricia Tarka Only Fans Mega Link Folder
I used to be recommended this website through my cousin. I’m no longer positive whether or not this put up is written by him as no one else recognise such precise about my problem. You’re wonderful! Thank you!
Gracie Bon Only Fans Mega Link Folder
I pay a visit day-to-day a few websites and blogs to read articles, however this webpage presents feature based writing.
Your style is so unique in comparison to other people I have read stuff from. Many thanks for posting when you’ve got the opportunity, Guess I will just bookmark this web site.
Celina Smith Only Fans Mega Link Folder
I think the admin of this site is really working hard in support of his web site, because here every information is quality based information.
Angie Acosta, Takara Lee, The Plug Daughter Only Fans Leaks( https://CrocSpot.Fun )
Hi there everybody, here every person is sharing these know-how, thus it’s nice to read this website, and I used to pay a quick visit this blog daily.
Hey very nice blog!
What’s up friends, how is everything, and what you desire to say on the topic of this article, in my view its in fact remarkable in support of me.
When someone writes an paragraph he/she keeps the thought of a user in his/her brain that how a user can be aware of it. Therefore that’s why this piece of writing is perfect. Thanks!
Gracie Bon Only Fans Mega Link Folder
Tik Tok Instagram Snapchat LEAKED NUDES VIDEOS( https://UrbanCrocSpot.org/shop/ )
Hey! I could have sworn I’ve been to thi website
before but aftr checking through some of thhe postt I realized it’s nnew too me.
Anyhow, I’m definnitely glad I foun itt and I’ll
bee book-marking and checkingg back often!
I have read so many content regarding the blogger lovers except this paragraph is in fact a fastidious post, keep it up.
Great information. Lucky me I discovered your site by chance (stumbleupon). I’ve saved as a favorite for later!
These are in fact enormous ideas in regarding blogging. You have touched some pleasant factors here. Any way keep up wrinting.
It’s a pity you don’t have a donate button! I’d without a doubt donate to this outstanding blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to new updates and will talk about this blog with my Facebook group. Talk soon!
Good day! I could have sworn I’ve been to this blog before
butt after looking at some of the articles I ealized it’s
new too me. Anyways, I’m definitely deligbhted I came across it and I’ll be bookmarking it and checking back often! https://Www.Waste-Ndc.pro/community/profile/tressa79906983/
I’m truly enjoying the design and layout of your site. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme? Great work!
Hi it’s me, I am also visiting this website daily, this web page is in fact fastidious and the people are really sharing nice thoughts.
I was extremely pleased to uncover this page. I need to to thank you for ones time for this particularly fantastic read!! I definitely enjoyed every little bit of it and I have you bookmarked to check out new things in your website.
It is not my first time to visit this site, i am browsing this web site dailly and obtain good facts from here every day.
I’d like to find out more? I’d like to find out some additional information.
Great info. Lucky me I came across your blog by chance (stumbleupon). I have saved as a favorite for later!
Medicine information. What side effects?
cost of imitrex pill
All information about medicines. Get now.
These are really fantastic ideas in regarding blogging. You have touched some nice points here. Any way keep up wrinting.
Hello colleagues, its fantastic piece of writing on the topic of teachingand completely explained, keep it up all the time.
Hi, i believe that i saw you visited my site thus i got here to go back the prefer?.I’m trying to to find issues to enhance my website!I assume its good enough to use some of your ideas!!
Right here is the perfect site for anybody who hopes to find out about this topic. You know a whole lot its almost tough to argue with you (not that I really would want to…HaHa). You certainly put a new spin on a topic that has been written about for decades. Great stuff, just wonderful!
Hello! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche. Your blog provided us beneficial information to work on. You have done a marvellous job!
Thanks for a marvelous posting! I actually enjoyed reading it, you could be a great author. I will make sure to bookmark your blog and will often come back from now on. I want to encourage one to continue your great work, have a nice day!
Howdy! Someone in my Facebook group shared this website with us so I came to check it out. I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my followers! Exceptional blog and great style and design.
Thank you a lot for sharing this with all of us you actually recognise what you’re speaking about! Bookmarked. Kindly additionally consult with my web site =). We could have a hyperlink change contract among us
Hurrah, that’s what I was seeking for, what a information! present here at this weblog, thanks admin of this site.
The spa center best calls visit one of the ways massage, is what we do. What is an exotic massage interested in everyone. Prostate massage it’s a craftsmanship of giving for pleasure. You be surprised to that,what variety enjoyment can get to know from choice massage. In school Soapy massage masseuses can do erotic massage with stones.
How is it done, and is there something exotic? We will tell you all about him that you wanted to know |Our aromatic massage is visited not only by men but also by women, and also by couples. You necessarily want to use only this infinitely … Our primary а task this is to please customer fantastic chic massage woman – woman. Private approach to any your wishes and conditions.
The sexy women our the spa center will give you an unforgettable experience. The spa salon is a place of rest and relaxation. This Sakura massage, as in principle, and relaxation, affects on some parts naked body, this helps man and woman become less tense. Choose one or just two beauties! Choose by appearance, both professional and professional proficiency!
Our salon in Empire City we can offer gorgeous Spa rooms with convenient interior. All of these rooms apply be you you are staying with us not attracting the attention of other customers.
We have a showroom in Midtown West. Girls Ariana :
nude massage studio
Interesting blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog stand out. Please let me know where you got your theme. With thanks
We’re a group of volunteers and opening a new scheme in our community. Your website offered us with valuable information to work on. You’ve done a formidable job and our entire community will be thankful to you.
Greetings! Very helpful advice in this particular article! It’s the little changes which will make the biggest changes. Thanks a lot for sharing!
I absolutely love your site.. Excellent colors & theme. Did you make this site yourself? Please reply back as I’m planning to create my very own blog and would love to find out where you got this from or exactly what the theme is called. Cheers!
kątownik 120×120
you’re truly a good webmaster. The site loading velocity is amazing. It kind of feels that you are doing any unique trick. Moreover, The contents are masterwork. you have done a fantastic activity on this topic!
I for all time emailed this web site post page to all my associates, for the reason that if like to read it after that my friends will too.
Excellent goods from you, man. I have understand your stuff previous to and
you are just too magnificent. I really like what you’ve acquired here, certainly like what
you’re stating and the way in which you say it.
You make it enjoyable and you still take care of to keep
it wise. I can’t wait to read much more from you. This is really a terrific site.
Generally I don’t read article on blogs, however I would like to say that this write-up very forced me to check out and do so! Your writing style has been surprised me. Thank you, very nice article.
Hi, I do think this is an excellent website. I stumbledupon it 😉 I will return yet again since I book marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
What i do not understood is in reality how you are now not really a lot more well-favored
than you might be right now. You are very intelligent.
You recognize thus considerably in the case of this matter, produced me in my opinion imagine it from
a lot of varied angles. Its like women and men are not fascinated until it’s one thing to
do with Lady gaga! Your personal stuffs outstanding.
Always handle it up!
I really like what you guys tend to be up too.
This type of clever work and coverage! Keep up the terrific works
guys I’ve included you guys to my personal blogroll.
Greate pieces. Keep writing such kind of info on your site. Im really impressed by your blog.
Hi there, You’ve done an excellent job. I will definitely digg it and individually suggest to my friends. I’m confident they’ll be benefited from this web site.
Attractive element of content. I just stumbled upon your blog and in accession capital to claim that I acquire in fact loved account your weblog posts. Any way I’ll be subscribing on your feeds or even I success you get right of entry to consistently fast.
Generally I do not learn article on blogs, however I wish to say that this write-up very pressured me to try and do it! Your writing style has been amazed me. Thank you, quite nice post.
Aw, this was an incredibly nice post. Finding the time and actual effort to make a superb article… but what can I say… I hesitate a whole lot and don’t manage to get anything done.
What’s up to every body, it’s my first pay a quick visit of this web site; this webpage includes remarkable and really fine data designed for readers.
ItMe.Xyz
[…]that will be the end of this write-up. Here you will find some web-sites that we believe you will appreciate, just click the links over[…]
Heya are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and set up my own. Do you need any html coding expertise to make your own blog? Any help would be greatly appreciated!
Right away I am going to do my breakfast, after having my breakfast coming yet again to read additional news.
Yes! Finally something about %keyword1%.
I will immediately seize your rss as I can not in finding your email subscription hyperlink or newsletter service. Do you’ve any? Kindly let me understand so that I may just subscribe. Thanks.
I visited many blogs however the audio feature for audio songs present at this web site is really wonderful.
Hi there! Do you know if they make any plugins to help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Many thanks!
Wow, marvelous blog layout! How long have you been blogging for? you made blogging look easy. The overall look of your website is excellent, let alone the content!
Hi, I do think this is a great website. I stumbledupon it 😉 I will come back yet again since I bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to guide other people.
My brother recommended I might like this blog. He used to be entirely right. This post actually made my day. You cann’t consider simply how a lot time I had spent for this info! Thanks!
Very quickly this web site will be famous among all blog viewers, due to it’s fastidious posts
Howdy, i read your blog from time to time and i own a similar one and i was just wondering if you get a lot of spam remarks? If so how do you prevent it, any plugin or anything you can advise? I get so much lately it’s driving me crazy so any support is very much appreciated.
I have been checking out many of your posts and i can claim pretty clever stuff. I will make sure to bookmark your site.
You can’t change anything.
What words … super
What can you say about this?
This is really fascinating, You are a very skilled blogger. I have joined your rss feed and sit up for looking for more of your magnificent post. Additionally, I have shared your web site in my social networks
Great article. I am facing a few of these issues as well..
Hi would you mind stating which blog platform you’re using? I’m going to start my own blog in the near future but I’m having a difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design and style seems different then most blogs and I’m looking for something unique. P.S Sorry for being off-topic but I had to ask!
Thanks , I’ve just been looking for info approximately this subject for a while and yours is the greatest I have came upon so far. But, what in regards to the conclusion? Are you sure in regards to the source?
GG With The WAP OnlyFans Mega Link Download
You made some decent points there. I looked on the internet for more information about the issue and found most people will go along with your views on this website.
Buy Leaked Only Fans ( Visit https://archiver.fans )
Ahaa, its nice conversation about this piece of writing here at this web site, I have read all that, so at this time me also commenting here.
Black Ass Jenny OnlyFans Mega Link Download
Hot 4 Lexi OnlyFans Mega Link Download ( Visit https://archiver.fans )
Ima Cri Baby OnlyFans Mega Link Download ( Visit https://archiver.fans )
Excellent pieces. Keep writing such kind of information on your page. Im really impressed by your site.
Hey there, You have done an incredible job. I’ll definitely digg it and for my part recommend to my friends. I’m sure they will be benefited from this site.
Congratulations, what words … wonderful thought
Genesis Mia Lopez OnlyFans Mega Link Download
Yasmine Lopez OnlyFans Mega Link Download ( Visit https://archiver.fans )
North Natt OnlyFans Mega Link Download
Black Ass Jenny OnlyFans Mega Link Download
10TB Only Fans Mega ( Visit https://archiver.fans )
continuously i used to read smaller posts which as well clear their motive, and that is also happening with this paragraph which I am reading now.
I’m not sure where you’re getting your information, but great topic. I needs to spend some time learning much more or understanding more. Thanks for excellent information I was looking for this info for my mission.
TheRealRebeccaJ OnlyFans Mega Link Download
Paragraph writing is also a fun, if you know afterward you can write if not it is difficult to write.
Genesis Mia Lopez OnlyFans Mega Link Download
Emmanuel Lustin OnlyFans Mega Link Download ( Visit https://archiver.fans )
Black Ass Jenny OnlyFans Mega Link Download
Fansly Leaks Mega Link
Jenise Hart OnlyFans Mega Link Download
Barely Legal Lexi OnlyFans Mega Link Download
Lexi 2 Legit OnlyFans Mega Link Download
Genesis Mia Lopez OnlyFans Mega Link Download
3TB Only Fans Mega
Bulma XO OnlyFans Mega Link Download
Jenise Hart OnlyFans Mega Link Download
3TB Only Fans Mega
Caaart OnlyFans Mega Link Download
North Natt OnlyFans Mega Link Download
Caaart OnlyFans Mega Link Download
I enjoy reading a post that can make people think. Also, thank you for allowing for me to comment!
Buy Only Fans Leaks ( Visit https://archiver.fans )
Its Lunar Liv OnlyFans Mega Link Download
Daalischus Rose OnlyFans Mega Link Download
Updated Only Fans Leaks ( Visit https://archiver.fans )
I just couldn’t go away your site before suggesting that I actually loved the standard information an individual supply to your visitors? Is gonna be back regularly in order to investigate cross-check new posts
Genesis Mia Lopez OnlyFans Mega Link Download
TheRealRebeccaJ OnlyFans Mega Link Download
What’s up colleagues, nice article and good urging commented here, I am in fact enjoying by these.
Buy Leaked Only Fans ( Visit https://archiver.fans )
Good day I am so excited I found your web site, I really found you by error, while I was searching on Bing for something else, Nonetheless I am here now and would just like to say thanks a lot for a remarkable post and a all round exciting blog (I also love the theme/design), I don’t have time to read it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the superb work.
Mega Link Shop ( Visit https://archiver.fans )
Mega Link Store
GG With The WAP OnlyFans Mega Link Download
Mega Link Store
Mega Link Shop ( Visit https://archiver.fans )
8TB Only Fans Mega ( Visit https://archiver.fans )
Rebecca J OnlyFans Mega Link Download ( Visit https://archiver.fans )
Wonderful beat ! I wish to apprentice while you amend your site, how can i subscribe for a blog site? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast offered bright clear idea
cost of cheap albuterol online
Buy Mega Links ( Visit https://archiver.fans )
What’s Going down i’m new to this, I stumbled upon this I’ve found It positively useful and it has aided me out loads. I’m hoping to give a contribution & assist other customers like its helped me. Good job.
TheRealRebeccaJ OnlyFans Mega Link Download
I am not certain where you’re getting your info, but great topic. I needs to spend some time studying more or figuring out more. Thank you for excellent info I used to be searching for this info for my mission.
It’s not my first time to go to see this website, i am browsing this site dailly and take fastidious information from here every day.
Updated Only Fans Leaks ( Visit https://archiver.fans )
WOW just what I was looking for. Came here by searching for %keyword%
Only Fans Leaks Free Download
8TB Only Fans Mega ( Visit https://archiver.fans )
With havin so much written content doo you ever run into any problems of plagorism or copyright
violation? My blog has a lot of completely unique content I’ve either written myself or outsourced but it looks like a lot of it is popping it up all over the web without my permission. Do you knnow any ways to help stop content from being stolen? I’d truhly appreciate it. https://study.ozonetherapy.ru/blog/index.php?entryid=55614
8TB Only Fans Mega ( Visit https://archiver.fans )
Hi there! I’m at work browsing your blog from my new iphone 3gs! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the great work!
fan balancing
Understanding Fan Balancing: Ensuring Optimal Performance
Welcome to our comprehensive overview of fan balancing, a crucial process for maintaining the operational efficiency and longevity of industrial fans. In this guide, we will explore the significance, methods, and tools related to fan balancing, specifically focusing on the fan balancing technique used to mitigate vibrations in rotors and other machinery.
What is Fan Balancing?
Fan balancing refers to the process of optimizing the distribution of mass in a rotating system, such as industrial fans, to achieve smooth operation. Imbalances can lead to vibrations, which not only affect performance but can severely damage machinery over time. Therefore, effective fan balancing is essential in minimizing wear and tear, ensuring efficient operations, and prolonging the life of the equipment.
The Importance of Fan Balancing
Every rotating unit, including fans, generates vibrations due to various factors such as uneven mass distribution, misalignment, or operational stresses. Excessive vibrations can cause premature failure of components, increase noise levels, and negatively impact the environment around the machinery. By implementing fan balancing, companies can significantly enhance the reliability of their equipment, reduce maintenance costs, and improve overall efficiency.
Types of Fan Imbalance
Imbalance in fans often derives from a range of issues, including:
Mechanical Imbalance: This occurs when the fan blades are not uniformly weighted or distributed. Common causes include manufacturing tolerances and wear over time.
Installation Issues: Improperly installed fans can lead to misalignment, which significantly affects operation.
Aerodynamic Imbalance: Vibration may arise from aerodynamic forces interacting with fan components, generating stress and noise.
Methods of Fan Balancing
There are two primary methods of fan balancing: dynamic and static balancing.
Static Balancing: This method focuses on balancing the fan when it is not rotating, ensuring there is an equal distribution of weight around the rotational axis.
Dynamic Balancing: In this method, vibrations are measured while the fan operates, and adjustments are made to reduce any excessive vibrations detected.
Tools for Fan Balancing
To implement efficient fan balancing, a variety of tools and machines are available:
Portable Balancers: Equipment such as the Balanset-1A allows for on-site balancing while measuring vibrations across multiple planes.
Vibration Analyzers: These devices help assess the vibrational state of fans, identifying where imbalances may occur.
Dedicated Balancing Machines: High sensitivity machines specifically designed to assess and adjust rotor imbalances accurately.
Best Practices for Fan Balancing
To ensure the most effective fan balancing, it’s essential to adopt best practices:
Regular Maintenance: Routine inspections and balancing keep machinery in prime condition and can prevent unexpected failures.
Adherence to Standards: Following international standards such as ISO 1940-1 ensures proper balancing quality and procedures.
Monitoring Vibrational Trends: Continuously monitoring vibrations can help identify issues before they become severe problems, allowing for proactive maintenance.
Conclusion
In conclusion, fan balancing is an imperative process that improves the functionality and reliability of fans in various industrial applications. By understanding its importance, methods, and associated tools, businesses can enhance their operational efficiency and reduce downtime. Regular maintenance and adherence to balancing best practices can lead to significant cost savings while ensuring a smooth running environment. Invest in good practices today, and prepare to enjoy the benefits of effective fan balancing in your operations.
Contact Us
If you’re interested in learning more about fan balancing services or would like to purchase top-of-the-line balancing equipment, please reach out to us through our contact page. We’re here to help you achieve optimal performance in your operations!
Ima Cri Baby OnlyFans Mega Link Download ( Visit https://archiver.fans )
Corinna Kopf OnlyFans Mega Link Download ( Visit https://archiver.fans )
hello!,I really like your writing so a lot! percentage we keep in touch extra approximately your article on AOL? I require an expert in this area to unravel my problem. May be that’s you! Taking a look ahead to see you.
Taylor Hall OnlyFans Mega Link Download
Great post. I used to be checking constantly this blog and I am impressed! Very helpful info specifically the last section 🙂 I care for such info a lot. I was looking for this certain information for a long time. Thanks and good luck.
Buy Leaked Only Fans ( Visit https://archiver.fans )
8TB Only Fans Mega ( Visit https://archiver.fans )
Good way of describing, and nice piece of writing to obtain data about my presentation subject matter, which i am going to convey in university.
Buy Mega Links ( Visit https://archiver.fans )
Mulan Hernandez OnlyFans Mega Link Download ( Visit https://archiver.fans )
Itz Grippy TV OnlyFans Mega Link Download ( Visit https://archiver.fans )
where buy generic finpecia without dr prescription
Mega Link Store
Free Only Fans Leaks ( Visit https://archiver.fans )
Itz Grippy TV OnlyFans Mega Link Download ( Visit https://archiver.fans )
Crii Baby RiRi OnlyFans Mega Link Download ( Visit https://archiver.fans )
Thanks very nice blog!
Now I am ready to do my breakfast, afterward having my breakfast coming again to read more news.
Buy Mega Links ( Visit https://archiver.fans )
Only Fans Leaks Mega Folders
먹튀 문제에 대해 이렇게 자세히 설명해주시니 감사해요! 방문하다 먹튀레이더
Nice
Jenise Hart OnlyFans Mega Link Download
Buy Fansly Leaks ( Visit https://archiver.fans )
10TB Only Fans Mega ( Visit https://archiver.fans )
Free Only Fans Leaks ( Visit https://archiver.fans )
Caaart OnlyFans Mega Link Download
Mulan Hernandez OnlyFans Mega Link Download ( Visit https://archiver.fans )
Buy Fansly Leaks ( Visit https://archiver.fans )
Free Only Fans Leaks ( Visit https://archiver.fans )
Only Fans Leaks Mega Folders
Only Fans Leaks Updates
GG With The WAP OnlyFans Mega Link Download
Mega Link Store
Buy Leaked Content ( Visit https://archiver.fans )
Emmanuel Lustin OnlyFans Mega Link Download ( Visit https://archiver.fans )
Caaart OnlyFans Mega Link Download
Genesis Mia Lopez OnlyFans Mega Link Download
Please let me know if you’re looking for a author for your blog. You have some really good posts and I feel I would be a good asset. If you ever want to take some of the load off, I’d really like to write some material for your blog in exchange for a link back to mine. Please send me an email if interested. Many thanks!
Buy Leaked Content ( Visit https://archiver.fans )
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You clearly know what youre talking about, why throw away your intelligence on just posting videos to your site when you could be giving us something enlightening to read?
Only Fans Leaks Free Download
Everything is very open with a precise explanation of the issues. It was definitely informative. Your site is extremely helpful. Many thanks for sharing!
3TB Only Fans Mega
Buy Mega Links ( Visit https://archiver.fans )
I’m amazed, I must say. Rarely do I come across a blog that’s both educative and interesting, and let me tell you, you’ve hit the nail on the head. The problem is something that too few people are speaking intelligently about. Now i’m very happy that I stumbled across this in my search for something regarding this.
Gina WAP OnlyFans Mega Link Download ( Visit https://archiver.fans )
At this time it looks like Expression Engine is the top blogging platform available right now. (from what I’ve read) Is that what you’re using on your blog?
Hey, I think your site might be having browser compatibility issues. When I look at your website in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, wonderful blog!
Hello There. I discovered your weblog the use of msn. That is a really smartly written article. I will be sure to bookmark it and return to read more of your helpful info. Thank you for the post. I’ll certainly return.
Only Fans Leaks Updates
Ima Cri Baby OnlyFans Mega Link Download ( Visit https://archiver.fans )
Genesis Mia Lopez OnlyFans Mega Link Download
North Natt OnlyFans Mega Link Download
8TB Only Fans Mega ( Visit https://archiver.fans )
Rubi Rose OnlyFans Mega Link Download
Barely Legal Lexi OnlyFans Mega Link Download
3TB Only Fans Mega
Buy Only Fans Leaks ( Visit https://archiver.fans )
Only Fans Leaks Mega Folders
North Natt OnlyFans Mega Link Download
Bulma XO OnlyFans Mega Link Download
билайн домашний интернет
https://bvbborussiadortmundfansclub.com/read-blog/5188_vybor-tarifnogo-plana-bilajn-domashnij-internet-chto-uchest.html
билайн интернет
провайдер мтс
http://www.ssokhongchiam.in.th/main/index.php?name=webboard&file=read&id=931774
мтс тарифы краснодар
Pretty nice post. I just stumbled upon your weblog and wanted to say that I have really enjoyed surfing around your blog posts. After all I will be subscribing to your rss feed and I hope you write again very soon!
мегафон тарифы на интернет
https://bayer04leverkusenfansclub.com/read-blog/9704_sravnenie-megafon-interneta-s-drugimi-provajderami.html
провайдер мегафон
Your method of explaining the whole thing in this paragraph is truly fastidious, every one be able to easily understand it, Thanks a lot.
Good day! I could have sworn I’ve been to this site before but after reading through some of the post I realized it’s new to me. Anyhow, I’m definitely happy I found it and I’ll be book-marking and checking back frequently!
Gina WAP OnlyFans Mega Link Download ( Visit https://archiver.fans )
Only Fans Leaks Updates
Only Fans Leaks Mega Folders
билайн подключение кемерово
https://manchesterunitedfansclub.com/read-blog/7443_vybor-pristavki-dlya-bilajn-tv-v-kemerovo.html
билайн подключение
Daalischus Rose OnlyFans Mega Link Download
Buy Leaked Only Fans ( Visit https://archiver.fans )
Barely Legal Lexi OnlyFans Mega Link Download
мтс подключение
https://chelseafansclub.com/read-blog/12351_mts-dengi-v-kemerovo.html
сайт мтс кемерово
3TB Only Fans Mega
Lexi 2 Legit OnlyFans Mega Link Download
мтс тарифы краснодар
https://santosfcfansclub.com/read-blog/6882_mts-tv-poisk-i-sortirovka-kontenta.html
мтс тарифы на интернет
Nice post. I was checking continuously this blog and I am impressed! Extremely useful information specifically the last part 🙂 I care for such info a lot. I was seeking this particular info for a very long time. Thank you and best of luck.
Buy Leaked Only Fans ( Visit https://archiver.fans )
Ima Cri Baby OnlyFans Mega Link Download ( Visit https://archiver.fans )
Asking questions are in fact fastidious thing if you are not understanding anything completely, but this piece of writing offers fastidious understanding even.
Buy Fansly Leaks ( Visit https://archiver.fans )
Mulan Hernandez OnlyFans Mega Link Download ( Visit https://archiver.fans )
ттк подключение барнаул
https://realmadridperipheral.com/read-blog/5925_ttk-stoimost-podklyucheniya-k-seti-5g.html
ттк домашний интернет
Excellent pieces. Keep posting such kind of information on your blog. Im really impressed by your blog.
Hi there, You’ve done an incredible job. I will certainly digg it and for my part recommend to my friends. I am sure they’ll be benefited from this web site.
Its Lunar Liv OnlyFans Mega Link Download
ттк тарифы ростов
https://jamesrodriguezclub.com/read-blog/5064_ttk-tv-rostov-blokirovka-kanalov-i-prichiny.html
ттк подключение
Best Online Casinos in South Africa 2024
TheRealRebeccaJ OnlyFans Mega Link Download
Taylor Hall OnlyFans Mega Link Download
TheRealRebeccaJ OnlyFans Mega Link Download
Mulan Hernandez OnlyFans Mega Link Download ( Visit https://archiver.fans )
Buy Only Fans Leaks ( Visit https://archiver.fans )
Ima Cri Baby OnlyFans Mega Link Download ( Visit https://archiver.fans )
Taylor Hall OnlyFans Mega Link Download
When I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I recieve
4 emails with the same comment. Perhaps there is a way you are able to remove me from that service?
Thanks a lot!
Mikaila Dancer OnlyFans Mega Link Download
Daalischus Rose OnlyFans Mega Link Download
10TB Only Fans Mega ( Visit https://archiver.fans )
Buy Leaked Content ( Visit https://archiver.fans )
It’s very effortless to find out any topic on net as compared to books, as I found this piece of writing at this web page.
If some one needs to be updated with most recent technologies afterward he must be pay a quick visit this web site and be up to date daily.
Hi, just wanted to tell you, I enjoyed this post. It was inspiring. Keep on posting!
Its not my first time to pay a visit this site, i am browsing this website dailly and take fastidious facts from here every day.
Bokeo really is a captivating treasure in Thailand! The combination of natural
beauty, rich culture, and calming landscapes provides an unforgettable travel experience.
From hidden waterfalls, to authentic encounters, each
moment in Bokeo is like discovering. It is
a must-see for anyone looking for genuine Thai appeal and undiscovered adventure!
We’re a group of volunteers and opening a new scheme in our community. Your web site provided us with valuable information to work on. You have done a formidable job and our entire community will be grateful to you.
Using cryptocurrency feels like being part of a movement.
https://t.me/cryptonetlake
What’s up to all, how is all, I think every one is getting more from this site, and your views are pleasant designed for new visitors.
Barely Legal Lexi OnlyFans Mega Link Download
Usually I don’t read post on blogs, but I would like to say that this write-up very compelled me to try and do it! Your writing taste has been amazed me. Thank you, quite nice article.
Barely Legal Lexi OnlyFans Mega Link Download
Hola Bulma OnlyFans Mega Link Download ( Visit https://archiver.fans )
Superb, what a webpage it is! This blog gives useful facts to us, keep it up.
I’m gone to tell my little brother, that he should also pay a visit this webpage on regular basis to obtain updated from newest information.
Only Fans Leaks Updates
Black Ass Jenny OnlyFans Mega Link Download
Lexi 2 Legit OnlyFans Mega Link Download
GinaWAP Only Fans PPVS Download https://urbancrocspot.org/tag/gg-with-the-wap/
GGWithTheWAP Only Fans PPVs ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
CocoFantasia OnlyFans Leaks Mega Folder Link Download ( https://UrbanCrocSpot.org )
Pretty nice post. I simply stumbled upon your blog and wished to say that I’ve truly enjoyed browsing your weblog posts. In any case I will be subscribing to your rss feed and I hope you write once more very soon!
Bombshell Mint OnlyFans Leaks ( https://urbancrocspot.org/the-real-bombshell-mint-only-fans-mega-link/ )
MatiVIP OnlyFans Leaks Mega Folder Link Download
The Real Bombshell Mint Only Fans Leaks ( https://UrbanCrocSpot.org/ )
buy levitra 20mg tablets
buy levitra 20mg tablets
advair mexico pharmacy
advair mexico pharmacy
tadalafil time to work
tadalafil time to work
viagra name
viagra name
TheThroatBully OnlyFans Leaks Mega Folder Link Download
Appreciate the recommendation. Will try it out.
KorinaKova OnlyFans Leaks Mega Folder Link Download
GinaWAP Only Fans Leaks ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
sildenafil how long does it take to work
sildenafil how long does it take to work
GGWithTheWAP Only Fans PPVs ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
The Real Bombshell Mint ( https://urbancrocspot.org/the-real-bombshell-mint-only-fans-mega-link/ )
Hey very nice blog!
GGWithTheWAP Mega Folder Download ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
Tytiania Sargent OnlyFans Leaks ( https://urbancrocspot.org/the-real-bombshell-mint-only-fans-mega-link/ )
what is sildenafil used for
what is sildenafil used for
MiaaDiorr OnlyFans Leaks Mega Folder Link Download ( https://UrbanCrocSpot.org )
ChrissyK OnlyFans Leaks Mega Folder Link Download ( https://UrbanCrocSpot.org )
The Real Bombshell Mint ( https://urbancrocspot.org/the-real-bombshell-mint-only-fans-mega-link/ )
GinaWAP Only Fans Leaks ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
The Real Touch XX OnlyFans Leaks Mega Folder Link Download ( https://CrocSpot.Fun )
GinaWAP Only Fans Leaks ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
Tytiania Sargent Naked Only Fans ( https://UrbanCrocSpot.org/shop )
Jasminca David OnlyFans Leaks Mega Folder Link Download
Tytiania Sargent Naked Only Fans ( https://UrbanCrocSpot.org/shop )
cialis price
cialis price
GGWithTheWAP Only Fans Leaks https://urbancrocspot.org/product-tag/gg-with-the-wap/
5mg tadalafil daily
5mg tadalafil daily
Bombshell Mint Nude Leaks ( https://CrocSpot.Fun )
get levitra online
get levitra online
BombshellMint ( https://UrbanCrocSpot.org/shop )
Jasminca David OnlyFans Leaks Mega Folder Link Download
what does sildenafil do
what does sildenafil do
WavyTing OnlyFans Leaks Mega Folder Link Download ( https://UrbanCrocSpot.org )
GinaWAP Only Fans PPVS Download https://urbancrocspot.org/tag/gg-with-the-wap/
GGWithTheWAP Mega Folder Download ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
what pharmacy has green xanax bars
what pharmacy has green xanax bars
viagra vs cialis which is better
viagra vs cialis which is better
It’s a pity you don’t have a donate button! I’d without a doubt donate to this fantastic blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to brand new updates and will share this site with my Facebook group. Chat soon!
мегафон домашний интернет
https://24ekb-domasnij-internet.ru
мегафон подключение екатеринбург
мегафон подключить
https://24ekb-domasnij-internet-2.ru
мегафон интернет
can tadalafil lower blood pressure
can tadalafil lower blood pressure
Why viewers still use to read news papers when in this technological world all is accessible on net?
мегафон интернет
https://24ekb-domasnij-internet-3.ru
мегафон домашний интернет екатеринбург
Spectrum of gases – cargo Ulyanovsk
Dioxide N2+CO2
Phones: +7(9272)70-80-09
Fax: +7 (8422) 65-10-78.
2025
билайн подключение краснодар
https://domashnij-internet-krasnodar.ru
билайн тв краснодар
билайн интернет краснодар
https://domashnij-internet-krasnodar-2.ru
сайт билайн краснодар
Normally I don’t learn post on blogs, however I wish to say that this write-up very compelled me to try and do so! Your writing style has been surprised me. Thank you, very great article.
провайдер билайн
https://domashnij-internet-krasnodar-3.ru
билайн подключение краснодар
мегафон домашний интернет
https://24ekb-domasnij-internet.ru
мегафон тв
Attractive section of content. I just stumbled upon your blog and in accession capktal to assert tha I acquire actually enjoyed account your blog posts.
Anyway I will be subscribing to your feeds and even I achievement you access consistently rapidly. https://www.romanarmytalk.com/rat/member.php?action=profile&uid=12392
If you wish for too obtain a good dral from this post then yoou have to apply these strategies
to your won website. https://www.selfhackathon.com/how-to-write-a-college-application-essay-a-complete-guide/
Hmm itt appears like your website ate my first commennt (it wwas super long) so I gess I’ll just sum it upp what I
wrotee and say, I’m thorouhly enjoying your blog. I ttoo aam an aspiring blog blogger but
I’m stipl new tto everything. Do you have any tips and hints for newbie blog writers?
I’d genuinely appreciate it. https://belajarjadimudah.com/blog/index.php?entryid=163
Just want to say your article is as astounding.
The clarity on your post is simply cool and i could assume you’re
knowledgeable on this subject. Fine togrther with yohr permission aallow me to grasp your feed to keep uup to date with
drawing close post. Thank you 1,000,000 and please continue the gratifying work. http://forum.altaycoins.com/viewtopic.php?id=1959995
It’s an amazing piece of writing in favor of all the online visitors; they will obtain benefit from it I am sure.
мегафон тв екатеринбург
https://24ekb-domasnij-internet-2.ru
мегафон интернет екатеринбург
Spectrum of gases – cargo Ulyanovsk
Oxigen O2
Phones: +7(9272)70-80-09
Fax: +7 (8422) 65-10-78.
2025
мегафон интернет екатеринбург
https://24ekb-domasnij-internet-3.ru
мегафон тарифы на интернет
Thanks for the concepts you have contributed here. Moreover, I believe usually there are some factors that keep your motor insurance premium decrease. One is, to take into account buying automobiles that are within the good list of car insurance firms. Cars which are expensive will be more at risk of being lost. Aside from that insurance policies are also depending on the value of the car, so the more pricey it is, then the higher the actual premium you spend.
I enjoy what you guys are usually up too. This type of clever work and reporting! Keep up the great works guys I’ve added you guys to my own blogroll.
билайн тв
https://domashnij-internet-krasnodar.ru
билайн цены
билайн краснодар
https://domashnij-internet-krasnodar-2.ru
билайн домашний интернет краснодар
Thank you for the good writeup. It actually was once a enjoyment account it. Look complicated to more added agreeable from you! By the way, how could we communicate?
Since manuscripts are subject to deterioration
билайн тв
https://domashnij-internet-krasnodar-3.ru
билайн тв
dosage of tegretol cr
dosage of tegretol cr
how often can i give my 3 year old ibuprofen
how often can i give my 3 year old ibuprofen
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to your blog? My website is in the very same area of interest as yours and my users would truly benefit from some of the information you present here. Please let me know if this ok with you. Thanks a lot!
gabapentin tabletten
gabapentin tabletten
мегафон домашний интернет екатеринбург
https://24ekb-domasnij-internet.ru
мегафон домашний интернет екатеринбург
sulfasalazine tablet formulation
sulfasalazine tablet formulation
мегафон тарифы екатеринбург
https://24ekb-domasnij-internet-2.ru
мегафон тарифы на интернет
celecoxib inflammation
celecoxib inflammation
мегафон телевидение
https://24ekb-domasnij-internet-3.ru
мегафон тв екатеринбург
Howdy are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and set up my own. Do you require any html coding knowledge to make your own blog? Any help would be greatly appreciated!
you are really a good webmaster. The site loading speed is incredible. It seems that you are doing any unique trick. In addition, The contents are masterwork. you’ve done a fantastic job on this topic!
провайдер билайн
https://domashnij-internet-krasnodar.ru
билайн подключить краснодар
билайн интернет
https://domashnij-internet-krasnodar-2.ru
билайн интернет краснодар
билайн домашний интернет
https://domashnij-internet-krasnodar-3.ru
билайн домашний интернет краснодар
Hello there! I could have sworn I’ve visited this web site before but after going through a few of the articles I realized it’s new to me. Nonetheless, I’m certainly happy I discovered it and I’ll be bookmarking it and checking back frequently!
GinaWAP Free Only Fans https://urbancrocspot.org/tag/gg-with-the-wap/
мегафон тв екатеринбург
https://24ekb-domasnij-internet.ru
провайдер мегафон
The Real Bombshell Mint Only Fans Leaks ( https://UrbanCrocSpot.org/ )
мегафон интернет
https://24ekb-domasnij-internet-2.ru
мегафон подключить
GinaWAP Only Fans PPVS Download https://urbancrocspot.org/tag/gg-with-the-wap/
мегафон тв
https://24ekb-domasnij-internet-3.ru
мегафон телевидение екатеринбург
RealPrincess97 OnlyFans Leaks Mega Folder Link Download ( https://CrocSpot.Fun )
Mandy Lee OnlyFans Leaks Mega Folder Link Download
Bombshell Mint Nude Leaks ( https://CrocSpot.Fun )
билайн телевидение краснодар
https://domashnij-internet-krasnodar.ru
билайн краснодар
билайн тарифы на интернет
https://domashnij-internet-krasnodar-2.ru
билайн тарифы на интернет
Howdy, i read your blog from time to time and i own a similar one and i was just wondering if you get a lot of spam responses? If so how do you stop it, any plugin or anything you can suggest? I get so much lately it’s driving me insane so any help is very much appreciated.
билайн цены
https://domashnij-internet-krasnodar-3.ru
билайн тв
Great, this is a very valuable phrase
GGWithTheWAP Mega Folder Download ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
Tytiania Sargent Naked Only Fans ( https://UrbanCrocSpot.org/shop )
Tytiania Sargent OnlyFans Leaks ( https://urbancrocspot.org/the-real-bombshell-mint-only-fans-mega-link/ )
GinaWAP Mega Folder Link https://urbancrocspot.org/product-tag/gg-with-the-wap/
The Real Touch XX OnlyFans Leaks Mega Folder Link Download ( https://CrocSpot.Fun )
CocoFantasia OnlyFans Leaks Mega Folder Link Download ( https://UrbanCrocSpot.org )
cilostazol prescribing information
cilostazol prescribing information
I think this is one of the most important information for me. And i am glad reading your article. But should remark on few general things, The website style is perfect, the articles is really great : D. Good job, cheers
diclofenac uses
diclofenac uses
mebeverine hydrochloride colese
mebeverine hydrochloride colese
You have made some good points there. I looked on the net to find out more about the issue and found most people will go along with your views on this website.
how to get pyridostigmine without dr prescription
how to get pyridostigmine without dr prescription
mestinon buy online
mestinon buy online
Hi, Neat post. There’s an issue along with your web site in internet explorer, might check this? IE nonetheless is the market chief and a large section of other people will pass over your wonderful writing due to this problem.
imitrex and neck pain
imitrex and neck pain
Hello, of course this post is actually fastidious and I have learned lot of things from it about blogging. thanks.
EnvyKellsx3 OnlyFans Leaks Mega Folder Link Download
GGWithDaWAP Only Fans Leaks https://urbancrocspot.org/tag/gg-with-the-wap/
amitriptyline generic name
amitriptyline generic name
GGWithTheWAP Only Fans PPVs ( https://urbancrocspot.org/gina-wap-gg-with-the-wap-only-fans-mega-link-9gb/ )
Tytiania Sargent Nude Leaks ( https://UrbanCrocSpot.org/ )
Alexis Texas OnlyFans Leaks Mega Folder Link Download ( https://CrocSpot.Fun )
Tytiania Sargent Naked Only Fans ( https://UrbanCrocSpot.org/shop )
Having read this I thought it was rather informative. I appreciate you taking the time and effort to put this short article together. I once again find myself personally spending way too much time both reading and commenting. But so what, it was still worthwhile!
Hey! I could have sworn I’ve been to this site before but after checking through some of the post I realized it’s new to me. Nonetheless, I’m definitely happy I found it and I’ll be book-marking and checking back often!
A motivating discussion is worth comment. I do believe that you should publish more on this issue, it may not be a taboo subject but usually folks don’t discuss these topics. To the next! Cheers!!
Normally I do not read post on blogs, but I would like to say that this write-up very forced me to try and do it! Your writing style has been surprised me. Thanks, quite nice article.
Hi! This is kind of off topic but I need some guidance from an established blog. Is it hard to set up your own blog? I’m not very techincal but I can figure things out pretty quick. I’m thinking about making my own but I’m not sure where to begin. Do you have any tips or suggestions? Many thanks
Hey I am so glad I found your blog page, I really found you by accident, while I was looking on Aol for something else, Nonetheless I am here now and would just like to say many thanks for a incredible post and a all round enjoyable blog (I also love the theme/design), I don’t have time to go through it all at the minute but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read much more, Please do keep up the excellent work.
You have made some really good points there. I checked on the web for more info about the issue and found most people will go along with your views on this site.
Just wish to say your article is as astonishing. The clearness in your post is just excellent and i can assume you’re an expert on this subject. Well with your permission let me to grab your feed to keep updated with forthcoming post. Thanks a million and please continue the rewarding work.
It’s amazing how crypto can empower people financially in developing countries.
https://t.me/cryptonetlake
maxalt and wellbutrin
maxalt and wellbutrin
Valuable information. Fortunate me I discovered your site by chance, and I’m shocked why this accident did not happened earlier! I bookmarked it.
lioresal buvable
lioresal buvable
drug class of mobic
drug class of mobic
baclofen for rigidity
baclofen for rigidity
feldene sublingual piroxicam
feldene sublingual piroxicam
rizatriptan benz odt
rizatriptan benz odt
imdur medication information
imdur medication information
One important thing is that when you find yourself searching for a student loan you may find that you will need a co-signer. There are many situations where this is true because you might discover that you do not use a past credit rating so the mortgage lender will require that you have someone cosign the borrowed funds for you. Good post.
I take pleasure in, cause I discovered exactly what I was taking a look for. You’ve ended my 4 day long hunt! God Bless you man. Have a nice day. Bye
imuran enzyme test
imuran enzyme test
without prescription aceon perindoprilum store
buy aceon safely internet
aceon buy gloucester
buy cyprostol cytotec 200mg
buy aceon online and aceon
cytotec uk buy online
buy cytotec without rx needed
where can i buy ketorolac pill
where can i buy ketorolac pill
how to wean off tizanidine
how to wean off tizanidine
aceon hypertension cheap
no prescription armix aceon online
pharmacy cytotec purchase jcb otc
cyproheptadine canine side effects
cyproheptadine canine side effects
how to get cheap toradol prices
how to get cheap toradol prices
periactin uses side effects
periactin uses side effects
cytotec plus order form
order cytotec discount pill wokingham
artane beaumont community centre
artane beaumont community centre
zanaflex flexeril interactions
zanaflex flexeril interactions
best price aceon south carolina
One thing is that if you are searching for a student loan you may find that you’ll want a cosigner. There are many situations where this is correct because you will find that you do not use a past credit ranking so the bank will require that you have someone cosign the loan for you. Interesting post.
aceon online saturday delivery
cost for aceon in columbia
What’s up to every one, it’s actually a good for me to pay a quick visit this website, it consists of important Information.
purchase cytotec wokingham
no prescription armix aceon online
purchase cytotec vermont
price cytotec fast delivery louisville
buy upjohn cytotec 2mg.bars
purchase aceon mexico
cheap aceon online drug
Great blog here! Also your site loads up fast! What host are you using? Can I get your affiliate link to your host? I wish my site loaded up as quickly as yours lol
Перейти до вмісту
tradinginfo
Аналітика
Навчання
Криптовалюта
Трейдинг
Компанія
Консультація
Пошук…
Навчання трейдингу
Навчання трейдингу, курси трейдингу в Львів, Київ, Одеса, Чернівці, Харків, Ужгород, Вінниця, Тернопіль, Запоріжжя, Івано-Франківськ, Полтава, Чернігів, Черкаси, Суми, Луцьк, Миколаїв, Дніпро, Кропивницький, Рівне, Хмельницький, Житомир, Херсон та онлайн. Індивідуальні заняття з практикуючими трейдерами. Криптовалюта, Валютні ринки, Фондові ринки.
Навчання криптовалюта
Криптовалюта з чого почати
Рівень: початковий
Кількість уроків: 10-30
Детальніше
Навчання по криптовалюті
Рівень: початковий
Кількість уроків: 10
Детальніше
Трейдинг криптовалют
Рівень: початковий, середній
Кількість уроків: 10
Детальніше
Блокчейн навчання
Рівень: початковий, середній
Кількість уроків: 10
Детальніше
Курс “10 кращих крипто стратегій”
Рівень: середній
Кількість уроків: 10
Детальніше
Навчання трейдингу
Безпечний трейдинг
Рівень: початковий
Кількість уроків: 5
Детальніше
Трейдинг для початківців
Рівень: початковий
Кількість уроків: 10
Детальніше
Курси трейдингу онлайн
Рівень: початковий
Кількість уроків: 10
Детальніше
10 кращих стратегій трейдингу
Рівень: середній
Кількість уроків: 10
Детальніше
Smart Money Курс
Рівень: початковий
Кількість уроків: 10
Детальніше
Навчання трейдингу в офісах
Навчання трейдингу Київ
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Харків
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Львів
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Рівне
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Дніпро
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Одеса
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Івано-Франківськ
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Луцьк
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Тернопіль
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Чернівці
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Хмельницький
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Ужгород
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Вінниця
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Полтава
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Житомир
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Запоріжжя
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Херсон
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Суми
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Черкаси
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Навчання трейдингу Чернігів
Рівень: початковий, середній, профі
К-сть уроків: 5-30
Детальніше
Чому трейдери обирають TradingInfo
Навчання Форекс та криптовалюта. З нами кожен знайде курс для себе:
навчання трейдингу криптовалют
здобуття навичок короткотермінової і середньотермінової торгівлі
алготрейдинг
психологія торгівлі
торгові стратегії для крипто та форекс ринку
навчання торгівлі на Форексі
біткоін курси
форекс торгові стратегії
Навчання трейдингу
Команда професійних трейдерів розробляє курси виходячи зі свого досвіду, зміни ринку і сучасних методик, які допомагають в найкоротші терміни освоїти матеріал і вийти на новий рівень прибутку.
Тебе чекає оптимальний мікс теорії і практики, відсутність “водички” і всебічна підтримка наставника.
Ви можете пройти навчання трейдингу Львів, Київ, Одеса, Чернівці, Харків, Ужгород, Вінниця, Тернопіль, Запоріжжя, Івано-Франківськ, Полтава, Чернігів, Черкаси, Суми, Луцьк, Миколаїв, Дніпро, Кропивницький, Рівне, Хмельницький, Житомир, Херсон та онлайн.
Як відомо, навчання Форекс з наставником проходить швидше, дає кращі результати та обходиться дешевше. Так як помилки новачків можуть коштувати їм не одного депозиту, тоді як робота з досвідченим трейдером допоможе скоротити втрати в рази.
Вибирайте відповідний курс і вчіться за авторською методикою.
tradinginfo
Все про фінансові ринки. Криптовалюта, Біткоін, Форекс, Акції. Торгові стратегії. Торгові сигнали. Навчання трейдингу.
Контакти
Львів, проспект В’ячеслава Чорновола, 77 (ЖК Платинум)
+380934125348
info@tradinginfo.club
Facebook
Instagram
Telegram
Аналітика
Аналітика валют
Аналітика криптовалют
Аналітика фінансових ринків
Аналітика фондового ринку
Індекс страху і жадібності криптовалют
Таблиця прогнозу спільноти форекс
Теплова карта криптовалют
Форекс економічний календар
Прогноз EUR/USD
Прогноз GBP/USD
Прогноз USD/UAH
Навчання
Навчання
Курс Smart Money
Безпечний трейдинг
Блокчейн навчання
Криптовалюта з чого почати
Курси трейдингу онлайн
Навчання по криптовалюті
Навчання трейдингу Київ
Навчання трейдингу Львів
Навчання трейдингу Одеса
Трейдинг для початківців
Трейдинг криптовалют навчання
Трейдинг
Price Action
Книги про трейдинг
Основи трейдингу
Словник трейдера
Технічний аналіз
Технічні індикатори
Торгові стратегії
Трейдинг
Успішні трейдери
Фондовий ринок
Фундаментальний аналіз
Криптовалюта
Біткоін
Блокчейн
Криптовалюта
Криптовалюти
Криптовалютні гаманці
Основи криптовалюти
Словник криптотермінів
Теплова карта криптовалют
Торгівля криптовалютою
Курс Bitcoin (BTC)
Курс Ethereum (ETH)
Курс Solana (SOL)
Курс Dogecoin (DOGE)
Курс Ripple (XRP)
© 2024 TradingInfo. Всі права захищено.
Політика конфіденційності
Відмова від відповідальності
Відмова від відповідальності
Компанія не надає гарантій заробітку на біржах в якій би то не було формі. Компанія не займається діяльністю, яка підлягає ліцензуванню. Компанія не займається брокерським обслуговуванням. Компанія не займається довірчим управлінням. Компанія не залучає позики у населення.
Open chaty
no script misoprostol cytotec generic
как отыграть бонус в 1xbet tranzechpay 30
When I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I recieve four emails with the same comment. There has to be a way you can remove me from that service? Appreciate it!
Hello there I am so grateful I found your blog, I really found you by error, while I was searching on Askjeeve for something else, Anyways I am here now and would just like to say thank you for a tremendous post and a all round interesting blog (I also love the theme/design), I don’t have time to browse it all at the minute but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the superb jo.
I’m impressed by the speed of growth in the cryptocurrency industry
https://t.me/s/cryptonetlake
Fantastic website. A lot of useful information here. I’m sending it to some buddies ans additionally sharing in delicious. And certainly, thanks on your effort!
сколько стоит составление искового заявления в суд у юриста в москве
I have really noticed that credit repair activity ought to be conducted with tactics. If not, you might find yourself damaging your ranking. In order to grow into success fixing your credit rating you have to ascertain that from this moment you pay your monthly expenses promptly before their planned date. It really is significant given that by not really accomplishing this, all other activities that you will decide to use to improve your credit standing will not be effective. Thanks for sharing your strategies.
Thanks for helping me to acquire new suggestions about computer systems. I also have the belief that one of the best ways to maintain your laptop computer in primary condition has been a hard plastic-type material case, and also shell, that fits over the top of one’s computer. Most of these protective gear tend to be model distinct since they are made to fit perfectly above the natural casing. You can buy all of them directly from owner, or from third party places if they are readily available for your laptop computer, however only a few laptop could have a covering on the market. All over again, thanks for your recommendations.
This article is a breath of fresh air! The author’s distinctive perspective and insightful analysis have made this a truly fascinating read. I’m grateful for the effort she has put into crafting such an educational and mind-stimulating piece. Thank you, author, for offering your expertise and sparking meaningful discussions through your brilliant writing!
cytotec plus order form
buy online order buy cytotec
aceon online discount
Heya i?m for the primary time here. I came across this board and I in finding It truly helpful & it helped me out much. I am hoping to offer one thing again and aid others such as you aided me.
One thing I would really like to say is the fact that before acquiring more pc memory, have a look at the machine in which it could well be installed. In the event the machine is actually running Windows XP, for instance, the particular memory ceiling is 3.25GB. Installing greater than this would purely constitute a waste. Be sure that one’s motherboard can handle the actual upgrade quantity, as well. Great blog post.
билайн телевидение
https://chelseafansclub.com/read-blog/14192_bilajn-ceny-na-mobilnyj-internet-v-raznyh-paketah.html
билайн подключить кемерово
whoah this blog is great i love reading your posts. Keep up the good work! You understand, lots of people are looking round for this information, you could help them greatly.
мтс подключение
https://www.netrecruit.al/employer/therese/
мтс подключение
мтс телевидение краснодар
https://cambodiaexpertalliance.net/employer/earle/
мтс домашний интернет
сайт мегафон ростов
https://enchile.cl/employer/corina/
мегафон тарифы на интернет
An impressive share! I have just forwarded this onto a colleague who has been doing a little homework on this. And he actually bought me dinner due to the fact that I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending time to discuss this matter here on your site.
Mit den free coins slotpark kannst du dein Spiel sofort verbessern! Kein Aufwand, keine Registrierung – einfach klicken und die besten Vegas-Slots spielen.
мегафон телевидение
https://thathwamasijobs.com/companies/everette/
сайт мегафон ростов
ттк тарифы на интернет
https://job4thai.com/profile/isobelmcaulay7
ттк интернет барнаул
Hello there, You have done a great job. I’ll certainly digg it and personally suggest to my friends. I’m confident they will be benefited from this web site.
ттк домашний интернет ростов
https://myjobapply.com/employer/cathern/
ттк тв ростов
Hi Dear, are you genuinely visiting this site daily, if so then you will without doubt take good knowledge.
билайн телевидение кемерово
https://dayjobs.in/employer/cortez/
билайн подключить кемерово
провайдер мтс
https://newtheories.info/community/profile/valenciallewely/
мтс интернет
мтс домашний интернет
http://jobjungle.co.za/profile/brittnygrave93
мтс тарифы краснодар
мегафон подключение ростов
https://rabotadnr.ru/companies/gretchen/
мегафон подключить
ттк подключить барнаул
https://tayseerconsultants.com/employer/rae/
ттк тв
ттк тарифы ростов
https://dreamcorpsllc.com/employer/clement/
ттк подключение ростов
This is really interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your wonderful post. Also, I have shared your site in my social networks!
билайн цены
https://collegejobportal.in/employer/miles/
билайн тв кемерово
Wow that was odd. I just wrote an really long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say great blog!
мтс кемерово
https://jobseeker.charisonecare.co.uk/employer/sam/
мтс телевидение кемерово
мтс подключить
https://job-maniak.com/employer/vida/
провайдер мтс
сайт мегафон ростов
https://heifernepal.org/employer/veola/
мегафон тарифы на интернет
ттк цены
https://trustemployement.com/employer/clinton/
ттк подключить
Hi there, after reading this remarkable piece of writing
i am too happy to share my knowledge here with colleagues.
I got this web page from my pal who informed me regarding this site and now this time I am visiting this web page
and reading very informative articles or reviews at this time.
провайдер ттк
https://www.jobplanner.eu/employer/leigh/
ттк домашний интернет
Δωρεάν μάρκες καθημερινά για σένα – τακτικά! Χωρίς κόπο, χωρίς εγγραφή, ξεκίνα το παιχνίδι αμέσως! }
https://github.com/GreekGames/IviBet-Greece
билайн кемерово
https://www.punajuaj.com/companies/stevie/
билайн домашний интернет
I am curious to find out what blog platform you have been utilizing? I’m experiencing some small security problems with my latest blog and I would like to find something more risk-free. Do you have any solutions?
You have a real talent for this field. Top adult movies
провайдер мтс
https://realestate.kctech.com.np/profile/samarapearsall
мтс телевидение краснодар
мегафон ростов
http://lesstagiaires.com/employer/raina/
мегафон домашний интернет
ттк телевидение барнаул
https://itheadhunter.vn/jobs/companies/arletha/
ттк телевидение барнаул
сайт ттк ростов
https://portalwe.net/employer/sebastian/
ттк подключить
Предлагаем услуги профессиональных инженеров офицальной мастерской.
Еслли вы искали ремонт фотоаппаратов canon в москве, можете посмотреть на сайте: ремонт фотоаппаратов canon
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Accelerate your medical career with MBBS Direct Admission in Orissa.
Entdecke die Welt der Slotpark-Boni mit dem slotpark bonus, der dir hilft, jedes Spiel zu dominieren. Tägliche Boni sind der Schlüssel, um das Spiel lange und mit viel Freude zu spielen. Du wirst überrascht sein, wie schnell du die besten Spielautomaten knacken kannst, wenn du den richtigen Bonus verwendest.
мегафон тв екатеринбург
https://ekb-domasnij-internet-3.ru
мегафон тв
мегафон подключить екатеринбург
https://ekb-domasnij-internet.ru
мегафон подключить екатеринбург
Thanks for the suggestions you have shared here. Something important I would like to talk about is that pc memory needs generally increase along with other breakthroughs in the technological know-how. For instance, any time new generations of processor chips are made in the market, there is certainly usually an equivalent increase in the type preferences of both the laptop or computer memory and hard drive space. This is because the application operated by way of these processor chips will inevitably surge in power to leverage the new engineering.
билайн подключить
https://infodomashnij-internet-krasnodar-2.ru
билайн подключить
билайн телевидение
https://infodomashnij-internet-krasnodar-3.ru
билайн подключить
I have realized that online degree is getting favorite because getting your college degree online has become a popular alternative for many people. Many people have definitely not had a chance to attend a traditional college or university nevertheless seek the improved earning potential and career advancement that a Bachelor Degree grants. Still some others might have a college degree in one discipline but want to pursue a thing they now possess an interest in.
билайн интернет краснодар
https://infodomashnij-internet-krasnodar.ru
билайн подключить
мегафон интернет екатеринбург
https://ekb-domasnij-internet-2.ru
мегафон телевидение екатеринбург
Discover how MBBS Admission Through Management/Nri Quota in Jharkhand can make your career path smoother.
мегафон домашний интернет екатеринбург
https://ekb-domasnij-internet-3.ru
мегафон екатеринбург
мегафон подключение екатеринбург
https://ekb-domasnij-internet.ru
мегафон домашний интернет
билайн тв краснодар
https://infodomashnij-internet-krasnodar-2.ru
билайн подключить
билайн краснодар
https://infodomashnij-internet-krasnodar-3.ru
билайн интернет краснодар
билайн подключение
https://infodomashnij-internet-krasnodar.ru
билайн интернет краснодар
мегафон подключение екатеринбург
https://ekb-domasnij-internet-2.ru
мегафон домашний интернет
Хотите узнать, какие криптобиржи будут самыми надежными в 2025 году? Мы подготовили для вас подробный обзор топ-10 платформ, которые заслуживают вашего внимания! Узнайте, где лучше торговать, хранить и приумножать свои активы. Читайте статью и выбирайте биржу, которая подходит именно вам!
Криптобиржи с поддержкой фиата 2025
мегафон подключить
https://ekb-domasnij-internet.ru
провайдер мегафон
билайн подключение краснодар
https://infodomashnij-internet-krasnodar-2.ru
билайн тв
I do not even know how I ended up here, but I thought this post was good. I don’t know who you are but certainly you’re going to a famous blogger if you aren’t already 😉 Cheers!
билайн тарифы на интернет
https://infodomashnij-internet-krasnodar-3.ru
билайн тарифы краснодар
билайн подключение
https://infodomashnij-internet-krasnodar.ru
билайн интернет
провайдер мегафон
https://ekb-domasnij-internet-2.ru
мегафон подключить
мегафон подключить екатеринбург
https://ekb-domasnij-internet-3.ru
мегафон телевидение екатеринбург
провайдер мегафон
https://ekb-domasnij-internet.ru
мегафон телевидение екатеринбург
Φίλοι των κουλοχέρηδων, προσοχή! Πάρε τις καθημερινές δωρεάν μάρκες σου και κέρδισε – χωρίς ερωτηματολόγια! }
https://github.com/GreekGames/Mighty-Hot-Wilds-Demo
You are so awesome! I do not think I’ve truly read through something like that before. So wonderful to find someone with original thoughts on this subject. Really.. many thanks for starting this up. This site is one thing that is needed on the internet, someone with a bit of originality!
I really like your blog.. very nice colors & theme. Did you create this website yourself or did you hire someone to do it for you? Plz respond as I’m looking to construct my own blog and would like to find out where u got this from. appreciate it
билайн домашний интернет
https://infodomashnij-internet-krasnodar-2.ru
билайн подключить краснодар
билайн подключение краснодар
https://infodomashnij-internet-krasnodar-3.ru
билайн подключение
I am not sure where you are getting your information, but great topic. I needs to spend some time learning more or understanding more. Thanks for fantastic info I was looking for this info for my mission.
билайн цены
https://infodomashnij-internet-krasnodar.ru
билайн тв краснодар
You can certainly see your skills in the work you write. The world hopes for more passionate writers like you who aren’t afraid to say how they believe. Always follow your heart.
It’s going to be end of mine day, but before finish I am reading this wonderful piece of writing to increase my know-how.
Thanks for your helpful article. One other problem is that mesothelioma cancer is generally brought on by the breathing of material from asbestos fiber, which is a cancer causing material. It is commonly observed among laborers in the engineering industry who definitely have long contact with asbestos. It could be caused by moving into asbestos insulated buildings for a long time of time, Family genes plays an important role, and some folks are more vulnerable towards the risk than others.
сайт мтс новосибирск
https://eng.worthword.com/bbs/board.php?bo_table=free&wr_id=1871147
мтс подключить новосибирск
Your home is valueble for me. Thanks!?
мтс цены
https://timviec24h.com.vn/companies/jobsinsidcul3282/
мтс новосибирск
Предлагаем услуги профессиональных инженеров офицальной мастерской.
Еслли вы искали ремонт фотоаппаратов canon в москве, можете посмотреть на сайте: ремонт фотоаппаратов canon в москве
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Thanks a bunch for sharing this with all of us you really know what you are talking about! Bookmarked. Please also visit my web site =). We could have a link exchange arrangement between us!
мтс интернет
https://www.opad.biz/employer/2t-s6213/
мтс подключить новосибирск
мтс подключить новосибирск
https://jobs.constructionproject360.com/employer/ondispatch5037/
мтс тарифы новосибирск
Youre so cool! I dont suppose Ive read something like this before. So nice to seek out anyone with some original thoughts on this subject. realy thanks for starting this up. this website is something that is wanted on the internet, someone with just a little originality. helpful job for bringing one thing new to the internet!
мтс подключить
https://dreamcorpsllc.com/employer/bcstaffing6906/
мтс тв
мтс подключение
https://www.chuhaipin.cn/employer/cbfacilitiesmanagement4520/
мтс цены
Very nice post. I just stumbled upon your blog and wished to say that I have truly enjoyed browsing your blog posts. In any case I?ll be subscribing to your feed and I hope you write again very soon!
I blog often and I genuinely appreciate your content. This great article has truly peaked my interest. I’m going to book mark your website and keep checking for new details about once a week. I opted in for your RSS feed too.
Stake Eth
Rocket Pool
https://crypto-news.xlog.app/How-to-Use-Rocket-Pool-for-Staking-ETH-A-Step-by-Step-Guide
I just couldn’t depart your site prior to suggesting that I extremely enjoyed the standard info a person provide for your visitors? Is gonna be back often in order to check up on new posts
https://medium.com/@CoinNebula/how-to-use-rocket-pool-with-metamask-a-step-by-step-guide-dd7a7466e2b2
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
visit my article https://medium.com/@RyanNakamoto1/minswap-the-best-platform-for-swapping-crypto-in-2025-a3500dc2d5c7
https://steemit.com/crypto/@cryptonewsonline/rocket-pool-the-best-platform-for-staking-eth-in-2025
Simply desire to say your article is as amazing. The clearness for your post is simply nice and that i could think you’re a professional on this subject. Fine together with your permission let me to grasp your feed to keep up to date with forthcoming post. Thanks one million and please keep up the gratifying work.
https://sushi-swap.medium.com/what-is-rocket-pool-a-complete-guide-to-decentralized-eth-staking-f35ef4f9a056
“Sơn Hà Agency Dịch vụ mua bán backlink chất lượng chuyên nghiệp là một công cụ mạnh mẽ giúp bạn cải thiện thứ hạng trang web, tăng lượng traffic và tăng uy tín cho trang web.
https://medium.com/@MiraHayes/how-to-stake-eth-on-rocket-pool-a-complete-guide-7b4038da761f
Причины отсутствия цветения картофеля https://e-pochemuchka.ru/prichiny-otsutstviya-czveteniya-kartofelya/
Robert Lee VanSickle was born Feb 13, 1917 near Almira and entered into rest throughout his sleep on Feb 14, 1974 at his daughter’s home in Lengthy Seaside , CA .
visit my article https://medium.com/@RyanNakamoto1/minswap-the-best-platform-for-swapping-crypto-in-2025-a3500dc2d5c7
https://www.newsbreak.com/crypto-bull-313322310/3799707985806-market-analyst-sees-1500-pump-in-xrp-price-amid-multiple-etf-applications
https://www.newsbreak.com/crypto-bull-313322310/3799707985806-market-analyst-sees-1500-pump-in-xrp-price-amid-multiple-etf-applications
https://www.newsbreak.com/crypto-bull-313322310/3799707985806-market-analyst-sees-1500-pump-in-xrp-price-amid-multiple-etf-applications
Nice article, have a look at my site “https://www.issuewire.com/sushi-swap-the-best-crypto-platform-in-2025-1823683727364009”
https://medium.com/@anthonywalkerfck49/how-to-swap-crypto-on-sushi-swap-a-step-by-step-guide-1d39e9a42974
Nice article, have a look at my site “https://www.issuewire.com/sushi-swap-the-best-crypto-platform-in-2025-1823683727364009”
nice article ave a look at my site “https://www.newsbreak.com/crypto-space-hub-313321940/3799652652916-top-crypto-investments-in-2025-bitcoin-ai-projects-tokenized-assets”
nice article ave a look at my site “https://www.newsbreak.com/crypto-space-hub-313321940/3799652652916-top-crypto-investments-in-2025-bitcoin-ai-projects-tokenized-assets”
Nice article, have a look at my site “https://www.issuewire.com/sushi-swap-the-best-crypto-platform-in-2025-1823683727364009”
nice article ave a look at my site “https://www.newsbreak.com/crypto-space-hub-313321940/3799652652916-top-crypto-investments-in-2025-bitcoin-ai-projects-tokenized-assets”
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to create my own blog and would like to know where u got this from. thanks a lot
nice article ave a look at my site “https://www.newsbreak.com/crypto-space-hub-313321940/3799652652916-top-crypto-investments-in-2025-bitcoin-ai-projects-tokenized-assets”
Nice article, have a look at my site “https://www.issuewire.com/sushi-swap-the-best-crypto-platform-in-2025-1823683727364009”
https://guide-to-spookyswap-r.gitbook.io/en-us/
https://spookyswap-r-4.gitbook.io/en-us/
https://guide-to-spookyswap-r.gitbook.io/en-us/
https://spookyswap-tm-2.gitbook.io/en-us/
https://spookyswap-c.gitbook.io/en-us
https://r-guide-spookyswap-r.gitbook.io/en-us
nice blog, visit my site
I loved as much as you will receive carried out right here. The sketch is attractive, your authored subject matter stylish. nonetheless, you command get bought an edginess over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this increase.
Hey there! I’m at work surfing around your blog from my new iphone 4! Just wanted to say I love reading through your blog and look forward to all your posts! Keep up the superb work!
https://spookyswap-r-3.gitbook.io/en-us/
I’ve bookmarked this post. Really useful info!
Thought you might enjoy this article I found http://school97.ru/vesti20/index.php?PAGE_NAME=profile_view&UID=219576
Thought you might enjoy this article I found http://school97.ru/vesti20/index.php?PAGE_NAME=profile_view&UID=219576
Thought you might enjoy this article I found http://school97.ru/vesti20/index.php?PAGE_NAME=profile_view&UID=219576
I discovered your weblog site on google and verify a couple of of your early posts. Continue to keep up the very good operate. I just extra up your RSS feed to my MSN News Reader. Looking for forward to reading more from you afterward!?
As the decentralized finance (DeFi) space continues to evolve in 2025, SpookySwap has established itself as one of the leading decentralized exchanges (DEXs) on the Fantom Opera blockchain. Known for fast, low-cost token swaps, yield farming, and liquidity rewards, SpookySwap is a powerful tool for traders and DeFi enthusiasts looking to maximize their returns while maintaining full control of their funds.
Woofi Finance helped me manage my budget!
мтс тв
https://wisewayrecruitment.com/employer/inetrnet-domashnij-ekb-3/
мтс интернет
I appreciate the depth of research in this post.
I like looking through a post that will make people think. Also, thanks for allowing for me to comment!
мтс подключить
https://aidesadomicile.ca/employer/inetrnet-domashnij-ekb-2/
мтс подключить
https://spookyswap-c.gitbook.io/en-us
https://spookyswap-c.gitbook.io/en-us
мтс подключение
https://www.refermee.com/companies/inetrnet-domashnij-ekb/
мтс подключить екатеринбург
https://spookyswap-tm-1.gitbook.io/en-us/
The best platforms to securely trade and store your crypto.
Good insights! It’s great to see SpookySwap working hard to improve the user experience with every update.
I prefer spooky swap over other exchanges, way faster.
Any upcoming updates for spookyswap? Excited to see what’s next!
мтс подключить екатеринбург
https://jobs.ezelogs.com/employer/inetrnet-domashnij-ekb/
мтс домашний интернет
Seriously, spooky swap deserves all the praise! Best DEX ever!
Been using spooky swap for years—still my favorite DEX.
Spooky swap offers real-time pricing and minimal swap delays.
мтс тарифы на интернет
https://jobs.careersingulf.com/companies/inetrnet-domashnij-ekb-3/
мтс интернет
https://spookyswap-tm-3.gitbook.io/en-us/
SpookySwap is a decentralized exchange (DEX) on the Fantom Opera blockchain
https://spookyswap-tm-3.gitbook.io/en-us/
It is my belief that mesothelioma is most dangerous cancer. It has unusual traits. The more I really look at it a lot more I am certain it does not work like a real solid cells cancer. In the event mesothelioma is usually a rogue viral infection, hence there is the possibility of developing a vaccine and offering vaccination to asbestos subjected people who are open to high risk involving developing long run asbestos connected malignancies. Thanks for revealing your ideas about this important ailment.
мтс телевидение
https://tayseerconsultants.com/employer/inetrnet-domashnij-ekb/
мтс домашний интернет
Hey there just wanted to give you a quick heads up and let you know a few of the images aren’t loading properly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
мтс подключить
https://healthcarestaff.org/employer/inetrnet-domashnij-ekb-3/
мтс интернет екатеринбург
best crypto site in 2025
https://r-guide-spookyswap-r.gitbook.io/en-us
https://spookyswap.app/
https://spookyswap-14.gitbook.io/en-us/
https://spookyswap-12.gitbook.io/en-us/
https://spookyswap-12.gitbook.io/en-us/
best crypto site https://iziswap.org/
мтс домашний интернет
https://baitshepegi.co.za/employer/inetrnet-domashnij-ekb/
мтс тарифы екатеринбург
best crypto site https://iziswap.org/
мегафон подключение
https://ekb-domasnij-internet-2.ru
мегафон телевидение
Thank you for the good writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
мегафон интернет екатеринбург
https://ekb-domasnij-internet-3.ru
мегафон телевидение екатеринбург
https://x.com/ByteTrailBen/status/1890117049457996023, WOOFi Finance Leading DEX 2025
https://x.com/DjiffardBCNEWS/status/1890119831527321791, WOOFi Finance Leading DEX 2025
WOOFi Finance Trading Guide: How to Trade Crypto in 2025
мегафон подключить
https://ekb-domasnij-internet.ru
мегафон тарифы на интернет
WOOFi Finance Trading Guide: How to Trade Crypto in 2025
Предлагаем услуги профессиональных инженеров офицальной мастерской.
Еслли вы искали ремонт iphone 11 в москве, можете посмотреть на сайте: срочный ремонт iphone 11
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
билайн тв краснодар
https://infodomashnij-internet-krasnodar-2.ru
провайдер билайн
Das bedeutet schnellerer Einstieg fГјr dich und mehr Chancen auf deinem Konto.
сайт билайн краснодар
https://infodomashnij-internet-krasnodar-3.ru
билайн интернет краснодар
сайт билайн краснодар
https://infodomashnij-internet-krasnodar.ru
билайн телевидение
Your webpage does not show up appropriately on my i phone – you might wanna try and repair that
билайн цены
https://plus-domashnij-internet-krasnodar-2.ru
билайн домашний интернет
Hey, you used to write wonderful, but the last several posts have been kinda boring? I miss your super writings. Past several posts are just a little bit out of track! come on!
The subsequent time I learn a weblog, I hope that it doesnt disappoint me as much as this one. I mean, I know it was my choice to learn, but I actually thought youd have something attention-grabbing to say. All I hear is a bunch of whining about one thing that you possibly can repair when you werent too busy searching for attention.
билайн телевидение краснодар
https://plus-domashnij-internet-krasnodar.ru
билайн подключить
I like what you guys are up also. Such smart work and reporting! Carry on the superb works guys I?ve incorporated you guys to my blogroll. I think it’ll improve the value of my website 🙂
Wonderful, what a web site it is! This website provides helpful data to us, keep it up.
билайн подключить краснодар
https://plus-domashnij-internet-krasnodar-3.ru
билайн интернет
сайт билайн краснодар
https://plus-domashnij-internet-krasnodar-2.ru
билайн тарифы краснодар
great post, very informative. I wonder why the other experts of this sector don’t notice this. You should continue your writing. I am confident, you’ve a huge readers’ base already!
билайн подключение краснодар
https://plus-domashnij-internet-krasnodar.ru
билайн домашний интернет
I like it whenever people get together and share thoughts. Great site, continue the good work!
Hi there, You’ve done a fantastic job. I?ll definitely digg it and for my part recommend to my friends. I’m sure they will be benefited from this website.
билайн телевидение краснодар
https://plus-domashnij-internet-krasnodar-3.ru
билайн тв
Heya i am for the first time here. I came across this board and I to find It truly useful & it helped me out a lot. I am hoping to offer one thing again and help others such as you aided me.
I can’t express how much I appreciate the effort the author has put into writing this remarkable piece of content. The clarity of the writing, the depth of analysis, and the wealth of information provided are simply astonishing. His enthusiasm for the subject is apparent, and it has undoubtedly made an impact with me. Thank you, author, for offering your insights and enlightening our lives with this extraordinary article!
Thanks a bunch for sharing this with all of us you really know what you’re talking about! Bookmarked. Please also visit my web site =). We could have a link exchange arrangement between us!
ceramic blade
билайн подключить
https://plus-domashnij-internet-krasnodar-2.ru
билайн домашний интернет
Discover Woofi Finance, the most trusted decentralized exchange for 2025, offering low fees, secure transactions, and seamless crypto swaps. Whether you’re staking or trading, Woofi Finance is the top platform for DeFi users worldwide
Good day! I could have sworn I’ve been to this site before but after browsing through some of the post I realized it’s new to me. Anyhow, I’m definitely glad I found it and I’ll be bookmarking and checking back often!
One thing I would really like to discuss is that fat reduction plan fast can be carried out by the correct diet and exercise. People’s size not merely affects the look, but also the entire quality of life. Self-esteem, depressive disorder, health risks, and also physical ability are impacted in extra weight. It is possible to make everything right and at the same time having a gain. Should this happen, a problem may be the primary cause. While excessive food instead of enough exercising are usually to blame, common medical conditions and key prescriptions can greatly add to size. I am grateful for your post in this article.
Discover the power of MinSwap, the leading decentralized exchange platform offering seamless trading and low fees. Maximize your assets and join the next generation of decentralized finance
Discover CowSwap, the trusted decentralized exchange platform for seamless crypto trades in 2025. With low fees, high security, and fast transactions, CowSwap is a go-to solution for DeFi users worldwide
Discover the future of decentralized finance with Woofi Finance, a cutting-edge platform for seamless crypto staking and yield farming. Maximize your returns with low fees and high rewards. Join the revolution in DeFi today!
Discover CowSwap, the trusted decentralized exchange platform for seamless crypto trades in 2025. With low fees, high security, and fast transactions, CowSwap is a go-to solution for DeFi users worldwide
массаж в подарок женщине москва сертификат
билайн цены
https://plus-domashnij-internet-krasnodar.ru
билайн телевидение
You made some decent factors there. I looked on the web for the difficulty and located most people will associate with along with your website.
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three e-mails with the same comment. Is there any way you can remove me from that service? Thanks!
Discover the power of MinSwap, the leading decentralized exchange platform offering seamless trading and low fees. Maximize your assets and join the next generation of decentralized finance
Discover CowSwap, the trusted decentralized exchange platform for seamless crypto trades in 2025. With low fees, high security, and fast transactions, CowSwap is a go-to solution for DeFi users worldwide
Discover the future of decentralized finance with Woofi Finance, a cutting-edge platform for seamless crypto staking and yield farming. Maximize your returns with low fees and high rewards. Join the revolution in DeFi today!
Discover CowSwap, the trusted decentralized exchange platform for seamless crypto trades in 2025. With low fees, high security, and fast transactions, CowSwap is a go-to solution for DeFi users worldwide
Тут можно преобрести огнестойкие сейфы цена купить сейф несгораемый
билайн подключить
https://plus-domashnij-internet-krasnodar-3.ru
билайн цены
One important issue is that when you’re searching for a education loan you may find that you will need a cosigner. There are many scenarios where this is true because you might discover that you do not possess a past credit ranking so the mortgage lender will require that you’ve got someone cosign the financing for you. Good post.
One thing I’d prefer to reply to is that fat reduction plan fast can be achieved by the perfect diet and exercise. Someone’s size not just affects appearance, but also the complete quality of life. Self-esteem, major depression, health risks, and also physical capabilities are impacted in putting on weight. It is possible to do everything right and at the same time having a gain. If this happens, a condition may be the reason. While a lot food instead of enough physical exercise are usually the culprit, common health conditions and key prescriptions may greatly add to size. Thanks a bunch for your post here.
мегафон тарифы екатеринбург
мегафон подключение екатеринбург
мегафон интернет
I’ll right away seize your rss feed as I can not to find your email subscription hyperlink or e-newsletter service. Do you’ve any? Kindly allow me know so that I may just subscribe. Thanks.
Thank you. I enjoy it!
prepaid mastercard online casino https://magicalcasino.info/legit-online-casinos/ win win casino online
Simply wish to say your article is as surprising. The clarity for your publish is simply excellent and that i can assume you’re knowledgeable in this subject. Well together with your permission allow me to grasp your RSS feed to stay up to date with imminent post. Thanks 1,000,000 and please continue the gratifying work.
мегафон тарифы на интернет
https://plus-ekb-domasnij-internet-2.ru
мегафон екатеринбург
Reliable Boats for Sale
Тут можно преобрести навес автомобильный в Санкт-Петербурге подробно на сайте навесы для машин
If you are going for finest contents like I do, only visit this web site all the time as it offers quality contents, thanks
мегафон интернет екатеринбург
https://plus-ekb-domasnij-internet-3.ru
мегафон подключить
мегафон подключить екатеринбург
мегафон интернет екатеринбург
мегафон тарифы на интернет
Тут можно преобрести купить офисный сейф сейфы для офисов цены
With Stargate Bridge, blockchain transfers are quick, easy, and cost-effective. Join the future of DeFi today!
Try the best blockchain bridge in 2025 – Stargate Bridge offers seamless cross-chain transfers with low fees.
You have made your point!
como descontrolar una mГЎquina de casino online https://shadowcasino.info/tennessee-online-casino/ neue online casinos mit startguthaben
мегафон подключить екатеринбург
https://plus-ekb-domasnij-internet-2.ru
мегафон домашний интернет екатеринбург
Need fast, secure, and low-fee cross-chain transfers? Stargate Bridge is the solution you’ve been waiting for!
Don’t miss out on Stargate Bridge – the top blockchain bridge for seamless cross-chain transfers and enhanced security.
Don’t miss out on Stargate Bridge – the top blockchain bridge for seamless cross-chain transfers and enhanced security.
мегафон интернет
https://plus-ekb-domasnij-internet-3.ru
мегафон тарифы на интернет
мегафон телевидение екатеринбург
мегафон интернет
мегафон телевидение
провайдер мегафон
https://plus-ekb-domasnij-internet-2.ru
мегафон телевидение
As I web-site possessor I believe the content material here is rattling magnificent , appreciate it for your efforts. You should keep it up forever! Good Luck.
Тут можно преобрести продвижение сайтов медицинских услуг продвижение медицинских услуг
мегафон тв
https://plus-ekb-domasnij-internet-3.ru
мегафон подключение
Hi there! I could have sworn I’ve visited this site before but after looking at some of the posts I realized it’s new to me. Nonetheless, I’m definitely pleased I came across it and I’ll be book-marking it and checking back often!
Manta Bridge
I have observed that online education is getting common because accomplishing your degree online has developed into popular solution for many people. Numerous people have not necessarily had a possible opportunity to attend a regular college or university but seek the raised earning possibilities and a better job that a Bachelor Degree grants. Still people might have a degree in one discipline but wish to pursue some thing they now have an interest in.
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I get actually enjoyed account your blog posts. Any way I’ll be subscribing to your feeds and even I achievement you access consistently rapidly.
Manta Bridge
I never had a better trading experience than with Spookyswap. Everything just works seamlessly. The best DEX hands down.
If you’re still using outdated exchanges, switch to Spookyswap. It’s decentralized, secure, and lightning-fast. Perfect for trading in 2025.
Тут можно преобрести сео продвижение медицинских сайтов продвижение медицинских услуг
Cross-chain technology is evolving, and Stargate Bridge is at the forefront. A top-tier choice for DeFi enthusiasts!
Looking for a cutting-edge bridge in 2025? Stargate Bridge is the ideal choice for users who value trust and efficiency.
This site can be a stroll-by for the entire info you wished about this and didn?t know who to ask. Glimpse right here, and also you?ll definitely uncover it.
After exploring a handful of the blog posts on your website, I truly like your way of blogging. I bookmarked it to my bookmark webpage list and will be checking back in the near future. Please visit my web site too and tell me what you think.
Hmm it appears like your site ate my first comment (it was extremely long) so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog. I as well am an aspiring blog blogger but I’m still new to the whole thing. Do you have any tips and hints for newbie blog writers? I’d certainly appreciate it.
It’s a shame you don’t have a donate button! I’d certainly donate to this excellent blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to fresh updates and will share this website with my Facebook group. Chat soon!
I think one of your advertisings caused my web browser to resize, you might want to put that on your blacklist.
Тут можно преобрести продвижение медицинского центра продвижение медицинских сайтов
билайн подключить
https://fmstaffingsource.com/companies/monika/
билайн тарифы кемерово
Hiya very nice web site!! Guy .. Excellent .. Amazing .. I will bookmark your website and take the feeds additionally? I am glad to search out so many useful information right here in the publish, we want develop extra strategies on this regard, thanks for sharing. . . . . .
мтс подключение
https://raida-bw.com/employer/frederick/
мтс домашний интернет кемерово
Can I just say what a relief to search out someone who truly knows what theyre speaking about on the internet. You definitely know how to deliver an issue to light and make it important. More individuals need to read this and perceive this facet of the story. I cant consider youre not more in style because you definitely have the gift.
Many thanks for your post. I want to write my opinion that the expense of car insurance will vary from one policy to another, since there are so many different facets which give rise to the overall cost. Such as, the brand name of the vehicle will have a large bearing on the purchase price. A reliable older family car will have a more affordable premium compared to a flashy racecar.
мтс тарифы краснодар
https://jobs.ethio-academy.com/employer/ingrid/
мтс интернет
мегафон интернет
https://jobs.alibeyk.com/employer/helen/
мегафон телевидение ростов
билайн тарифы кемерово
http://wp10476777.server-he.de/ej/wordpress/jobs-in-christlichen-unternehmen/felix/
билайн домашний интернет
ттк барнаул
https://earthdailyagro.com/employer/ttk-tarif-and-co/
ттк интернет
ттк подключить ростов
http://www.jobteck.co.in/companies/marlene/
ттк интернет ростов
мтс подключить
https://dakresources.com/employer/kathrin/
мтс тв
мегафон тарифы ростов
https://canworkers.ca/employer/mia/
мегафон интернет
билайн подключить кемерово
https://carepositive.com/employer/maybelle/
провайдер билайн
билайн интернет кемерово
https://www.inclusivehires.com/companies/corrine/
билайн интернет
мтс тарифы на интернет
https://empregos.acheigrandevix.com.br/employer/stephany/
мтс домашний интернет
Тут можно преобрести продвижение сайта медицинского центра продвижение сайтов медицинских услуг
Top-rated DeFi platform , SpookySwap
мтс подключить краснодар
https://www.mafiscotek.com/employer/thao/
мтс тв
Best website to swap FTM in 2025 , SpookySwap
мтс интернет
https://eleeo-europe.com/employer/emely/
мтс тв кемерово
мегафон подключить
https://jobs.quvah.com/employer/lois/
мегафон домашний интернет
Fantastic data. With thanks!
online casino stocks https://casinoslotoking.com/new-zealand-online-casino/ online casino anmelden
you’re in reality a just right webmaster. The website loading pace is amazing. It seems that you are doing any distinctive trick. Also, The contents are masterwork. you have done a great activity on this matter!
сайт мтс краснодар
https://job.honline.ma/employer/lynda/
мтс интернет
ттк тарифы ростов
https://www.joboptimizers.com/employer/jerrold/
провайдер ттк
Thanks for expressing your ideas on this blog. Additionally, a myth regarding the financial institutions intentions any time talking about home foreclosure is that the financial institution will not take my repayments. There is a fair bit of time the bank will take payments occasionally. If you are too deep inside the hole, they will commonly call that you pay the actual payment in full. However, i am not saying that they will not take any sort of repayments at all. When you and the financial institution can seem to work some thing out, a foreclosure practice may end. However, in the event you continue to neglect payments wih the new program, the foreclosure process can pick up exactly where it left off.
Incredible a good deal of fantastic facts!
melhor casino online em portugal https://ratingcasino.info/nascar-betting/ free bonus online casino malaysia
You reported this fantastically.
bc online casinos https://combatcasino.info/poker/ gta online casino car
сайт мегафон ростов
https://contractoe.com/employer/evie/
сайт мегафон ростов
мтс тарифы на интернет
https://www.towingdrivers.com/employer/bret/
мтс домашний интернет
мтс цены
https://rabota.newrba.ru/employer/alyssa/
мтс тв краснодар
Nicely voiced certainly! !
best online casinos ireland https://casinoshaman.com/wild-casino-no-deposit-bonus-codes/ most trusted online casino
I like what you guys tend to be up too. This kind of clever work and coverage! Keep up the good works guys I’ve you guys to our blogroll.
I really appreciate this post. I have been looking everywhere for this! Thank goodness I found it on Bing. You have made my day! Thx again
мегафон подключить ростов
https://thesecurityexchange.com/employer/julian/
мегафон интернет
You should be a part of a contest for one of the most useful websites on the internet.
I am going to recommend this blog!
Valuable postings. Regards.
online casinos that accept neosurf https://mgmonlinecasino.us/live-casino-betting/ borgata casino online promotions
Very well expressed certainly! .
australian online no deposit casino https://snipercasino.info/online-casino-canada/ best ainsworth online casino sites
сайт ттк барнаул
https://www.securityprofinder.com/employer/ttk-tarif/
ттк домашний интернет барнаул
You made your stand very clearly!!
best casino online in canada 2021 yukon gold https://casinoslotssaid.com/bitcoin-casino-fast-payout/ pinup online casino aviator
ттк тарифы ростов
https://gst.meu.edu.jo/employer/minda/
ттк телевидение
Kudos, Great information.
casino missions gta v online https://igamingcasino.info/real-money-slots/ stake online casino location
Good stuff, Appreciate it!
australian online casino that accepts paypal https://casinocashstars.com/ online casino in las vegas
сайт ттк ростов
https://globalhospitalitycareer.com/employers/maira/
сайт ттк ростов
Regards, Terrific stuff.
instant cash out online casino https://hotgamblingguide.com/mlb-sports-betting/ hollywood casino columbus online slots
Hello! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche. Your blog provided us useful information to work on. You have done a extraordinary job!
Excellent website. Plenty of useful info here. I am sending it to some friends ans also sharing in delicious. And obviously, thanks for your sweat!
You actually revealed that perfectly!
cepheus star casino online real money https://combatcasino.info/review-cafe/ online casino new 2022
билайн подключить
https://nujob.ch/companies/fletcher/
билайн тарифы на интернет
Hi just wanted to give you a quick heads up and let you know a few of the
images aren’t loading correctly. I’m not sure why but I think its a
linking issue. I’ve tried it in two different web browsers and both show the same results.
Have you ever thought about adding a little bit more than just your articles? I mean, what you say is fundamental and everything. However imagine if you added some great visuals or video clips to give your posts more, “pop”! Your content is excellent but with images and clips, this site could certainly be one of the most beneficial in its niche. Wonderful blog!
мтс тарифы кемерово
https://jobseeker.charisonecare.co.uk/employer/terese/
мтс подключить
Info very well used.!
bandar casino blackjack online https://mapcasino.info/fast-payout-casinos/ island resort and casino online gaming
Nicely put. Kudos.
wind creek casino online games https://uscasinoguides.com/betting-sites/ luckystar online casino real money
мтс домашний интернет краснодар
https://careers.indianschoolsoman.com/employer/sue/
мтс домашний интернет
мегафон интернет
https://skillfilltalent.com/employer/garnet/
сайт мегафон ростов
ттк интернет барнаул
https://www.truckjob.ca/employer/ttk-tarif-solutions/
ттк телевидение
You explained this very well!
superbet casino games online https://igamingcasino.info/mbl-betting/ casino online gratis en espaГ±ol
ттк ростов
http://candidacy.com.ng/employer/2793/rafael/
ттк домашний интернет
билайн домашний интернет
https://thesecurityexchange.com/employer/barbra/
билайн тарифы на интернет
Hello, i think that i noticed you visited my site thus i got here to return the desire?.I am trying to to find issues to enhance my website!I assume its ok to use some of your concepts!!
мтс домашний интернет
https://iraqhire.com/employer/cornell/
мтс тарифы кемерово
With thanks. Quite a lot of content.
casino epoca online https://casinoshaman.com/online-casino-illinois/ free game online casino
мтс тарифы на интернет
https://career.zetapharma.net/employer/bart/
мтс подключить
Heya i am for the primary time here. I found this board and I in finding It really useful & it helped me out much. I am hoping to give something again and help others such as you aided me.
Thanks! Wonderful information.
online casino krasloten https://uscasinoguides.com/cryptoslots-review/ free online no deposit casinos
Superb material. Cheers.
newest usa online casino 2022 https://hotgamblingguide.org/ohio-online-casino-real-money/ legit online casinos for us players
мегафон тарифы ростов
http://app.vellorepropertybazaar.in/profile/paulazaragoza5
мегафон ростов
Thanks for your intriguing article. Other thing is that mesothelioma is generally due to the breathing of material from asbestos fiber, which is a cancer causing material. Its commonly witnessed among individuals in the structure industry who have long experience of asbestos. It’s also caused by living in asbestos covered buildings for years of time, Genetic makeup plays an important role, and some consumers are more vulnerable towards the risk than others.
You made your position pretty effectively.!
caesar palace casino online https://casinoshaman.com/lucky-tiger-100-free-spins/ online casinos klarna
ттк домашний интернет барнаул
https://empregos.acheigrandevix.com.br/employer/ttk-tarif-and-co/
ттк телевидение
You stated this well!
online casino bonus 300 https://onlinecasinoindex.us/online-casino-tennessee-real-money/ australian online casino 2020
After looking over a number of the blog articles on your web page, I seriously like your technique of blogging. I bookmarked it to my bookmark site list and will be checking back soon. Please check out my website too and tell me what you think.
ттк тв ростов
http://recruitmentfromnepal.com/companies/rose/
ттк интернет
Thank you. Ample postings!
master casino game online https://buckscasino.info/ohio-online-casinos/ all right casino online
Cheers! I appreciate this!
online casino games play https://buckscasino.info/online-keno/ online casino texas
Incredible lots of good facts.
usa online casinos no deposit bonus codes 2020 https://eseomail.com/betwhale-app/ casinos online con bonos exclusivos
I can’t express how much I value the effort the author has put into creating this remarkable piece of content. The clarity of the writing, the depth of analysis, and the wealth of information offered are simply impressive. Her passion for the subject is obvious, and it has certainly struck a chord with me. Thank you, author, for offering your knowledge and enriching our lives with this exceptional article!
Тут можно преобрести разработка сайт медицинского центра заказать сайт медицинской клиники
You revealed this well!
hollywood casino online pa app https://magicalcasino.info/review-ignition/ batman the animated series joker casino episode online
Thanks a lot, Loads of stuff.
nice 888 online casino https://casinosonlinenew.com/credit-card-casino/ online casino pros and cons
Perfectly voiced of course! .
beschwerde Гјber online casino https://magicalcasino.info/new-online-casinos/ online spiele kostenlos casino
If you want to grow your familiarity just keep visiting this
website and be updated with the latest information posted here.
Hey are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you require any html coding knowledge to make your own blog? Any help would be really appreciated!
Appreciate it! A lot of material.
can online casinos change rtp https://cryptogamblingguru.com/slot-online/ online casino game real money india
This is very interesting, You’re a very skilled blogger. I’ve joined your rss feed and look forward to seeking more of your fantastic post. Also, I have shared your site in my social networks!
Great post right here. One thing I’d like to say is that most professional areas consider the Bachelor Degree just as the entry level requirement for an online education. While Associate Qualifications are a great way to begin with, completing a person’s Bachelors opens many doors to various careers, there are numerous online Bachelor Course Programs available by institutions like The University of Phoenix, Intercontinental University Online and Kaplan. Another thing is that many brick and mortar institutions offer Online variations of their certifications but generally for a extensively higher charge than the corporations that specialize in online college diploma plans.
Tips nicely utilized!!
online casino spanien https://snipercasino.info/poker-online/ best online casinos review
Once I initially commented I clicked the -Notify me when new comments are added- checkbox and now every time a remark is added I get 4 emails with the identical comment. Is there any method you possibly can remove me from that service? Thanks!
You actually said that adequately!
online casino sperren https://cryptogamblingguru.com/online-betting-apps/ premier online casino
Another important area is that if you are an elderly person, travel insurance regarding pensioners is something you need to really take into account. The older you are, the harder at risk you will be for allowing something negative happen to you while overseas. If you are not really covered by a number of comprehensive insurance policies, you could have many serious problems. Thanks for sharing your hints on this blog.
I just couldn’t depart your site prior to suggesting that I actually enjoyed the standard information a person provide for your visitors? Is going to be back often to check up on new posts
This is nicely expressed. .
online casino immortal romance https://casinoslotoking.com/minnesota-online-casinos/ mobi games online casino
Really a good deal of helpful advice!
app casino online argentina mercadopago https://combatcasino.info/real-money-roulette/ australian online casino microgaming
Very good knowledge. Many thanks!
online casino deutsche lizenz https://cryptogamblingguru.com/nhl-hockey-betting/ amsterdam online casino
Whoa tons of very good info.
casinos online mexico https://igamingcasino.info/casino-games-online/ gta v online diamond casino heist scope out
Whoa quite a lot of great advice!
legal online casinos in nj https://uscasinoguides.com/ufc-betting/ betmgm online casino reviews
Thanks for the strategies you are revealing on this blog. Another thing I would really like to say is the fact that getting hold of duplicates of your credit history in order to examine accuracy of each detail is the first action you have to perform in credit improvement. You are looking to freshen your credit file from destructive details faults that wreck your credit score.
With thanks. Loads of write ups!
casino online kenya https://casinoshaman.com/table-tennis-bets/ nz casino online
Thank you. Ample material.
legal online casino australia https://casinoslotssaid.com/best-minnesota-online-casino/ is yukon gold online casino legit
excellent points altogether, you simply gained a brand new reader. What would you recommend in regards to your post that you made a few days ago? Any positive?
Nicely put. Cheers.
agen judi casino slot joker123 online https://uscasinoguides.com panda master online casino
Thank you for sharing your info. I really appreciate your efforts and I will be waiting for your further post thank you once again.
Hello there, just became alert to your blog through Google, and found that it’s really informative. I am gonna watch out for brussels. I?ll appreciate if you continue this in future. A lot of people will be benefited from your writing. Cheers!
Spot on with this write-up, I absolutely believe this web site needs much more attention. I’ll probably be returning to read through more, thanks for the advice!
Тут можно преобрести создание сайта клиники разработка сайт медицинского центра
I have seen that car insurance corporations know the automobiles which are susceptible to accidents and various risks. In addition, they know what style of cars are susceptible to higher risk as well as higher risk they’ve the higher your premium charge. Understanding the basic basics connected with car insurance will allow you to choose the right kind of insurance policy that should take care of your needs in case you happen to be involved in an accident. Appreciate your sharing a ideas on your own blog.
Hello there, I found your web site by way of Google whilst looking for a similar matter, your web site got here up, it looks good. I have bookmarked it in my google bookmarks.
I used to be very pleased to find this internet-site.I wanted to thanks to your time for this excellent read!! I definitely having fun with every little little bit of it and I’ve you bookmarked to check out new stuff you weblog post.
Thank you for some other informative web site. Where else may just I am getting that type of information written in such a perfect means? I have a challenge that I’m simply now working on, and I’ve been on the look out for such information.
With havin so much written content do you ever run into any issues of plagorism or copyright violation? My blog has a lot of unique content I’ve either authored myself or outsourced but it appears a lot of it is popping it up all over the internet without my permission. Do you know any solutions to help protect against content from being stolen? I’d really appreciate it.
Thanks for the guidelines shared on the blog. Yet another thing I would like to mention is that fat loss is not information on going on a dietary fad and trying to get rid of as much weight as you’re able in a couple of days. The most effective way to lose weight is by using it little by little and obeying some basic ideas which can assist you to make the most out of your attempt to shed weight. You may learn and already be following some of these tips, nonetheless reinforcing knowledge never hurts.
Just wish to say your article is as surprising. The clearness in your put up is simply nice and i can suppose you are a professional on this subject. Well with your permission let me to clutch your feed to keep updated with approaching post. Thank you a million and please carry on the rewarding work.
Hi this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
Providing liquidity on SpookySwap is one of the most effective ways to earn passive income in DeFi https://spokyswap.net/
Купить шампуни онлайн Ульяновск
https://trustgas.ru/
Всёгда лучшая продукция в наличии
Только онлайн
03/03/2025
Great article. It’s very unfortunate that over the last ten years, the travel industry has already been able to to fight terrorism, SARS, tsunamis, bird flu virus, swine flu, plus the first ever entire global economic downturn. Through it the industry has really proven to be strong, resilient and also dynamic, acquiring new strategies to deal with hardship. There are constantly fresh difficulties and chance to which the business must again adapt and respond.
I have recently started a web site, the information you offer on this website has helped me greatly. Thank you for all of your time & work.
Hello, this weekend is pleasant in support of me, for the reason that this moment i am reading this enormous informative article here at my residence.
These days of austerity and relative stress about incurring debt, most people balk contrary to the idea of utilizing a credit card to make acquisition of merchandise and also pay for a holiday, preferring, instead to rely on the particular tried and also trusted procedure for making settlement – hard cash. However, if you have the cash available to make the purchase entirely, then, paradoxically, that is the best time to be able to use the credit cards for several motives.
I additionally believe that mesothelioma is a extraordinary form of cancer that is usually found in people previously subjected to asbestos. Cancerous tissue form while in the mesothelium, which is a defensive lining that covers almost all of the body’s areas. These cells usually form within the lining on the lungs, abdomen, or the sac which actually encircles the heart. Thanks for expressing your ideas.
I’m extremely inspired along with your writing abilities as smartly as with the layout in your blog. Is that this a paid topic or did you modify it yourself? Anyway stay up the excellent high quality writing, it?s rare to peer a great blog like this one today..
What’s up, I read your blogs regularly. Your story-telling style is witty, keep up the good work!
For seamless cross-chain swaps, SpookySwap provides the best experience among Fantom DEXs https://spokyswap.net/
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to more added agreeable from you! By the way, how could we communicate?
https://decormedley.com/features-of-a-penthouse-understanding-the-luxury-and-appeal/
Thanks for revealing your ideas. I’d also like to convey that video games have been ever evolving. Better technology and improvements have helped create realistic and enjoyable games. These kinds of entertainment games were not that sensible when the concept was first of all being tried. Just like other areas of technological know-how, video games way too have had to advance by many years. This itself is testimony to the fast growth of video games.
Hmm is anyone else having problems with the images on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any responses would be greatly appreciated.
Тут можно преобрести продвижение сайтов медицинских услуг продвижение медицинского центра
Good ? I should certainly pronounce, impressed with your web site. I had no trouble navigating through all the tabs and related info ended up being truly easy to do to access. I recently found what I hoped for before you know it in the least. Reasonably unusual. Is likely to appreciate it for those who add forums or anything, site theme . a tones way for your customer to communicate. Nice task..
Many thanks for sharing most of these wonderful threads. In addition, the best travel in addition to medical insurance system can often ease those fears that come with touring abroad. A new medical crisis can rapidly become costly and that’s guaranteed to quickly impose a financial stress on the family’s finances. Having in place the excellent travel insurance package deal prior to setting off is definitely worth the time and effort. Thanks
Superb post however I was wondering if you could write a litte more on this subject? I’d be very thankful if you could elaborate a little bit more. Cheers!
Hello there! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly? My web site looks weird when viewing from my iphone4. I’m trying to find a theme or plugin that might be able to resolve this issue. If you have any recommendations, please share. Appreciate it!
Thanks for your post. Another point is that just being a photographer entails not only difficulties in catching award-winning photographs but in addition hardships in getting the best photographic camera suited to your requirements and most especially hardships in maintaining the quality of your camera. This really is very accurate and noticeable for those photography enthusiasts that are straight into capturing this nature’s eye-catching scenes — the mountains, the actual forests, the actual wild or maybe the seas. Going to these adventurous places surely requires a photographic camera that can meet the wild’s severe conditions.
This is hands down one of the best articles I’ve read on this topic! The author’s comprehensive knowledge and passion for the subject are apparent in every paragraph. I’m so thankful for coming across this piece as it has enhanced my comprehension and stimulated my curiosity even further. Thank you, author, for dedicating the time to create such a phenomenal article!
Howdy! I’m at work browsing your blog from my new iphone! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the excellent work!
lhlld3
Plastic Fabrication
Plastic Fabrication
Plastic Fabrication
Hey very nice blog!
Plastic Fabrication
Touche. Sound arguments. Keep up the good spirit.
Do you have a spam problem on this website; I also am a blogger, and I was wondering your situation; we have created some nice methods and we are looking to swap solutions with others, be sure to shoot me an e-mail if interested.
I have really noticed that credit improvement activity needs to be conducted with tactics. If not, you are going to find yourself causing harm to your positioning. In order to realize your aspirations in fixing your credit history you have to be careful that from this minute you pay all of your monthly expenses promptly prior to their slated date. It really is significant for the reason that by not accomplishing that, all other activities that you will choose to adopt to improve your credit ranking will not be useful. Thanks for discussing your concepts.
Wonderful blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Cheers
Hi! This post could not be written any better! Reading this post reminds me of my old room mate! He always kept chatting about this. I will forward this write-up to him. Pretty sure he will have a good read. Thank you for sharing!
Beginners could possibly construct muscle using simply body weight, but the extra advanced you turn out to be, you may need to regulate the load accordingly. To allow you to get the most out of your exercises, we dug through the prevailing analysis and asked professional trainers for his or her recommendation on how to promote muscle progress through evidence-based hypertrophy training. Even when fats loss happens concurrently and total physique weight decreases, increasing the size of your muscular tissues will mechanically imply rising the weight of your lean mass. Eggs are high in protein and fats that’ll help bolster your muscle-building meal plan. Opt for omelettes with cheese to further up your protein and calorie consumption. When it involves calorie consumption, consuming more calories than you burn (creating a calorie surplus) is necessary to gain muscle, as supported by evidence printed by Frontiers. Nonetheless, you only have limited funds in your recovery account.
In addition to strength coaching, you have to eat enough energy throughout the day to gasoline your body correctly. Protein is crucial nutrient for muscle development, but your body also requires adequate carbohydrates and fat to help energy levels, hormone production, and muscle recovery. If looking to do a minimize and keep as much of your current mass as possible, you may wish to hold your protein intake high and proceed to include constant weight training. The analysis suggests that about one gram of protein per pound of physique weight might help shield lean mass in a calorie deficit (90). You can also increase your calorie burn with extra high-intensity training that includes some body weight workouts -helping to promote fats loss whereas sustaining your strength. Carbs, on the opposite hand, are barely more difficult to convert to body fat than dietary fats and contribute to muscle achieve in distinctive methods.
The actuality is there may not be a precise rep quantity to attempt for throughout all kinds of lifts and individuals variations will always be at play. And working on massive core competencies will add total strength and muscle building capabilities. So if you are simply getting started, do not feel like you have to leap right into Olympic lifts and heavy squats. Instead, take time to build your basis and find a muscle constructing workout plan that meets your private wants.
Think About including MyProtein mass gainer in your food regimen for a small enhance when you discover it difficult to achieve weight or when you practise veganism/have a dietary restriction. Plus, because it’s plant-based, those who are vulnerable to pimples will discover this suitable for them as well. You’ll find this mass gainer contributes to your mass-gaining journey. Since the serving size is humongous, some individuals who use this have taken to proportioning the servings to go properly with their diet, particularly if they’re getting enough vitamins from their meals consumption. This program is designed to construct muscle and strength, so ideally, you will be in a caloric surplus.
Nevertheless, one of the best-tasting mass gainers shakes I’ve taken for an extended time frame. Dymatize says this supplement is good for “hard gainers,” which describes people who wouldn’t have the metabolism or the time to construct major muscle mass. This chocolate-flavored product could attraction to individuals wanting to realize weight and add important vitamins and minerals to their diet. The protein-to-carbohydrate ratio is 1 to five, so it may not suit people who want extra protein and fewer calories. Here, we give you the finest workouts to add to your forearm exercises to not solely construct massive forearms but in addition improve your grip strength. For all these exercises, try including chalk for extra activation. By the time you move on to your 4th train, your deltoids are already going to be firing because of deadlifts and bench presses.
They’ll additionally give you pointers on the method to improve your results. And they’re additionally to help ensure you’re not poor of any micronutrients (vitamins and minerals). Bodybuilding nutrition has been made more complicated than needed. There are so many different diets and lots of the contradict one another. Isolation workout routines are the place you get into shaping your muscular tissues with that deep burn.
A 2019 evaluation checked out 30 studies on different coaching workouts. It means that 3–6 sets with as much as 12 repetitions at a reasonable intensity with subsequent depth increases can maximize overall muscle growth. Alongside with fifty two g of fast-, medium-, and slow-digesting proteins, this product incorporates 17 nutritional vitamins and minerals selected to help muscle restoration, wholesome muscles, and balanced nutrition.
It is entirely attainable to gain muscle with out weights, particularly for newbies. Body Weight exercises, like push-ups, air squats, and strolling lunges, could be an efficient method to building and sustaining lean muscle. Nonetheless, as quickly as these exercises turn out to be too straightforward, you may need to consider rising the resistance with train bands or light weight.
For hypertrophy, working a quantity of muscle groups directly may promote uniform development. For power, working multiple groups directly can enhance general energy. To be effective, the depth you select must be sufficient to generate stress while permitting you to do enough reps to succeed in fatigue. Acute training variables are the basic parts of any coaching program, in accordance with the NAMS. The authors discovered that when the whole quantity is high, you could experience extra power than hypertrophy gains. Nonetheless, hypertrophy positive aspects happen regardless of whether or not the volume load is low or high. Resistance training offers many health benefits besides getting stronger.
Nevertheless, hypertrophy coaching also helps bodybuilders achieve strength. As such, you presumably can focus on energy coaching and nonetheless obtain your weight loss targets. Some folks counsel hypertrophy coaching is best for weight reduction because you carry out more repetitions, which could burn more energy. Most mass gainers also add in some flavoring, plus vitamins and minerals as well.
While real food should all the time come first, some supplements may help. Nevertheless, these ought to be had only after session with a doctor. There’s no need to overcomplicate the tried and true strategies for muscle-making gains. With the best plan and the best self-discipline, you can get seriously shredded in simply 28 days. Lengthy generally identified as the king of plant-based protein, soy-based tofu is a staple in vegetarian and vegan kitchens because of its nutrient density, antioxidant properties, excessive protein content and flexibility. Whereas there are health benefits to all nuts and seeds, pumpkin seeds are one of many stars of the show in relation to muscle health and maintenance.
Whether you’re a fitness center newbie or a seasoned lifter, these insights will turbocharge your routine and catapult your outcomes. Overtraining is attributable to excessive train without adequate rest (44). Having a partner to train with gives you accountability to never miss a exercise and can help motivate you in the gym. This will help you lift more weight and push your self harder. Research even show that a workout partner might help double exercise performance (37, 38).
You could primarily use this as your mass-building grocery listing and be just fine. Extra importantly, a few of this junk can lead to health problems. First, let’s begin with the types of meals you wish to restrict or avoid altogether. The only exception could be if you’re energetic in other sports or activities where you’re burning a considerable quantity of energy. For shoulders, you can at all times mix it up by doing different variations of those workouts (as explained on again day).
Follow the top bodybuilding and health web sites, read books, and proceed to analysis different methods of diet, coaching, relaxation, and supplementation. Perform “forced reps” to coach previous failure and shock the muscles. This coaching methodology must be used sparingly but is fitted to a bulking plan the place calories, vitality, and vitamins are plentiful. Intense exercises can solely go on for thus lengthy without reaching a state of overreaching. However, many weightlifters go away the health club after 30–45 minutes without really breaking sweat. Increasing exercises to 1 hour will place greater stress on the muscle fibers, leading to increased hypertrophy.
Curiously, girls might get well faster than males since estrogen is assumed to play a task in recovering from sore muscle tissue (88). Recovering from sore muscular tissues can involve some light activity, stretching, foam rolling, and correct vitamin. But more so, it simply takes time for the soreness to go away. It is often found in pre-workouts, coupled with another components, or as a single supplement. It has limited research to again up claims however remains in style within the health world.
Muscle tissue burns more energy at rest than fats tissue burns. So by building and retaining extra lean muscle mass, you’ll burn extra energy each day, even when at rest. Many people confuse mass gainers with more general protein powder dietary supplements which are particularly geared in course of gaining muscle, while keeping physique fat positive aspects to a minimum. Constructing muscle requires power availability and creating an energy surplus. Mass gainers provide the extra fuel wanted for intense workouts. A balanced method of cardio and resistance training is crucial when utilizing mass gainers. This combination aids in muscle gain whereas maintaining fats accumulation in examine.
Of course, it goes without saying that mass gainers are antithetical to your aims if you want to shed weight. With a great balance of protein and carb, plus creatine for increased muscle energy, Clear Labs is the clear alternative for athletes. Its minimalist design also helps stop a number of the digestion problems that may be spurred by other mass gainers bloated with sugar and synthetic ingredients. You’d want virtually twice as high of a caloric content of most different mass gainers to get as a lot protein.
If you’re naturally skinny, you can go for the upper end of that interval, but when you find yourself gaining fats simply, it’s higher to goal for the decrease end. Strength training includes utilizing resistance workout routines to build energy and muscle mass. We’ve gone by way of the best mass gainers available on the market and ranked them in accordance with their effectiveness. Quality mass gainers accelerate the repair of broken muscle fibers, reducing soreness and permitting for extra frequent, productive coaching periods. After exercise, your physique begins its restore process, referred to as muscle protein synthesis. This is when amino acids, that are the building blocks of protein, shuttle in and work their magic to help rebuild and repair muscle tissue and help make it stronger. Nonetheless, this process solely occurs if your body has these building blocks (aka amino acids) available.
Whereas many people are experts at gaining weight by accident, what about intentional and wholesome weight gain? At first, it would sound easy, however selling muscle progress may be tough for a lot of people. It requires an optimal stability of diet, training, rest, and consideration of numerous particular person elements. You’ll get most of your carbohydrates early in the day (up to nearly 100g at breakfast), whereas your later meals are mostly protein. This offers your body the amino acids it requires and negates the carbs it doesn’t necessarily need at this time of day. Since insulin sensitivity tends to be decrease later in the day, avoiding carbs helps stop fat acquire.
You can practice far lower than someone else but find yourself getting dramatically better results by simply dialing in your vitamin. Now, I have designed these with the “optimal” volume, but within each PDF, I additionally explain how you could minimize it right down to the minimalist volume we talked about earlier should you needed to save much more time. You in all probability won’t be ready to do as many reps as you could during the earlier set, however you must positively be succesful of get various. Whereas another research changed 3 regular units with 1 normal set adopted by four drop units.
Also visit my webpage :: https://classified-ads.ph/index.php?page=user&action=pub_profile&id=9247
мтс цены
https://www.1elijnuitzendorganisatie.nl/employer/gita9423/
мтс домашний интернет
best seo services
SEO casino content marketing
best malta casinos
сайт мтс новосибирск
https://timviecvtnjob.com/employer/jerri447/
сайт мтс новосибирск
I?d have to examine with you here. Which is not one thing I often do! I get pleasure from reading a post that will make folks think. Also, thanks for permitting me to comment!
мтс интернет новосибирск
http://candidacy.com.ng/employer/3963/penelope7670/
мтс тв новосибирск
SEO casino content marketing
I discovered your blog website on google and check a few of your early posts. Proceed to keep up the very good operate. I just extra up your RSS feed to my MSN News Reader. Searching for ahead to reading extra from you later on!?
new online casinos 2021
сайт мтс новосибирск
https://aicreator24.com/employer/alena6895/
сайт мтс новосибирск
With havin so much written content do you ever run into any issues of plagorism or copyright infringement? My blog has a lot of completely unique content I’ve either authored myself or outsourced but it looks like a lot of it is popping it up all over the web without my permission. Do you know any ways to help reduce content from being ripped off? I’d definitely appreciate it.
best quickspin casinos 2025
провайдер мтс
https://givebackabroad.org/employer/abraham2941/
мтс цены
мтс домашний интернет новосибирск
https://ecsusa.net/employer/flossie3882/
мтс телевидение новосибирск
PIXL DUO 12 6K POD VAPE KIT
PYNE POD CLICK 10K PRE-FILLED POD 5 X MULTIPACK
PYNE POD CLICK 10K PRE-FILLED POD
PIXL DUO 12 6K POD VAPE KIT
мтс домашний интернет
http://connect.lankung.com/read-blog/18391_mts-tv-ekaterinburg-mobilnoe-prilozhenie.html
мтс домашний интернет
мтс подключить
https://talentostartapero.com/employer/inetrnet-domashnij-ekb-2/
мтс подключение
PYNE POD CLICK 10K PRE-FILLED POD
мтс тарифы на интернет
https://www.careerplus.com.au/employer/inetrnet-domashnij-ekb-2/
мтс тарифы на интернет
мтс подключить
https://www.pharmalinkin.com/companies/inetrnet-domashnij-ekb-2/
мтс тарифы екатеринбург
Yet another issue is that video games can be serious naturally with the major focus on finding out rather than enjoyment. Although, it has an entertainment feature to keep your children engaged, every single game is generally designed to improve a specific skill set or area, such as math concepts or scientific research. Thanks for your posting.
мтс екатеринбург
https://cphallconstlts.com/employer/24inetrnet-domashnij-ekb/
мтс тарифы на интернет
Hi there would you mind stating which blog platform you’re using? I’m planning to start my own blog soon but I’m having a hard time making a decision between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your layout seems different then most blogs and I’m looking for something completely unique. P.S Sorry for getting off-topic but I had to ask!
Hello my family member! I want to say that this post is amazing, nice written and include almost all vital infos. I?d like to see more posts like this .
Тут можно преобрести офисные сейфы москва купить сейф в москве для офиса
провайдер мтс
https://horizonsmaroc.com/entreprises/24inetrnet-domashnij-ekb-3/
мтс телевидение
Hi there would you mind letting me know which web host you’re using? I’ve loaded your blog in 3 completely different web browsers and I must say this blog loads a lot faster then most. Can you suggest a good web hosting provider at a honest price? Thanks a lot, I appreciate it!
мтс подключение
https://xpressrh.com/employer/24inetrnet-domashnij-ekb/
мтс телевидение
мтс подключение екатеринбург
http://webheaydemo.co.uk/profile/chauncey37s460
мтс телевидение екатеринбург
I’m truly enjoying the design and layout of your website. It’s a very easy on the eyes which makes it much more pleasant for me to come here and visit more often. Did you hire out a designer to create your theme? Fantastic work!
мтс тарифы на интернет
https://studentvolunteers.us/employer/24inetrnet-domashnij-ekb-2/
сайт мтс екатеринбург
Hi, i think that i saw you visited my weblog thus i came to ?return the favor?.I’m trying to find things to improve my site!I suppose its ok to use some of your ideas!!
Thanks, I’ve been searching for details about this topic for ages and yours is the best I have found so far.
You could certainly see your expertise in the work you write. The world hopes for even more passionate writers like you who aren’t afraid to say how they believe. Always follow your heart.
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Rocket Pool’s Ethereum staking service reaches $1B in TVL
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Rocket Pool’s Ethereum staking service reaches $1B in TVL
Ethereum Foundation confirm $1.25M to Tornado Cash defense
I can’t believe how amazing this article is! The author has done a tremendous job of delivering the information in an captivating and informative manner. I can’t thank her enough for sharing such priceless insights that have undoubtedly enhanced my awareness in this topic. Bravo to him for producing such a masterpiece!
Rocket Pool’s Ethereum staking service reaches $1B in TVL
Ethereum Foundation confirm $1.25M to Tornado Cash defense
Rocket Pool’s Ethereum staking service reaches $1B in TVL
Right now it appears like BlogEngine is the top blogging platform out there right now. (from what I’ve read) Is that what you are using on your blog?
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Rocket Pool’s Ethereum staking service reaches $1B in TVL
Have you ever thought about creating an e-book or guest authoring on other sites?
I have a blog centered on the same ideas you
discuss and would love to have you share some stories/information. I
know my audience would value your work. If you are even remotely interested, feel free to send me an email.
Ethereum Foundation confirm $1.25M to Tornado Cash defense
Ethereum Foundation confirm $1.25M to Tornado Cash defense
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Appreciate it! A good amount of facts!
Feel free to surf to my web site; http://www.jsbs.kr/bbs/board.php?bo_table=free&wr_id=640066
Ethereum Foundation confirm $1.25M to Tornado Cash defense
ethereum casino sites
Ethereum Foundation confirm $1.25M to Tornado Cash defense
Youre so cool! I dont suppose Ive read anything like this before. So nice to seek out any individual with some authentic ideas on this subject. realy thanks for starting this up. this website is one thing that’s wanted on the web, someone with a bit originality. helpful job for bringing one thing new to the web!
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
best no kyc casino
Rocket Pool’s Ethereum staking service reaches $1B in TVL
anonymous bitcoin casinos without deposit
Pretty section of content. I just stumbled upon your website and in accession capital to assert that I get in fact enjoyed account your blog
posts. Any way I will be subscribing to your augment
and even I achievement you access consistently quickly.
I have mastered some points through your site post. One other thing I would like to convey is that there are numerous games on the market designed specially for toddler age kids. They involve pattern acknowledgement, colors, dogs, and models. These normally focus on familiarization as opposed to memorization. This makes little kids occupied without having the experience like they are learning. Thanks
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Phantom takes second spot in Apple’s US App Store utilities category
Phantom takes second spot in Apple’s US App Store utilities category
Elon Musk’s X eyeing capital raise at $44B valuation: Report
My coder is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the costs. But he’s tryiong none the less. I’ve been using Movable-type on a variety of websites for about a year and am concerned about switching to another platform. I have heard fantastic things about blogengine.net. Is there a way I can import all my wordpress posts into it? Any kind of help would be greatly appreciated!
Тут можно преобрести купить сейф москва сейф цена купить
Elon Musk’s X eyeing capital raise at $44B valuation: Report
Phantom takes second spot in Apple’s US App Store utilities category
Phantom takes second spot in Apple’s US App Store utilities category
Great paintings! That is the kind of information that should be shared across the net. Disgrace on the seek engines for now not positioning this submit upper! Come on over and talk over with my site . Thank you =)
Elon Musk’s X eyeing capital raise at $44B valuation: Report
Elon Musk’s X eyeing capital raise at $44B valuation: Report
Elon Musk’s X eyeing capital raise at $44B valuation: Report
Elon Musk’s X eyeing capital raise at $44B valuation: Report
Phantom takes second spot in Apple’s US App Store utilities category
The things i have seen in terms of laptop memory is the fact that there are specifications such as SDRAM, DDR etc, that must match the features of the motherboard. If the pc’s motherboard is pretty current while there are no os issues, changing the memory space literally usually takes under sixty minutes. It’s among the list of easiest laptop or computer upgrade procedures one can think about. Thanks for sharing your ideas.
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Simply desire to say your article is as astonishing. The clearness in your post is simply spectacular and i can assume you’re an expert on this subject. Fine with your permission allow me to grab your RSS feed to keep updated with forthcoming post. Thanks a million and please keep up the rewarding work.
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Why users still make use of to read news papers when in this technological world the whole thing is available on web?
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Trading Bitcoin’s halving: 3 traders share their thoughts
US Bitcoin reserve prompts $370 million in ETF outflows: Farside
Тут можно преобрести купить сейф интернете модели сейфов
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Trading Bitcoin’s halving: 3 traders share their thoughts
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
You actually make it appear really easy along with your presentation but I find this topic to be actually one thing which I believe I’d never understand. It seems too complex and very wide for me. I’m taking a look ahead in your subsequent submit, I’ll attempt to get the hold of it!
Trading Bitcoin’s halving: 3 traders share their thoughts
One thing is that if you are searching for a student loan you may find that you’ll need a co-signer. There are many cases where this is true because you might find that you do not employ a past credit standing so the loan provider will require you have someone cosign the money for you. Thanks for your post.
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
Trading Bitcoin’s halving: 3 traders share their thoughts
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
I have learned some new things through the blog post. Also a thing to I have discovered is that normally, FSBO sellers can reject you actually. Remember, they’d prefer never to use your services. But if a person maintain a gradual, professional connection, offering guide and keeping contact for around four to five weeks, you will usually have the ability to win a business interview. From there, a house listing follows. Thank you
Trading Bitcoin’s halving: 3 traders share their thoughts
Trading Bitcoin’s halving: 3 traders share their thoughts
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Thanks , I have recently been searching for info approximately this subject for a while and yours is the best I have discovered so far. However, what concerning the bottom line? Are you sure about the supply?
Trading Bitcoin’s halving: 3 traders share their thoughts
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
A person essentially help to make seriously articles I would state. This is the very first time I frequented your website page and thus far? I amazed with the research you made to make this particular publish incredible. Wonderful job!
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
The things i have seen in terms of pc memory is that there are features such as SDRAM, DDR etc, that must match up the specific features of the motherboard. If the pc’s motherboard is rather current while there are no operating-system issues, changing the storage space literally usually takes under sixty minutes. It’s among the easiest computer system upgrade processes one can envision. Thanks for spreading your ideas.
Trading Bitcoin’s halving: 3 traders share their thoughts
Analysts : Bitcoin experiencing ‘shakeout,’ not end of 4-year cycle
Trump Opens 300x Leverage Trade After Call with Putin – Is This the Trade of the Century?
Arbitrum whales transfer $18.5M in tokens following $2.3B unlock
Тут можно преобрести навес из поликарбоната для дачи в Санкт-Петербурге подробно на сайте навес под авто
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz respond as I’m looking to create my own blog and would like to know where u got this from. kudos
fantastic points altogether, you simply gained a new reader. What would you recommend in regards to your post that you made a few days ago? Any positive?
Thanks for the suggestions you are discussing on this blog site. Another thing I’d like to say is that getting hold of copies of your credit score in order to check accuracy of the detail is the first action you have to carry out in credit score improvement. You are looking to thoroughly clean your credit file from harmful details flaws that ruin your credit score.
мтс интернет екатеринбург
https://eurosynapses.giannistriantafyllou.gr/employer/24inetrnet-domashnij-ekb/
мтс домашний интернет екатеринбург
เช่ารถกระเช้า
เช่ารถกระเช้าคุณภาพดี
pdacenter.ru – сервис по ремонту бытовой техники
Ремонт посудомоечных машин в Перми в официальном сервисном центре PDACENTER.
Наши инженеры выполняют ремонт любой сложности по дотупным ценам!
กระเช้าระยะสั้น
누누티비
รถกระเช้าไฟฟ้าให้เช่า
누누티비
Hiya very nice site!! Man .. Beautiful .. Superb .. I’ll bookmark your blog and take the feeds also?I’m glad to seek out a lot of useful info right here in the publish, we need develop more techniques in this regard, thanks for sharing. . . . . .
เช่ารถกระเช้าใกล้ฉัน
누누티비
รถกระเช้าสำหรับงานสำรวจ
누누티비
esports domains
[…]usually posts some incredibly fascinating stuff like this. If you池e new to this site[…]
누누티비
Good way of explaining, and nice piece of writing to take facts concerning my presentation focus, which i am going to convey in institution of higher education.
누누티비
Hey there! Would you mind if I share your blog with my twitter group? There’s a lot of people that I think would really enjoy your content. Please let me know. Cheers
Предлагаем услуги профессиональных инженеров офицальной мастерской.
Еслли вы искали ремонт приставок xbox адреса, можете посмотреть на сайте: ремонт приставок xbox цены
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
деньги под птс без отказа
avtolombard-11.ru/ekb.html
где взять кредит под залог авто
Thanks for another excellent article. Where else could anyone get that type of info in such a perfect way of writing? I’ve a presentation next week, and I’m on the look for such information.
Good day! Do you know if they make any plugins to help with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Kudos!
автоломбард залог
avtolombard-11.ru/kazan.html
займ под залог птс авто
Wonderful blog! I found it while searching on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Cheers
Hello! I just wanted to ask if you ever have any trouble with hackers? My last blog (wordpress) was hacked and I ended up losing several weeks of hard work due to no backup. Do you have any methods to protect against hackers?
взять кредит в залог автомобиля
avtolombard-11.ru/kemerovo.html
займ под залог авто
best probiotic for french bulldogs
[…]that may be the end of this article. Right here you値l find some web-sites that we feel you will appreciate, just click the hyperlinks over[…]
clima en chimalhuacan
[…]we like to honor many other net websites around the internet, even though they aren稚 linked to us, by linking to them. Below are some webpages worth checking out[…]
french bulldog texas
[…]always a massive fan of linking to bloggers that I really like but do not get a whole lot of link really like from[…]
где взять кредит под птс
avtolombard-11.ru
деньги под птс машины
Asking questions are genuinely pleasant thing
if you are not understanding anything totally, except this post offers good understanding
yet.
It’s appropriate time to make a few plans for the longer term and it’s time to be happy. I’ve read this put up and if I may I wish to suggest you few fascinating things or advice. Maybe you could write subsequent articles regarding this article. I desire to read even more things approximately it!
french bulldog
[…]usually posts some pretty intriguing stuff like this. If you池e new to this site[…]
деньги под птс автомобиля
avtolombard-11.ru/nsk.html
деньги под залог кредитного авто
автоломбард под автомобиль
https://bewerbermaschine.de/employer/avtolombard-11550/
деньги под залог автомобиля
french bulldog puppies near me
[…]the time to study or stop by the subject material or sites we’ve linked to below the[…]
micro french bulldog
[…]usually posts some very interesting stuff like this. If you are new to this site[…]
floodle puppies for sale
[…]that may be the finish of this article. Here you値l come across some web pages that we believe you値l appreciate, just click the hyperlinks over[…]
Spot on with this write-up, I actually suppose this website wants way more consideration. I?ll most likely be again to read far more, thanks for that info.
кредит под залог авто машины
http://jobshut.org/companies/ichgcp3927/
займ под залог машины круглосуточно
Touche. Great arguments. Keep up the amazing spirit.
gray zone warfare hacks
[…]one of our guests lately proposed the following website[…]
valorant ESP
[…]one of our visitors a short while ago proposed the following website[…]
rust hacks
[…]one of our guests just lately recommended the following website[…]
займ под птс казань
https://dlya-nas.com/employer/avtolombard-111030/
кредит под птс казань
securecheats battlebit
[…]very few websites that happen to become comprehensive beneath, from our point of view are undoubtedly very well worth checking out[…]
займ под залог птс автомобиля
https://givebackabroad.org/employer/ahhand179/
займ под птс автомобиля
I’m in awe of the author’s talent to make complex concepts accessible to readers of all backgrounds. This article is a testament to her expertise and commitment to providing helpful insights. Thank you, author, for creating such an compelling and illuminating piece. It has been an unforgettable experience to read!
Hey there just wanted to give you a quick heads up. The text in your post seem to be running off the screen in Internet explorer. I’m not sure if this is a formatting issue or something to do with internet browser compatibility but I figured I’d post to let you know. The layout look great though! Hope you get the problem solved soon. Thanks
securecheats eft hacks
[…]the time to read or go to the material or sites we have linked to below the[…]
кредит наличными под залог автомобиля
http://www.myjobsghana.com/employer/avtolombard-115030/
кредит под залог авто в кемерово
срочный кредит под залог птс
https://jobflux.eu/employer/23188/redemaxxi5515
кредит под залог птс автомобиля
выгодный кредит под залог авто
https://globalhospitalitycareer.com/employers/zaim-pod-zalog-pts-12293/
деньги под птс без машины
Hmm is anyone else having problems with the images on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any suggestions would be greatly appreciated.
деньги под птс
https://gigit.cz/employer/lgmtech9527/
деньги залог авто москва
кредит под птс автомобиля
https://gigsonline.co.za/employer/zaim-pod-zalog-pts-19991/
наличные под залог автомобиля
Excellent post. I was checking constantly this weblog and I am impressed! Extremely useful information particularly the ultimate phase 🙂 I handle such information a lot. I used to be looking for this particular info for a long time. Thank you and best of luck.
ломбард деньги под залог птс
https://skytechenterprisesolutions.net/employer/behavioralhealthjobs8514/
займ под залог авто круглосуточно
кредит под залог грузового авто
avtolombard-pid-zalog-pts.ru/ekb.html
взять кредит под птс автомобиля
авто под залог
avtolombard-pid-zalog-pts.ru/kemerovo.html
кредит под залог автомобиля кемерово
займ под птс москва
avtolombard-pid-zalog-pts.ru
деньги в залог авто
Oh my goodness! a tremendous article dude. Thanks Nonetheless I’m experiencing issue with ur rss . Don?t know why Unable to subscribe to it. Is there anyone getting similar rss drawback? Anyone who knows kindly respond. Thnkx
кредит под залог машины птс
avtolombard-pid-zalog-pts.ru/nsk.html
кредит под залог авто с плохой кредитной
Tornado Cash – Best Crypto Platform for Protects Your Crypto in 2025
Tornado Cash – Best Crypto Platform for Protects Your Crypto in 2025
оформить займ под птс
zaim-pod-zalog-pts1.ru/ekb.html
залог под птс авто
Hello my family member! I want to say that this post is amazing, nice written and include almost all important infos. I?d like to see extra posts like this .
How to Swap Tokens on ApeSwap: A Complete Guide 2025
Tornado Cash – Best Crypto Platform for Protects Your Crypto in 2025
Tornado Cash – Best Crypto Platform for Protects Your Crypto in 2025
How to Swap Tokens on ApeSwap: A Complete Guide 2025
Thanks for the helpful posting. It is also my opinion that mesothelioma has an really long latency time period, which means that indication of the disease won’t emerge until finally 30 to 50 years after the initial exposure to asbestos fiber. Pleural mesothelioma, that’s the most common type and impacts the area around the lungs, might cause shortness of breath, chest muscles pains, and a persistent cough, which may result in coughing up blood vessels.
How to Swap Tokens on ApeSwap: A Complete Guide 2025
Wow, amazing blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your web site is excellent, let alone the content!
Tornado Cash – Best Crypto Platform for Protects Your Crypto in 2025
Tornado Cash – Best Crypto Platform for Protects Your Crypto in 2025
кредит под залог авто в казани
avtolombard-pid-zalog-pts.ru/kazan.html
деньги под залог авто
How to Swap Tokens on ApeSwap: A Complete Guide 2025
автоломбард залог птс
zaim-pod-zalog-pts1.ru/kemerovo.html
займ под птс авто
How to Swap Tokens on ApeSwap: A Complete Guide 2025
Great write-up, I am regular visitor of one?s website, maintain up the nice operate, and It is going to be a regular visitor for a lengthy time.
автоломбард займ
zaim-pod-zalog-pts1.ru
займ под птс без автомобиля
Heya this is somewhat of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get advice from someone with experience. Any help would be enormously appreciated!
автоломбард новосибирск
zaim-pod-zalog-pts1.ru/nsk.html
деньги под залог птс быстро
How to Swap Tokens on ApeSwap: A Complete Guide 2025
ломбард деньги под залог авто
avtolombard-11.ru/ekb.html
займ под птс без посещения офиса
кредит под птс авто
avtolombard-11.ru/kazan.html
кредит под залог авто
With every little thing that appears to be building within this subject material, many of your perspectives are generally somewhat stimulating. Nevertheless, I beg your pardon, but I do not subscribe to your whole suggestion, all be it exciting none the less. It looks to us that your commentary are actually not completely justified and in simple fact you are generally yourself not even fully convinced of your point. In any case I did enjoy reading it.
Hmm is anyone else encountering problems with the images on this blog loading? I’m trying to determine if its a problem on my end or if it’s the blog. Any suggestions would be greatly appreciated.
срочный кредит под залог птс
avtolombard-11.ru/kemerovo.html
кредит под птс кемерово
mexican candy store
[…]Here is a good Weblog You might Locate Exciting that we Encourage You[…]
chamy rim dips
[…]Sites of interest we have a link to[…]
кредит наличными птс
avtolombard-11.ru
деньги под залог авто машин
займ кредит под птс
avtolombard-11.ru/nsk.html
деньги в долг под птс
займ под залог машины круглосуточно
https://job-daddy.com/employer/avtolombard-zalog-invest7355/
кредиты под залог машины с правом вождения
I’ve been absent for a while, but now I remember why I used to love this site. Thank you, I?ll try and check back more often. How frequently you update your web site?
isla mujeres golf cart rental
[…]the time to read or stop by the content or web pages we have linked to beneath the[…]
автоломбард под птс
https://new.carepositive.com/employer/ahaconsultant280/
займ под залог авто в екатеринбурге
То, что международный брокер Телетрейд вот уже четверть века обманывает клиентов по всему миру, давно ни для кого не секрет.
А за каждой масштабной аферой, конечно же, стоят люди — те, кто придумал, организовал и десятилетиями внедряет в жизнь преступную мошенническую схему. Среди них особо выделяется Сергей Сароян — директор всех украинских офисов Телетрейд.
“Отцом” компании Телетрейд был Владимир Чернобай. Недавно он скончался в Европе, где скрывался от правосудия.
Его наследники — вдова Анна Чернобай и племянник Олег Суворов, и другие прижизненные приспешники Чернобая, продолжают «мошенничество в особо крупных размерах». Именно так квалифицировали деятельность Телетрейд в России и Казахстане, где на брокера уже открыты уголовные дела.
Но в Украине, несмотря на многочисленные жалобы обманутых клиентов, уголовное дело пока не заведено. Похоже, Сергей Сароян знает, на какие рычаги во властных структурах нажимать, чтобы Телетрейд продолжал безнаказанно грабить украинцев.
Сергей Сароян и его роль в глобальном мошенничестве Телетрейд
Сергей Сароян — одиозная личность, с раздутым самолюбием и большими амбициями. Хитрый и двуличный, но при этом трусливый и бесхребетный, он умеет приспособиться и готов прогнуться, когда того требует ситуация. Он с легкостью раздает сладкие обещания, и с такой же легкостью подставляет тех, с кем работает, если обстоятельства складываются не в его пользу. Однажды, правда, это ему не помогло, и мошенника выгнали за воровство. Но обо всем по порядку.
На заре своей карьеры выпускник одесской академии связи Сергей Сароян, работал в телекоммуникационной компании. В попытке продвинуться по картеной лестнице он не нашел ничего лучше, как предложить руководству свои услуги в качестве доносчика, обещая рассказывать, о чем говорят в коллективе и кто с кем в каких отношениях пребывает. Но это предложение не встретило одобрения и стукачу-неудачнику пришлось уволиться. А невостребованные «способности» пригодились несколько позже, в Телетрейд.
В 2005-2006 годах Сергей Сароян был региональным куратором — фактически единоличным правителем Телетрейд в Украине. Ему подчинялись более 30 офисов по всей Украине: Киев, Одесса, Николаев, Харьков, Львов, Черновцы, и другие городах. В ведении Сарояна были также офисы в Европе и Азии — в Италии, Португалии, Польше, Венгрии, Малайзии, и других странах. И деньги лились в карман мошенника рекой — Сергей Сароян получал 3% от инаута (in-out), то есть от разницы между вводом денег клиентов(“in”) и выводом (“out”). Уже тогда в Телетрейд вращались гигантские суммы. В среднем ежемесячно клиенты только украинских офисов Сарояна приносили в компанию от $1 500 000, а выводили около $500 000. То есть in-out, соответственно, составлял $1 000 000, а зарплата Сарояна — более $30 000 в месяц. Но алчность, которая двигала Сарояном, заставляла его направлять всех клиентов в мошеннический проект Телетрейд “Биржа трейдеров”. Торговать на бирже умеет далеко не каждый, и самый логичный выход, который из этого видится — доверить свои деньги профессионалу. Однако брокерская компания не имеет право брать деньги клиентов в управление, и в Телетрейд создали якобы независимый проект «Биржа трейдеров». Мошенник Сергей Сароян именно туда направлял всех клиентов. И подконтрольные трейдеры сливали клиентам депозиты, иногда просто за одну ночь.
«Биржа трейдеров» сливала клиентские деньги, и выводить клиентам уже было нечего. Инаут в украинских офисах в этом случае составлял $1 500 000, а зарплата мошенника вырастала до $45 000 только по Украине. Так Сергей Сароян обворовывал клиентов ни один год. Но, в итоге, был изгнан из компании за воровство. Найти равноценный источник дохода мошеннику не удалось, его образ жизни стал значительно скромнее. Попросту говоря, Сергей Сароян начал стремительно беднеть. Компании не спешили предлагать ему руководящие должности, а коучинг особых прибылей не приносил.
Говорят, что в одну и ту же реку нельзя войти дважды. Но Сергей Сароян сумел. Спустя пять лет его снова позвали в Телетрейд, и он с радостью согласился. Вероятно руководство компании высоко ценит «талант» Сарояна разводить и обворовывать людей.
Сегодня мошенник и хапуга Сергей Сароян вернулся и снова начал кидать клиентов, возглавив все клиентские офисы Телетрейд в Украине, Португалии, Италии, Польше, Румынии и Венгрии. Но теперь уже, как директор, он получает не 3%, а долю со слитых депозитов клиентов. А вот признаваться прилюдно в причастности к мошеннической брокерской компании новоиспеченный директор не спешит. В своих соцсетях Сергей Сароян лишь туманно намекает на консультационные услуги, которые оказывает Телетрейд. Аферист тщательно маскируется, однако обманутым клиентам компании удалось вывести его на чистую воду — они получили доказательство того, что именно Сергей Сароян сегодня стоит у руля украинского Телетрейд. Видеоролик, где он сам признается в этом, был показан на пресс-конференции, состоявшейся в июле 2020 года.
В этом эксклюзивном видео видно как Сергей Сароян принимает в управление украинские офисы компании Центр Биржевых Технологий — дочернего предприятия Телетрейд в Украине.
Эту пресс-конференцию провела инициативная группа обманутых клиентов Телетрейд. Цель, которую они поставили перед собой — вывести на чистую воду брокера-мошенника и все руководство компании, а также вернуть свои деньги. Материалы, собранные обманутыми клиентами демонстрируют схемы развода, которые используются в Телетрейд. В частности, проект «Синхронная торговля», который пришел на смену «Бирже трейдеров». В «Синхронной торговле» уже не люди-трейдеры, а торговые роботы сливают клиентские депозиты. Теперь именно в этот проект заманивает клиентов Сергей Сароян. А затем, в определенный момент, дает программистам компании указание, и те перепрограммируют роботов на заключение заведомо убыточных сделок. Так депозиты клиентов сливаются в ноль.
Сергей Сароян опустошает карманы украинцев и подрывает экономику страны
Эти мошеннические схемы давно попали в поле зрения правоохранительных органов в России — уголовное дело на Телетрейд там завели еще несколько лет назад.
Последовали примеру российских коллег и в Казахстане, где уголовное производство началось летом 2020 года. Руководители казахского филиала Телетрейд и дочерней компании Wall Street Invest Partners сейчас находятся в следственном изоляторе.
Чтобы замять уголовные дела в России, руководители Телетрейд Сергей Шамраев, Олег Суворов и Мингиян Манжиков дают взятки чиновникам в Следственном Комитете РФ — ежемесячно «отстегивают» им около 20% от поступлений, а это сотни тысяч. И не рублей, а долларов. По инсайдерской информации руководство Телетрейд в России заставляют также финансировать боевые действия на Востоке Украины — мошенники отдают на это еще 10% от поступлений. Если рассматривать деятельность Телетрейд и с этой стороны, то мошенник Сергей Сароян, как директор Телетрейд, не только обворовывает своих сограждан страны, а еще и финансирует боевиков ДНР и ЛНР, отнимающих жизни украинцев.
Вызывает удивление тот факт, что в Украине деятельность Телетрейд на протяжении четверти века никто не проверяет. Количество обманутых клиентов брокера огромно. Мошенниками ежемесячно выводятся в офшоры миллионы долларов. Но пока правоохранительные органы не замечают, или не хотят замечать, противозаконной деятельности брокера. По сведениям из источников внутри компании Сергей Сароян рассказывает своим подчиненным — управляющим офисов в Украине, что им не нужно ничего бояться, так как руководство Департамента киберполиции Украины сидит у него на «зарплате». Вот так безнаказанно (пока!) Сергей Сароян разоряет украинцев, подрывает экономику Украины и спонсирует российскую агрессию на Донбассе.
автоломбард под залог птс
http://minority2hire.com/employer/avtolombard-zalog-invest3780/
деньги под залог авто в казани
займ под залог птс авто
https://www.ahrs.al/punesimi/msgsec6129/
кредит под залог птс
займ под птс авто
https://cphallconstlts.com/employer/avtolombard-zalog-invest886/
взять деньги под залог машины
автоломбард в кемерово под залог птс
https://okoskalyha.hu/employer/anetastaffing3595/
ломбард займ под птс
By my observation, shopping for electronics online may be easily expensive, nonetheless there are some tricks and tips that you can use to obtain the best products. There are constantly ways to discover discount specials that could help make one to come across the best electronic devices products at the cheapest prices. Thanks for your blog post.
деньги залог птс авто
https://jobs1.unifze.com/employer/avtolombard-114874/
где взять кредит под птс
Hey very nice website!! Man .. Beautiful .. Superb .. I’ll bookmark your site and take the feeds additionally?I am happy to find a lot of helpful information right here in the post, we’d like work out more strategies on this regard, thanks for sharing. . . . . .
french bulldog blue color
[…]Wonderful story, reckoned we could combine a handful of unrelated data, nonetheless genuinely worth taking a search, whoa did one particular understand about Mid East has got far more problerms too […]
деньги под птс круглосуточные
http://fatims.org/employer/avtolombard-116337/
получить деньги под залог птс
займ под залог авто
https://cannabisjobs.solutions/companies/ishayoga8220/
машина под залог
Wow! This could be one particular of the most beneficial blogs We’ve ever arrive across on this subject. Basically Great. I am also a specialist in this topic so I can understand your hard work.
in vitro fertilization mexico
[…]although internet sites we backlink to below are considerably not connected to ours, we feel they are essentially worth a go by means of, so have a look[…]
Generally I do not read article on blogs, but I wish to say that this write-up very forced me to try and do it! Your writing style has been amazed me. Thanks, very nice article.
dump him shirt
[…]we came across a cool web site that you just may well take pleasure in. Take a appear if you want[…]
hairdresser in houston
[…]Here is a superb Weblog You may Discover Intriguing that we Encourage You[…]
linh hoang
[…]Here is a superb Weblog You may Uncover Intriguing that we Encourage You[…]
круглосуточный автоломбард
avtolombard-pid-zalog-pts.ru/ekb.html
деньги под залог птс машины
french bulldog puppies for sale houston texas
[…]below you will find the link to some web-sites that we think you’ll want to visit[…]
кредит под птс кемерово
avtolombard-pid-zalog-pts.ru/kemerovo.html
автоломбард займ под птс
french bulldogs to rescue
[…]always a large fan of linking to bloggers that I love but don稚 get a good deal of link adore from[…]
sole mare vacanze t-shirt
[…]Sites of interest we have a link to[…]
автоломбард под авто
avtolombard-pid-zalog-pts.ru
займ залог авто
늑대닷컴
[…]just beneath, are many totally not related websites to ours, even so, they may be surely worth going over[…]
Crypto market news
Trending blockchain news
автоломбард под птс новосибирск
avtolombard-pid-zalog-pts.ru/nsk.html
взять кредит под залог птс
richest vietnamese in america
[…]here are some links to web sites that we link to because we consider they are really worth visiting[…]
iZiSwap
Trending blockchain news
автоломбард под залог птс
zaim-pod-zalog-pts1.ru/ekb.html
быстро деньги под птс
This week’s alpha
iZiSwap staking
Pretty portion of content. I just stumbled upon your weblog and in accession capital to say that I get in fact loved account your blog posts. Anyway I will be subscribing to your feeds or even I success you get entry to persistently rapidly.
iZiSwap
кредит под птс
avtolombard-pid-zalog-pts.ru/kazan.html
автоломбард
займ под залог машины
zaim-pod-zalog-pts1.ru/kemerovo.html
кредит в залог автомобиля
лучший интернет провайдер екатеринбург
domashij-internet-ekaterinburg001.ru
подключить интернет
лучший интернет провайдер екатеринбург
domashij-internet-ekaterinburg002.ru
интернет по адресу екатеринбург
joyce echols
[…]we came across a cool web site that you could get pleasure from. Take a appear if you want[…]
Great ideas! Concentrated Wisdom [ “https://concentratedwisdom.com/ ] truly offers a fresh perspective on personal growth.
I love how your material dives deep into self-improvement and practical knowledge.
Podcasts like yours make it much easier to learn useful lessons that can be applied in everyday living.
If someone is searching for the perfect Podcast for Personal
Growth it should be a top choice! Thank you for your amazing efforts.
I’m looking at the next episode! In addition, I’ve am currently exploring similar subjects on my blog, and would love to hear from you about your experiences.
Keep inspiring one another!
Read more about : Concentrated Wisdom
This blog post offers the most fascinating insight into the intricate area in wastewater treatment.
It’s essential tto understand the complexity that are involved in controlling and optimizing our water resources.
Discussions about the modern wastgewater treatment plants and the vitall
roe oof wastewater treatment companies highlights the dedicatikon to providing effective wastewater solution as well as a
complete wastewater treatment solution. It is
important to focus upon wastewater purification can be especially pertinent iin the current climate of environmental
degradation.
I als appreciate tthe mention of various approaches, including advanced systems like
sewage treatment plants aand more simple, yet efficient,
methods suh as sewage treatment. It’s fascinating to know more about johkasou system and its uses, as well as the importance of both domestic sewage
treatment plnt options for residents in residential arras and robust industrial wastewater treatment
as well as industrial wastewater treatment plants for large-scale requirements.
This is an extremely important subject that this blog
provides important light on the subject.
Check This Article about : industrial wastewater treatment plants
It’s a great tool! It is a great resource! printable habit tracker can be a straightforward but
effective tool for building the habit of being cobsistent and remain engaged.
I like hhow your tracking tools are nicely organized and simple too use.
They are perfect for creating and reaching indifidual targets.
The visual tracking of habits can make an enormous distinction in staying onn track.
We appreciate you for providing these useful templates!
We look forward to examining further of yoour offerings.
Additionally, I wrote a piece about the process of habit-forming and I would
like to hear fdom youu about your experiences.
You are doing a fantastic job!.
Read more about : Printable habit tracker
провайдеры интернета в екатеринбурге
domashij-internet-ekaterinburg003.ru
домашний интернет
Fanttastic article! The high pressure waater pumps are vital for numerous industrial
and commercial application, and your selection of the high-pressure pump is top
of the line. I appreciate the detailed insights about vertical multistage centrifugal pumps and
horizontal multistage centrifugal pumps because they’re essential for
efficient water transfer. Your knowledge in CNP pumps as well
as high-pressure centrifugal pumps is admirable. It’s wonderful too find an organization that can provide reliable centrifugal pumps for diverse demands.
Looking forward to exploring more about
your producys as well as your innovations in thiss area.
Keep it up!
Read more about :
Great resource! Finding trustworthy QuickBooks classes in Bangalore
can be challenging, andd this platform offer comprehensive advice for beginner and experienced users alike.
Learning QuickBooks efficiently is vital for managing finances efficiently, and I appreciate the structured
approach you provide. If anyone is looking for an expertly-guided QuickBooks
classes in Bangalore it is definitely worth checking out.I
look forward to hearing more information from yyou and
your team!
Read more about : Quickbooks Training in Bangalore
Excellent resource! Dosing pumps have a ital role in exact chemical dosing for diffeent industries.
your knowledge iin the field iis remarkable. From the chsmical dosing pump to metering pumps as
well as Milton Rooy dosing pumps the solutions you offer seem
to cover a wide range of applications. I also found your knowledge regarding washing pumps, dishwasher pumps pumps, dishwashers
and dosing machines for chhlorine extremely useful for thee industrial and household needs.
Your range iin Pumps for Injecta appears to bbe promising for providing accuracy
and effectiveness in Dosing chemicals. Looking forward to learning more about
your developments in this area!
Read more about : injecta pumps
boston terrier for sale in massachusetts
[…]usually posts some quite interesting stuff like this. If you池e new to this site[…]
My partner and I stumbled over here different web page and thought I may as well check things out. I like what I see so now i’m following you. Look forward to finding out about your web page repeatedly.
Fantastic ideas! Access to safe as well as safe water
is vital Your knowledge iin RO plants and water treatment options
is outstanding. It is crucial to have the reliability of a water treatment
plant for household and industrial use cannot be overstated.
I appreciate how your drinking water treatment and reverse osmosis plants aid in sustainabgility as well as water
purification. Solutions like industriaql RO plants, softener systems, as well as rainwater harvesting are game-changers
for making sure that we have safe water access.
I am looking forward to knowing more about the latest water purification technologies.
Keep up the great work!
Read more about : rain water harvesting
dog probiotic
[…]here are some links to internet sites that we link to mainly because we consider they’re worth visiting[…]
One more thing I would like to mention is that rather than trying to fit all your online degree programs on days that you finish off work (because most people are drained when they return home), try to arrange most of your classes on the week-ends and only a couple courses for weekdays, even if it means a little time away from your weekend break. This is beneficial because on the week-ends, you will be far more rested along with concentrated upon school work. Thanks a bunch for the different tips I have figured out from your weblog.
Как проверить Esperio на признаки мошенничества?
Чтобы проверить компанию на наличие жалоб и эпизодов введения клиентов в заблуждение, воспользуйтесь бесплатным сервисом ВСЯ ПРАВДА. Скопируйте адрес интересующего сайта и вставьте его в форму. Отправьте заявку и получите полное досье о компании. Также рекомендуем обращать внимание на отзывы других пользователей.
Как получить максимум информации о компании Esperio
Если компания надежная, то всю необходимую информацию можно найти в открытом доступе на сайте организации: государственную лицензию на оказание услуг, стаж работы, политику отношений с клиентами. Такие компании доказывают свою надежность сильной репутацией, поэтому обязательно читайте отзывы других клиентов.
Как отличить официальный сайт Esperio от ресурса мошенников?
Чтобы не попасться на поддельные сайты для хищения средств и личных данных потребителей, нужно проверить корректность доменного адреса, наличие протокола https, содержание пользовательского соглашения. Если вы заметили опасный сайт, сообщите о нем на.
Как вывести деньги от брокера Esperio?
Надежные поставщики услуг проводят прозрачную политику платежей. Документ со всеми правилами и ограничениями должен быть опубликован на официальном сайте компании. Если предприятие удерживает ваши средства и отклоняет заявки на вывод, получите консультацию по чарджбэку от экспертов ВСЯ ПРАВДА
Как распознавать мошенников самостоятельно?
Обращайте внимание на информацию о компании – она должна быть в открытом доступе и не вызывать сомнений. Будьте бдительными, если вас просят оплачивать услуги наперед или требуют доступ к личным данным. А также относитесь критически к предложениям быстро и легко заработать.
Что делать, если личный кабинет на сайте брокера заблокирован?
Лицензированные брокеры временно ограничивают доступ за нарушение своих правил. Это исправляется отправкой недостающих документов, дополнительной оплаты не требуется. Если же брокер не доказал свой на 100% легальный статус, если начал требовать деньги за разблокировку счета — это признаки мошенничества. Не платите таким компаниям, они просто вымогают деньги и готовятся ограбить клиентский счет, чем и зарабатывают на самом деле. Разблокировать счет у брокера-мошенника и спасти деньги с него можно только с экспертной поддержкой.
Что делать, если сайт брокера не открывается?
Проверьте технические проблемы на вашей стороне, почитайте отзывы других клиентов компании. Если причина закрытия сайта на стороне брокера — это признак скама. Если сайту брокера можно открыть только через VPN — значит, российские провайдеры заблокировали доступ к нему по предписанию надзорных органов за мошенничество. В любом случае важно восстановить доступ к своему счету и вывести деньги от брокера как можно скорее.
Как правильно вернуть отправленные компании-мошеннику деньги?
Борьба с преступлениями — работа правоохранителей, но возвратом депозитов они не занимаются. Вернуть деньги отправителю — это банковская процедура чарджбэк, для которой мошенничество не является основанием. При задаче вернуть утраченное потребуется профессиональная помощь , чтобы использовать chargeback к своей пользе.
Как подать заявление, чтобы гарантированно запустить возврат депозитов?
Его важно составить по всем правилам международной процедуры chargeback. Особую сложность представляет выбор банковского кода из ограниченных вариантов и доказательства соответствия ему. Малейшая неточность обеспечит законный отказ, поэтому пригодится экспертная поддержка экспертная поддержка.
На каком основании можно опротестовать перевод денег с карты брокеру или инвесткомпании?
В нормативных актах перечислены основания для банковской процедуры chargeback: от ошибок по техническим причинам до введения в заблуждение об оказываемых услугах. Для каждого предусмотрен специальный международный банковский код, мотивированный выбор которого стоит поручить профессионалам. Заявку с неверным кодом отклонят.
Финансовая компания работает честно или обманывает: как узнать?
Тщательно изучить все показанные ею документы. Установить их подлинность по банкам данных официальных инстанций. При недостаточности собственных компетенций диагностику можно поручить профессионалам, в т. ч. бесплатно
Как отделить фейковые отзывы о брокере от настоящих?
Обращайте внимание на периодичность публикаций, качество фактуры, хвалебную или более объективную тональность с учетом недостатков. Надежнее всего получить оценку пласта отзывов и самого брокера у экспертов.
Как отличить официальный сайт брокера от подделки?
Стоит как минимум проверить историю доменного имени, наличие клонов и сертификата сайта. В случае затруднений можно делегировать проверку специалистам — краткую экспертизу можно получить бесплатно.
fertility institute of nj
[…]please pay a visit to the web pages we stick to, like this one particular, as it represents our picks through the web[…]
70918248
References:
http://git.jishutao.com/mitchelcastano
A well-written, informative blog! I am truly
impressed byy the in-depth details you’ve offered.
It’s nnot easy tto find such clear and genuine information,
especially when itt comes to topics related to real estate
such as Land foor Sale in Namakkal. Your information stands
out because of iits accuracy and local relevance and makes it an invaluable source for pospective buyers as well as investors.
Keep going with the good work. Your efforts really help consumers make educated decision-making.
I’ll be sure to viisit yoir blog frequently for furtherr information, particularly about Land
for Sale Namakkal. I wish you continued success and looking forward too seeing your blog posts continuje
to be amazinbg in the near future. You’re doing aan amazing job–keep
your momentm up!
Read Moore About Land for Sale in Namakkal
домашний интернет
domashij-internet-kazan001.ru
провайдеры по адресу дома
подключить интернет казань
domashij-internet-kazan002.ru
провайдеры по адресу казань
провайдер по адресу
domashij-internet-kazan003.ru
подключить интернет в квартиру казань
Excellent job on yoour informative blog! I appreciate the time and
effort that you’ve put into providing the most valuable knowledge.
The way you’ve explained the potential and opportunities
in the property market particularly in Salem and the surrounding
areas, is inspiring and helpful for readers such
as me who are considering possibilities for investinbg in property.
Yourr content is clear entertaining, informative, and illustrates
thhe value of taking a look at the possibility oof byying
a pot in Salem. Keep it up! Your blog is aan eccellent source for those interested inn making wise
real esatate choices. Looking forward to reading the next posts in the
future. Don’t stop sharing your wisdom and helping others grow.
There’s a new faithful fan here!
Read More About Plots for Sale in Salem
провайдер интернета по адресу москва
domashij-internet-msk001.ru
домашний интернет в москве
70918248
References:
steroid stacks for beginners – https://video.office.saltworks.pl/@reaganbouldin?page=about,
провайдеры интернета в москве
domashij-internet-msk002.ru
интернет домашний москва
Heya i am for the first time here. I found this board and I find It really useful & it helped me out a lot. I hope to give something back and aid others like you aided me.
провайдер по адресу москва
domashij-internet-msk003.ru
интернет провайдеры москва по адресу
интернет тарифы нижний новгород
domashij-internet-nizhnij-novgorod001.ru
провайдеры по адресу дома
проверить интернет по адресу
domashij-internet-nizhnij-novgorod002.ru
домашний интернет нижний новгород
Great post. I was checking constantly this weblog and I am inspired! Very useful information specially the last section 🙂 I maintain such info much. I was looking for this particular information for a long time. Thanks and good luck.
Howdy! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
интернет тарифы нижний новгород
domashij-internet-nizhnij-novgorod003.ru
провайдеры интернета в нижнем новгороде по адресу
you’ve an ideal blog right here! would you prefer to make some invite posts on my blog?
подключить интернет тарифы новосибирск
domashij-internet-novosibirsk001.ru
интернет провайдер новосибирск
Nice post. I be taught one thing more challenging on totally different blogs everyday. It can at all times be stimulating to learn content material from different writers and observe a bit one thing from their store. I?d want to make use of some with the content material on my blog whether or not you don?t mind. Natually I?ll provide you with a hyperlink on your internet blog. Thanks for sharing.
интернет по адресу дома
domashij-internet-novosibirsk002.ru
провайдеры новосибирск
интернет провайдеры по адресу дома
domashij-internet-novosibirsk003.ru
интернет провайдеры по адресу новосибирск
недорогой интернет санкт-петербург
domashij-internet-spb001.ru
лучший интернет провайдер санкт-петербург
In other words, how they work in the body to promote muscle development, performance enhancement, fat loss, and other effects. There are other androgenic-type side effects that some SARMs can cause, apart from hair loss. However they’ll primarily only have an result on you if you’re susceptible already, and a massive quantity of SARM users don’t experience noticeable androgenic effects at all. The lack of estrogen (which men need at very low levels) is the primary purpose you want a testosterone base on SARMs as a result of SARMs don’t convert to estrogen as testosterone steroids can.
NPP stands for Nandrolone Phenylpropionate, which is a well-liked anabolic steroid. It is a modified form of nandrolone, which is a naturally occurring hormone in the body. If you’re considering utilizing anabolic steroids, it’s necessary to understand the variations between the assorted options available to you. For the performance enhancer an necessary subject of debate is commonly stacking as proper stacking will guarantee results of steroidation are of the highest attainable nature.
The greatest PCT medication to use are normally in the SERMs category – Clomid and Nolvadex. The timing of your PCT cycle after utilizing Sustanon will as quickly as again also be influenced by some other steroid compounds you’re using. Sustanon’s longer half-life total means your PCT for this specific steroid should be started about three weeks after your final injection to prevent the crash in testosterone ranges that can otherwise occur.
Some of the larger mg tabs such because the 50 mg tabs are actually a pain in the ass to me, as a outcome of I need to chop them up. I’ve tried “pulse cycling” earlier than (only operating orals on coaching days in bigger amounts), taking 1 large dose an hour before I prepare, and I by no means get as strong doing it that method. I’ve always found any oral to work higher in smaller dosages all through the day quite than just 1 massive dosage once per day. Anavar promotes muscle growth and with good discipline and legit Anavar, one can do an awful lot of adjusting in a pair brief months. NPP, on the other hand, is a more potent steroid than Anavar and is generally used for bulking. While Anavar is considered to be a light steroid, it can still cause unwanted effects. If on an applicable Oxandrolone dose, you are able to keep a reasonable testosterone degree, then good, however many are not, which means this principle and protocol is counterproductive.
However, it is extremely frequent amongst athletes who are not bulking at all, and it even has a use in some slicing cycles. The excellent news is, when stacking Deca Durabolin we are going to find well it stacks well with all anabolic steroids. The addition of Testosterone will result in considerably greater muscle and strength positive aspects, with Testosterone typically getting used as a bulking compound.
Correct food regimen, training, and cycle help are very important for getting essentially the most out of an Anavar cycle safely and successfully. The downside to utilizing Anavar continuously is that we see testosterone suppression exacerbate and LDL levels of cholesterol stay elevated for a sustained time period. Consequently, a person’s pure testosterone production will take longer to get well when lastly coming off Anavar. Previously, we cited a research that acknowledged men taking 20 mg a day for 12 weeks experienced a 45% lower in testosterone levels. This was an extreme cycle length, with a regular cycle length of 6–8 weeks for males. From this examine, we are ready to conclude that pure testosterone production is likely to stay fairly excessive if a average dose or cycle is performed. Anavar’s ability to extend energy is principally due to it being exogenous testosterone.
Winstrol is among the most popular steroids on Earth, so nearly all suppliers will at all times have it in inventory. It’s thought-about a comparatively low-cost anabolic steroid and is undoubtedly more affordable than Anavar (to which it’s often compared). The side effects of Winstrol, that are nearly a certainty for all users, will nearly at all times be the idea for negative reviews and experiences with this steroid.
Anvarol’s key components embrace ATP (adenosine triphosphate) and BCAAs (branched-chain amino acids), which improve vitality and assist muscle restoration. Anavar, or oxandrolone, proves to be an exceptional cutting steroid, successfully burning fat while preserving muscle mass. By increasing testosterone production, Anavar boosts the body’s metabolic fee, accelerating fat burning. On the opposite hand, Anavar focuses on cutting cycles, catering to those in search of to shed fats while preserving the hard-earned muscle positive aspects achieved throughout bulking phases.
A big good factor about Sustanon for testosterone alternative is to reduce the variations or ups and downs in your testosterone levels daily – as long as you’re injecting it on an everyday schedule. They usually are not related with the higher doses only, yet we cannot deny that laying with the dosage; paying no consideration to the possible risks will increase the mess of the nasty side effects. Right Here, we will focus on every thing you have to find out about this well-liked anabolic steroid, including its advantages, unwanted aspect effects, and how to use it safely. We may also cowl the newest analysis and information related to Winstrol, so keep tuned for informative and interesting content. It wouldn’t be an sincere evaluation without highlighting the unwanted facet effects experienced by some customers. Some of essentially the most commonly reported issues have been fluctuations in mood, modifications in libido, and in some cases, physical inconveniences like zits, hair loss, or gentle nausea.
These unwanted side effects, coupled with the possible issues to your longer-term health, make Winstrol a high-risk option no matter who you may be. The closest natural and authorized alternative to Winstrol I’ve found thus far is Win-Max. This makes the hair from each follicle thinner and shorter; over time, the follicle dies, which implies no more hair development. When this happens to 1000’s of follicles without delay, you will experience dreaded baldness, and it typically occurs in a familiar M-shaped sample on the pinnacle – hence the name male pattern baldness. Some individuals may have no zits on Winstrol, and a few will see severe flare-ups and increased oily skin. This is another genetically dependent aspect effect, though you can try to take measures to mitigate it somewhat by preserving a clear pores and skin regime.
Anavar is not any exception to this rule and is very true for ladies since Oxandrolone comparatively is a mild steroid. So, those that are involved about their libido or intercourse drive ought to reduce the quantity of Anavar when on its cycle or even use a pure various such as ACut from Brutal Drive. Another necessary factor is that Anavar may be consumed in smaller quantities if you finish up really concerned in regards to the side effects.
References:
what do steroids do to your body, https://10-4truckrecruiting.com/companies/side-effects-of-anavar/,
узнать провайдера по адресу санкт-петербург
domashij-internet-spb002.ru
провайдеры домашнего интернета санкт-петербург
провайдеры домашнего интернета санкт-петербург
domashij-internet-spb003.ru
интернет по адресу дома
провайдер по адресу екатеринбург
domashij-internet-ekaterinburg001.ru
домашний интернет тарифы
лучший интернет провайдер екатеринбург
domashij-internet-ekaterinburg002.ru
провайдеры домашнего интернета екатеринбург
провайдер интернета по адресу екатеринбург
domashij-internet-ekaterinburg003.ru
провайдер по адресу
интернет провайдеры в казани по адресу дома
domashij-internet-kazan001.ru
провайдер интернета по адресу казань
mexican candy store near me
[…]Here is a good Weblog You might Find Fascinating that we Encourage You[…]
mexican candy store near me
[…]we came across a cool web site that you just may well enjoy. Take a search in case you want[…]
подключить интернет тарифы казань
domashij-internet-kazan002.ru
домашний интернет в казани
Interesting post here. One thing I’d like to say is the fact that most professional domains consider the Bachelor Degree as the entry level standard for an online college degree. Whilst Associate Certifications are a great way to begin, completing ones Bachelors presents you with many good opportunities to various employment goodies, there are numerous internet Bachelor Diploma Programs available through institutions like The University of Phoenix, Intercontinental University Online and Kaplan. Another concern is that many brick and mortar institutions offer you Online versions of their qualifications but generally for a substantially higher fee than the corporations that specialize in online higher education degree programs.
mexican candy store near me
[…]always a significant fan of linking to bloggers that I like but really don’t get a whole lot of link enjoy from[…]
интернет провайдеры в казани по адресу дома
domashij-internet-kazan003.ru
недорогой интернет казань
дешевый интернет москва
domashij-internet-msk001.ru
провайдеры по адресу москва
mexican candy store near me
[…]check below, are some entirely unrelated websites to ours, even so, they’re most trustworthy sources that we use[…]
linh hoang
[…]below you値l locate the link to some websites that we assume it is best to visit[…]
интернет по адресу москва
domashij-internet-msk002.ru
подключить интернет
провайдеры интернета в москве по адресу
domashij-internet-msk003.ru
тарифы интернет и телевидение москва
интернет провайдеры по адресу дома
domashij-internet-nizhnij-novgorod001.ru
подключить интернет по адресу
Lovely postings. Cheers!
Feel free to surf to my website … http://old.remain.co.kr/bbs/board.php?bo_table=free&wr_id=4048595
провайдеры в нижнем новгороде по адресу проверить
domashij-internet-nizhnij-novgorod002.ru
подключить интернет по адресу
Korina Kova Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
xx Reeses Pieces Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет провайдеры нижний новгород по адресу
domashij-internet-nizhnij-novgorod003.ru
узнать провайдера по адресу нижний новгород
Good information. Lucky me I came across your blog by accident (stumbleupon). I’ve bookmarked it for later!
Very good post. I’m going through some of these issues as well..
Mara Santiago Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Howdy! This article couldn’t be written much better! Reading through this article reminds me of my previous roommate! He always kept preaching about this. I’ll forward this information to him. Fairly certain he’s going to have a great read. I appreciate you for sharing!
Oh my goodness! Awesome article dude! Thank you so much, However I am experiencing issues with your RSS. I don’t understand why I can’t join it. Is there anybody getting the same RSS problems? Anyone that knows the solution can you kindly respond? Thanx!!
подключение интернета новосибирск
domashij-internet-novosibirsk001.ru
интернет по адресу дома
With thanks, Numerous data.
Feel free to surf to my page; http://new.jesusaction.org/bbs/board.php?bo_table=free&wr_id=6417574
Many thanks. Helpful stuff!
Also visit my blog … http://Itoxi.Co.kr/bbs/board.php?bo_table=free&wr_id=1931688
интернет тарифы новосибирск
domashij-internet-novosibirsk002.ru
домашний интернет тарифы
EssEss Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Awesome data, Cheers!
Here is my homepage: http://olangodito.com/bbs/board.php?bo_table=free&wr_id=4155674
SlimAssTink – SlimGoesRounds Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Though the regulation dates again to the 18th century, it has been employed regularly in trendy occasions. A 1948 Supreme Courtroom case, Ludecke v. Watkins, interpreted presidential authority underneath the legislation very broadly, holding that it precluded judicial evaluate of the removals. Trump was relying on the Alien Enemies Act of 1798, a venerable statute that permits the president to order the deportation of “alien enemies” in times of warfare, invasion, incursion or menace thereof.
But that’s far from the only cause we use it; you can see multiple benefits of a Trenbolone cycle. Trenbolone promotes the same features in the body for muscle and energy features and other positive effects in the identical method most anabolic steroids do. Before using Trenbolone, it’s crucial to consult a healthcare skilled. A physician or healthcare supplier may help you understand the potential dangers and side effects of Trenbolone use, in addition to provide guidance on dosages and cycles. Additionally, they can monitor your health and intervene if any adverse side effects arise. Trenbolone is a synthetic anabolic-androgenic steroid that’s derived from testosterone.
However, it is value remembering that steroids normally only speed up hair loss, so if you’re not predisposed to baldness, this drawback will most likely not affect you. Due to the longer half-life the injections can be made 2-3 occasions a week. The androgenic activity of Trenbolone can result in hair loss on the pinnacle however elevated hair growth on the face and physique.
Girls may also turn out to be more “masculine” whereas using trenbolone, experiencing unwanted effects such as deepening of the voice and facial hair development. Additionally, not like “T,” trenbolone doesn’t convert to estrogen within the body and generally doesn’t cause estrogen-like results. Many tren steroid users expertise a violent coughing fit generally recognized as “tren cough” throughout or shortly after injecting the compound. Therefore, it’s sensible to be cautious about tren’s results on the liver till additional research supplies clearer insights.
Go direct from metropolis centre to city centre, or hop on board an oblique prepare and change at Brussels-Midi/Zuid. Both means, we’ll get you there feeling rested, relaxed, and ready for work or play. You can nonetheless travel all the way to Amsterdam with us, but you may want to change trains in Brussels-Midi/Zuid. They may also be capable of be purchased on the Maya Train web site and in individual at each of the practice stations once the project is fully full. Now that the moment we’ve all been ready for has arrived, and tourists can journey almost the complete Yucatan Peninsula aboard the Maya Train, it’s time to get into the details. Yes, you can attain Machu Picchu by climbing the Inca Path or by way of the route by way of Santa Teresa. Nevertheless, touring by practice is the most popular and handy for many tourists.
Topical pores and skin merchandise or oral antibiotics, as suggested by a well being care provider, can go a way in mitigating this problem. Those inclined to severe pimples when utilizing Tren won’t doubtless see much reduction from over-the-counter pimples treatments. One Other grievance you might encounter, mainly limited to guys utilizing Tren for slicing or recomposition, is that the increased urge for food turns into a problem.
You can’t buy tickets on-line, however only at the ticket window or one of the newspaper stands within the station. The Circumvesuviana station is on the decrease stage of the Naples Centrale practice station, under the excessive velocity practice platforms. Sounds weird but apparently Tren will fucks with your glycogen levels and tends to rob your liver of glycogen which does lots of work while you sleep. Your liver can solely maintain about 100grams of the stuff so it doesn’t have a lot to spare like all of your muscles. Maple syrup or Honey proper earlier than mattress helps give the liver the sugar it needs to get some glycogen going. This article is part of an entire tutorial about practice journey from Madrid where you’ll find a way to read all the knowledge you should organize your train journeys from the town. Atocha practice station is situated in one of the primary avenues of the city middle so it’s fairly simple to seek out it.
Genetics, food regimen, way of life, workouts, and cycle protocol will all affect a person’s trenbolone results. The Circumvesuviana trains are often late and overcrowded, with no place to take a seat, no air con, and no luggage storage. Pickpocketing and different non-violent theft is frequent.For a means more snug and safe possibility, e-book a non-public transfer from Naples to Sorrento. The main Piazza Garibaldi (Naples Centrale) station isn’t accessible as there are no ramps to the decrease degree. DD trains do not stop at all the stations, so attain Sorrento in about 50 minutes.
Your tolerance ranges will determine one of the best dosage for your needs, as will the inclusion of different compounds in your cycle. First-time users ought to start with a low dose of this very powerful steroid. But more advanced customers may take the dosage to over 400mg weekly – this is not beneficial for beginners and comes with significantly larger dangers of unwanted effects. It enhances purple blood cell manufacturing, leading to improved oxygenation and nutrient supply to muscle tissue. This interprets into increased endurance, stamina, and general athletic efficiency. Moreover, Trenbolone aids in post-workout recovery, reducing muscle fatigue and enhancing the body’s capability to repair and rebuild after intense training periods. Moreover, Trenbolone has the ability to increase pink blood cell production, which improves oxygen delivery to the muscular tissues and enhances endurance and performance.
Thankfully, this particular aspect effect is definitely prevented because it comes about as a result of your Tren dose being too high and not enough exogenous testosterone being provided to satisfy your needs. It’s merely essential that you include a type of testosterone in your Trenbolone, which, at the very least, must be at a hormone alternative dosage. Still, countless Tren users do, and it could possibly vary from mild to moderate incapability to fall or stay asleep, right as much as extreme insomnia where you’re barely getting any sleep at all. In the worst instances, some guys will turn to drugs or different sleeping aids to deal with this concern because if you’re not sleeping nicely, your results and performance are in jeopardy. Incidences of elevated sweating are reported rather more often with Trenbolone than with different steroids. The most probably cause for the extreme perspiration is the raised metabolic price that Tren causes.
Often called “Tren rage,” it is believed that individuals who already have an aggressive nature before using Tren are much extra likely to turn out to be worse while on it. The main purpose for so-called Tren-rage is the effect the androgenic compounds have on brain chemistry, inflicting irritability and a short fuse in some guys. Suppose you’re buying a Trenbolone product already blended into an oil solution ready for injection (rather than buying the raw veterinary pellets yourself). In that case, you’ll sometimes purchase 10 ml vials at 100mg/ml, which can cost wherever from $50 to $100. As A Result Of it’s manufactured specifically for livestock use, Tren Ace is bought as pellets. For use in people, labs or people will create an injectable type in an oil-based resolution.
References:
risks of using anabolic steroids and other performance-enhancing drugs (https://images.google.as/url?q=https://jbhnews.com/tren-trenbolone-acetate-steroid-for-bodybuilding/24831/)
подключение интернета новосибирск
domashij-internet-novosibirsk003.ru
провайдеры интернета в новосибирске
дешевый интернет санкт-петербург
domashij-internet-spb001.ru
подключить интернет тарифы санкт-петербург
Jae x Galore – BrattyJaeX Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
ThicckAsia – Thick Lauryn Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
провайдеры интернета санкт-петербург
domashij-internet-spb002.ru
провайдер по адресу санкт-петербург
Janie Fit Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
провайдеры интернета в санкт-петербурге по адресу
domashij-internet-spb003.ru
провайдеры интернета в санкт-петербурге по адресу проверить
Paola Rosalina Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Kim Lifts Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
I’ve had some lucky streaks on Tiger Fortune lately. fortune tiger demo
rent a yacht in cancun
[…]very couple of web sites that happen to be comprehensive beneath, from our point of view are undoubtedly very well worth checking out[…]
Sammyyk VIP Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
french bull
[…]Here is a good Weblog You may Come across Fascinating that we Encourage You[…]
CuteFruit Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Erzabel X Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Nadia Palik Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Curvy Mommy Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
It is indeed my belief that mesothelioma will be the most lethal cancer. It has unusual qualities. The more I really look at it the greater I am certain it does not work like a true solid flesh cancer. When mesothelioma is really a rogue viral infection, therefore there is the chance of developing a vaccine plus offering vaccination to asbestos open people who are at high risk of developing long run asbestos related malignancies. Thanks for sharing your ideas on this important ailment.
coco chanel dog collar
[…]Here are a number of the websites we advise for our visitors[…]
Thank you for this article. I would also like to convey that it can often be hard when you are in school and merely starting out to initiate a long credit standing. There are many college students who are merely trying to live and have an extended or positive credit history are often a difficult thing to have.
chanel dog bowls
[…]the time to study or pay a visit to the content material or sites we have linked to beneath the[…]
Jolene Canada Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Zuribella Rose Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Shiroktsne FANSLY Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
VivaLaKipp Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Fine Ass Mercedes Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Ambar Reyess Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
gaming
[…]we came across a cool web-site that you just may well love. Take a search if you want[…]
Gina Savage X Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Many thanks. I like it.
Have a look at my page … https://www.hb9lc.org/wiki/index.php/Analyse_De_Propri%C3%83_t%C3%83_Commerciale_:_Comment_%C3%83_valuer_Un_Bien_Immobilier_Pour_Un_Financement_Rentable
домашний интернет тарифы челябинск
domashij-internet-chelyabinsk001.ru
домашний интернет подключить челябинск
Sophie Raiin Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
RissaCute Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет провайдер челябинск
domashij-internet-chelyabinsk002.ru
подключить интернет в квартиру челябинск
Jae x Galore – BrattyJaeX Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Ny Ny Irene Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
дешевый интернет челябинск
domashij-internet-chelyabinsk003.ru
интернет тарифы челябинск
crypto news
[…]Every when inside a while we pick out blogs that we study. Listed below are the most current web pages that we choose […]
I Am Queen Jaii FANSLY Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
какие провайдеры интернета есть по адресу красноярск
domashij-internet-krasnoyarsk001.ru
провайдеры по адресу
KoKo Kay Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Ms Biddies Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
bjj houston tx
[…]just beneath, are quite a few absolutely not connected internet sites to ours, having said that, they may be certainly really worth going over[…]
провайдер интернета по адресу красноярск
domashij-internet-krasnoyarsk002.ru
подключить интернет по адресу
That Honey Dip Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Gabrielle The Goddesss Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Wow quite a lot of wonderful material.
Feel free to surf to my page – http://Www.itoxi.co.kr/bbs/board.php?bo_table=free&wr_id=1801971
Often, Anavar will flush out extracellular water and shuttle fluid inside the muscle. When an individual stops taking Anavar, they won’t look as dry, and their muscle tissue won’t be as full. However, this solely has a gentle impact on a person’s overall look. At Present, gymgoers should purchase Anavar on the black market because of the difficulty of getting a doctor to prescribe it for something aside from a muscle-wasting sickness. The 60 minutes prior to your workout is taken into account the optimum window for getting the most out of your Anavar dose. This offers the Anavar enough time to kick in before you start your heat up and training. Anavar, also called Oxandrolone, has a half-life of 8-12 hours when taken orally.
Anavar is a by-product of dihydrotestosterone; thus, there is no conversion to DHT by way of the 5-alpha reductase enzyme. Consequently, Anavar has delicate androgenic properties and unwanted aspect effects. Analysis exhibits that 20 mg of oxandrolone causes 72% much less sulfobromophthalein, a marker of liver stress, in comparison with an equal dose of fluoxymesterone (10). Based on our tests, Anavar is certainly one of the best steroids in regard to toxic unwanted effects. Analysis has also proven it to own safety in long-term medical settings (9). I needed to enhance my athletic efficiency and lose some fat without losing any muscle that I had worked exhausting for. There isn’t a lot difference in Anavar dosage for bodybuilding purposes whether or not you’re a man or lady.
The good news about Clenbuterol is that it’s not a hormonal compound and does not affect your testosterone manufacturing. However, suppose you (as a male) intend to stack Clen with any anabolic steroid or suppressive SARM. In that case, you’ll need to do some form of applicable post-cycle remedy relevant to the opposite PEDs being used. This cycle is for these already at a relatively low physique fat degree (average weight or below). 15lbs of weight loss is feasible, depending on your meals intake and exercise routine.
By nutrient partitioning, Clen can stop fat from being stored, encourage the utilization of fats for power, and stop the usage of lean muscle. Certain medical results and opposed reactions demonstrate the androgenic properties of this class of drugs. Full dissociation of anabolic and androgenic results has not been achieved. The actions of anabolic steroids are subsequently much like these of male sex hormones with the potential of causing severe disturbances of growth and sexual improvement if given to young kids. Anabolic steroids suppress the gonadotropic capabilities of the pituitary and will exert a direct impact upon the testes. Anavar has gained popularity among feminine bodybuilders and athletes as a result of its ability to pack in muscle without the accompanying gains in body fats, and it is also very minimally toxic. Whereas it provides wonderful outcomes, its possible risks cannot be taken flippantly either.
One of the first advantages of Oxandrolone is its ability to promote lean muscle mass positive aspects. It works by rising protein synthesis, which ends up in the development of quality muscle tissue. In Distinction To another steroids, it is much less likely to cause water retention or extreme weight achieve, making it a perfect choice for those in search of a lean and sculpted physique. One Other notable advantage of Anavar is its potential to enhance energy and power.
Intermediate customers might be on the stage the place you’re comfortable stacking Clen with at least one other compound. Nonetheless, the general goal might be a slicing cycle the place quick and highly effective fats loss is a precedence, as is retaining lean muscle and reaching a toned and ripped physique. Muscle loss and fats are at all times risks during a calorie-deficit phase or cutting cycle. Anavar will help preserve lean muscle mass while promoting fats loss in order that the muscle features one has made during bulking are retained. This factor is very important for ladies to retain their hard-earned muscles while dropping extra fat.
One of the explanations Clenbuterol isn’t accredited to be used in the USA is its potential to cause everlasting organ damage. Research have discovered that a very high share of Clenbuterol users who experienced extreme side effects ended up having to be admitted to hospital. Ongoing insomnia14 can also turn into a longer-term side effect of Clen. Lack of sleep will impression your results negatively and make it tougher for you to get well from intensive workouts. The proven reality that Clenbuterol is a stimulant means you’ll be able to anticipate a spread of unwanted effects that may influence each particular person to a special extent. Some customers of Clen shall be significantly extra delicate to stimulant-caused side effects, while others will have a higher level of tolerance. You won’t know what adverse effects you’ll find a way to expect from Clenbuterol till you’ve used it.
Your doctor may monitor your blood calcium level to forestall problems. Bear In Mind that this medication has been prescribed as a outcome of your physician has judged that the profit to you is larger than the danger of unwanted effects. When it comes to combining Anavar with other substances, warning is suggested. Anavar is known to be a relatively gentle steroid with low potential for unwanted facet effects, but it can still be harmful when used irresponsibly or in combination with certain substances. Be positive to additionally read my private experiences with an Anavar solely cycle. I’ve tried one two occasions and within the referenced publish I am happy to share how they labored out for me.
Such myths turn out to be a reality with a trenbolone/Winstrol cycle, the place a user’s waist measurement decreases and muscle dimension will increase concurrently. Our sufferers have reported fast fats loss while additionally constructing noticeable amounts of muscle and strength on trenbolone/Winstrol cycles. Anavar will also trigger elevations in liver enzymes, marking a level of hepatic stress. Thus, it’s crucial for users with compromised livers to keep away from Anavar and other oral anabolic steroids. If a person requires Anavar for cachexia however has compromised hepatic function, then injectable anabolic steroids could additionally be extra optimum.
Women can expect wonderful outcomes from an Anavar cycle, together with beautiful energy positive aspects. You’ll be lifting heavier weights and may find your lifting action improves with that strength boost. You should not expect important muscle features – Anavar just isn’t a bulking steroid, but it can promote some lean gains whereas concurrently losing fat. Ladies can achieve in the 10lbs range, whereas men tend to see smaller gains under 10lbs.
References:
are testosterone pills steroids (https://sigorta.jobs/employer/anavar-test-cycle/)
Toveyah Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
проверить интернет по адресу
domashij-internet-krasnoyarsk003.ru
провайдеры интернета по адресу
french bulldog
[…]we prefer to honor numerous other world wide web web sites around the net, even though they aren稚 linked to us, by linking to them. Below are some webpages really worth checking out[…]
bjj jiu jitsu cypress texas
[…]although web sites we backlink to beneath are considerably not connected to ours, we really feel they may be actually worth a go as a result of, so have a look[…]
провайдер по адресу краснодар
domashij-internet-krasnodar001.ru
интернет по адресу дома
Anelisa Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
5cf66f3
Best SEO system for franchise businesses
узнать интернет по адресу
domashij-internet-krasnodar002.ru
подключить интернет по адресу
The Real Touch XX Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
bjj jiu jitsu magnolia texas
[…]check below, are some entirely unrelated internet sites to ours, however, they are most trustworthy sources that we use[…]
You said it perfectly..
Feel free to surf to my site http://Www.infoanda.com/viewcomments.php?li=Sm.co.kr%2Fbbs%2Fboard.php%3Fbo_table%3Dfree%26wr_id%3D1656936
ur Fav Kittty Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
CuteFruit Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Awesome information, Thanks a lot!
My webpage – http://Onestopclean.kr/bbs/board.php?bo_table=free&wr_id=1193085
провайдеры по адресу краснодар
domashij-internet-krasnodar003.ru
узнать провайдера по адресу краснодар
mexican candy bags
[…]Wonderful story, reckoned we could combine a couple of unrelated information, nevertheless definitely worth taking a appear, whoa did a single understand about Mid East has got extra problerms as well […]
Lillianette Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет по адресу
domashij-internet-samara001.ru
провайдеры интернета по адресу
подключение интернета по адресу
domashij-internet-samara002.ru
провайдеры в самаре по адресу проверить
Ny Ny Irene Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет провайдеры по адресу дома
domashij-internet-samara003.ru
провайдер по адресу
Thanks for the suggestions about credit repair on this site. The things i would advice people is to give up this mentality that they buy at this moment and pay later. As being a society all of us tend to do that for many things. This includes vacations, furniture, and also items we want. However, you’ll want to separate a person’s wants from the needs. While you are working to raise your credit ranking score you really have to make some sacrifices. For example you can shop online to save money or you can click on second hand outlets instead of pricey department stores regarding clothing.
Howdy! Would you mind if I share your blog with my myspace group? There’s a lot of people that I think would really enjoy your content. Please let me know. Many thanks
интернет провайдеры по адресу дома
domashij-internet-ufa001.ru
провайдеры по адресу дома
Baddiee Babe Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Sophie Raiin Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить интернет по адресу
domashij-internet-ufa002.ru
интернет по адресу
Kara J Lee Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
I hit a hot streak on online blackjack—lucky day! dragon hatch
Tiahnie Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет по адресу
domashij-internet-ufa003.ru
провайдеры интернета в уфе по адресу проверить
Gabrielle The Goddesss Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
дешевый интернет челябинск
domashij-internet-chelyabinsk001.ru
подключить интернет
Bebe Da Brattttt Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
View this post on Instagram https://sellerweb.ru/product/adapter-bluetooth-5-3-type-c/
интернет провайдер челябинск
domashij-internet-chelyabinsk002.ru
подключить проводной интернет челябинск
I was just searching for this info for a while. After six hours of continuous Googleing, finally I got it in your website. I wonder what is the lack of Google strategy that do not rank this type of informative websites in top of the list. Generally the top websites are full of garbage.
I want to to thank you for this great read!! I absolutely loved every little bit of it. I have got you bookmarked to look at new things you post…
This article is a breath of fresh air! The author’s distinctive perspective and insightful analysis have made this a truly fascinating read. I’m grateful for the effort she has put into creating such an educational and thought-provoking piece. Thank you, author, for providing your knowledge and stimulating meaningful discussions through your brilliant writing!
интернет провайдер челябинск
domashij-internet-chelyabinsk003.ru
лучший интернет провайдер челябинск
Nicely put. Thank you!
Feel free to surf to my webpage; http://Maps.Google.ca/url?sa=t&url=http%3A%2F%2F365.Expresso.blog%2Fquestion%2Fagence-immobiliere-sur-le-quebec-votre-informations-pour-atteindre-dans-limmobilier-3%2F
Howdy! This blog post could not be written any better! Reading through this article reminds me of my previous roommate! He continually kept talking about this. I am going to send this article to him. Pretty sure he’ll have a very good read. Many thanks for sharing!
интернет провайдеры красноярск по адресу
domashij-internet-krasnoyarsk001.ru
какие провайдеры интернета есть по адресу красноярск
Howdy would you mind stating which blog platform you’re working with? I’m looking to start my own blog soon but I’m having a tough time deciding between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design seems different then most blogs and I’m looking for something unique. P.S Apologies for being off-topic but I had to ask!
Brown Bodii Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
This page truly has all of the info I needed about this subject and didn’t know who to ask.
We have found that valerian root dietary supplements could additionally be efficient for mild insomnia, decreasing the time taken to go to sleep and the quality of sleep (36, 37). In one study, participants reached sleep 36% faster after a single dose of valerian (38). Clenbuterol’s fat-burning results may be attributed to its highly effective effects on the central nervous system (CNS).
Women taking high doses are vulnerable to a big selection of unwanted aspect effects, among those is virilization. Girls can see important improvements in the above parameters depending on a number of factors like diet, way of life, exercise time, and intensity, not to forget, the genetic elements. You will proceed to see additional improvements until the completion of the 6-week cycle. This article gives perception into varied aspects of Anavar for ladies like what precisely is it, its benefits, dosage, risks, what is natural Anavar for girls, and rather more. Intervals can turn into late on Anavar (even on low doses), because the steroid interferes with the natural manufacturing of estrogen/progesterone. The reverse can even occur, with steroids being able to causing early menstruation in girls (9).
Analyze your progress knowledge and assess whether or not modifications to your training or vitamin plan are warranted. Based in your goals and individual response, you can contemplate growing the intensity of your exercises, adjusting caloric intake, or fine-tuning macronutrient ratios. Oxandrolone is renowned for its capability to contribute to varied health targets, including muscle definition, power enchancment, enhanced endurance, and fat loss. This desk provides a comparison of Anavar’s results on these key features, supplying you with an overview of the potential benefits it presents. Please notice that individual outcomes may range, and it is crucial to make use of Anavar responsibly and underneath professional guidance.
Whereas Anavar could assist in your bodybuilding journey, the road to a sculpted physique still primarily depends on devoted training, solid nutrition, and sufficient rest. Don’t rush the method, and ensure any changes to your dosage are thoughtfully thought of. When it comes to the usage of Oxandrolone, generally known as Anavar, understanding the appropriate dosage is important, and it could possibly differ based on gender. Each men and women seek the advantages of Anavar for enhancing their physique and efficiency, however the dosage requirements can vary significantly. In the table below, we present a comparison of really helpful Anavar dosages for women and men. Some girls could expertise noticeable side effects even at low doses, while others may tolerate greater doses with minimal issues.
Sure, Anavar can have an result on your interval by causing irregularities because of its influence on hormone ranges. People who wish to acquire Anavar should consider purchasing from reputable sources for authentication and high quality. The finest place to buy Anavar is thru the CrazyBulk official web site, as that may make certain the legality and security of this merchandise.
Extra blood or RBCs means extra oxygen which provides you higher muscle energy and endurance. Branched-chain amino acids are a combination of three important amino acids that include Valine, leucine, and isoleucine. BCAA’s are often taken to extend muscle development and boost exercise performance.
However that’s just one aspect of the story… Performance doses take things to a brand new stage as a outcome of we need to profit from Anavar’s anabolic effects beyond what’s required in medical remedies. As a remedy for anemia, Anavar has a very helpful effect on pink blood cell count21, bringing about heightened endurance by transporting extra oxygen and vitamins to the muscle tissue throughout exercise. This has a performance-enhancing and bodily appealing effect, with more oxygen and blood being carried via the veins, resulting in enhanced vascularity.
Ideally, you’ll need to already be around 15% body fats before using Anavar. Males on a cutting cycle with Anavar can anticipate a superb fat loss, and it goes to be quite quick because Anavar is a quick-acting steroid that you’ll solely use for eight weeks max. Using Anavar at low to reasonable doses is about as secure as it could get for anabolic steroid use. But abuse Anavar beyond the really helpful usage patterns, and also you do set yourself up for an unsafe steroid experience that can and will damage your health. The hardness and dryness of Anavar features and fats loss are amongst its strongest and most desirable advantages.
The higher your dose of Anavar, the more severe your testosterone suppression is more doubtless to be. It can take a quantity of months for your testosterone to get well its normal operate after finishing an Anavar cycle. Waiting for this to naturally occur is not an possibility because low testosterone is seriously debilitating. Symptoms can be widespread and severe and can include fatigue, despair, low libido, loss of muscle, and fats acquire, to call only a few. Facet effects caused by rising estrogen levels come about when a steroid causes the conversion of testosterone into estrogen (also referred to as aromatization). One of the most appealing issues about Anavar is that it does NOT aromatize and, therefore, does not cause estrogenic unwanted aspect effects.
Some potential unwanted side effects of Anavar in aged individuals may include liver strain, hormonal imbalances, and temper modifications. One Other thing is that Primobolan’s unwanted facet effects are very minimal, particularly if in comparison with different steroids that women (and men) use. The most essential thing to recollect is that steroid unwanted facet effects and their severity are going to be primarily based on the dose and size of the cycle.
Inexperienced users will share their unfavorable Anavar experiences, but so usually, this revolves round the truth that a person didn’t use a testosterone base when on an Anavar cycle! If Anavar is the primary steroid you wish to use, you’re nonetheless almost certainly going to stack it with no less than a form of testosterone as a testosterone alternative during your cycle. One of the much less spoken-about advantages of Anavar is a possible increase to your general mood. The identical can’t be mentioned for lots of different steroids, which can probably cause nervousness and elevated anger instead.
Therapeutic and medical research doses are typically 20mcg to 40mcg per day. Not Like steroids, where there is normally a vast distinction between female and male beneficial dosages, Clenbuterol permits each to make use of very comparable doses. Because females are, on common, smaller in body measurement and weight than males, the dose must be tailor-made accordingly. Otherwise, the response to Clenbuterol is very much the identical with each sexes.
References:
https://djtime.ru/latashiawhitak
I have observed that in the world today, video games would be the latest rage with children of all ages. Many times it may be extremely hard to drag young kids away from the video games. If you want the very best of both worlds, there are lots of educational video games for kids. Good post.
It’s perfect time to make some plans for the future and it’s time to be happy. I’ve read this post and if I could I wish to suggest you some interesting things or tips. Perhaps you can write next articles referring to this article. I wish to read even more things about it!
провайдеры интернета по адресу
domashij-internet-krasnoyarsk002.ru
интернет провайдеры в красноярске по адресу дома
Sexxy Jaimie Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет по адресу красноярск
domashij-internet-krasnoyarsk003.ru
какие провайдеры интернета есть по адресу красноярск
Queenn Cuban xXx – Cuban Chicc X Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
You actually make it seem so easy with your presentation however I in finding this matter to be actually something that I believe I’d by no means understand. It seems too complicated and very large for me. I am having a look ahead to your next put up, I’ll try to get the dangle of it!
Gabriella_ Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Thanks for expressing your ideas right here. The other point is that whenever a problem develops with a personal computer motherboard, individuals should not take the risk regarding repairing it themselves for if it is not done right it can lead to irreparable damage to an entire laptop. It is almost always safe just to approach a dealer of a laptop for that repair of its motherboard. They will have technicians who may have an competence in dealing with laptop computer motherboard issues and can get the right analysis and carry out repairs.
проверить провайдеров по адресу краснодар
domashij-internet-krasnodar001.ru
интернет по адресу дома
We are a group of volunteers and starting a new scheme in our community. Your web site provided us with valuable information to work on. You’ve done an impressive job and our whole community will be grateful to you.
You made some decent factors there. I seemed on the web for the difficulty and found most individuals will associate with along with your website.
интернет провайдеры по адресу
domashij-internet-krasnodar002.ru
проверить провайдера по адресу
Breckie Hill Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Nikki Stone Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Livv A Little Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
TylerUncensored Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
May I just say what a comfort to find somebody who genuinely knows what they’re discussing on the internet. You actually realize how to bring an issue to light and make it important. More people should check this out and understand this side of the story. I was surprised you’re not more popular since you surely have the gift.
провайдер по адресу краснодар
domashij-internet-krasnodar003.ru
интернет по адресу краснодар
Can I simply say what a reduction to seek out somebody who truly knows what theyre talking about on the internet. You undoubtedly know how you can bring an issue to mild and make it important. More individuals need to learn this and perceive this aspect of the story. I cant consider youre no more in style because you undoubtedly have the gift.
There are some interesting closing dates on this article but I don?t know if I see all of them middle to heart. There’s some validity but I will take hold opinion till I look into it further. Good article , thanks and we would like extra! Added to FeedBurner as nicely
Nicely put, Cheers.
Also visit my homepage :: http://ww17.spiritlines.com/__media__/js/netsoltrademark.php?d=thebestgamesites.Awardspace.info%2Findex.php%3Fa%3Dstats%26u%3Drafaeladoughty
проверить интернет по адресу
domashij-internet-samara001.ru
проверить провайдеров по адресу самара
Earthiangel Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
провайдеры интернета в самаре по адресу
domashij-internet-samara002.ru
проверить провайдера по адресу
I have been absent for a while, but now I remember why I used to love this blog. Thank you, I will try and check back more often. How frequently you update your website?
Missus Blu Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
I’m not that much of a online reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back later on. All the best
Gabrielle The Goddesss Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключение интернета по адресу
domashij-internet-samara003.ru
интернет провайдеры по адресу
Pretty section of content. I simply stumbled upon your web site and in accession capital to say that I get actually loved account your weblog posts. Any way I will be subscribing for your augment or even I achievement you access consistently rapidly.
узнать интернет по адресу
domashij-internet-ufa001.ru
какие провайдеры по адресу
Nasty GILF – YoFavShyFreak – Taveleigh Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Juicy Lips Goddess Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Good posts, Kudos!
my web blog; https://tangguifang.Dreamhosters.com/comment/html/?1334112.html
провайдер интернета по адресу уфа
domashij-internet-ufa002.ru
провайдеры в уфе по адресу проверить
Kayla G Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
70918248
References:
https://pandittechnologies.com/employer/anavar-resultados-de-p%C3%A9rdida-de-peso
Paola Rosalina Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет провайдеры по адресу дома
domashij-internet-ufa003.ru
какие провайдеры на адресе в уфе
Saab Silvi Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Hello! I know this is kind of off topic but I was wondering which blog platform are you using for this site? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be great if you could point me in the direction of a good platform.
Coco Fantasia Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
wix seo
[…]we like to honor many other world-wide-web web pages around the internet, even when they aren稚 linked to us, by linking to them. Under are some webpages worth checking out[…]
Nicole Aniston XO Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
minnect expert
[…]below you will find the link to some internet sites that we think you must visit[…]
Juliana x Ferrara Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
french pitbull
[…]Here is a great Weblog You might Come across Intriguing that we Encourage You[…]
boston terrier french bulldog mix
[…]although sites we backlink to beneath are considerably not connected to ours, we really feel they’re basically really worth a go by means of, so have a look[…]
Paola Rosalina Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
The Juicy Goddess Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Karla James Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
floodle
[…]check beneath, are some totally unrelated websites to ours, nonetheless, they’re most trustworthy sources that we use[…]
Jay The Creatorr Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Paola Rosalina Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Today, considering the fast life-style that everyone is having, credit cards have a big demand throughout the market. Persons coming from every area of life are using credit card and people who are not using the card have prepared to apply for just one. Thanks for revealing your ideas on credit cards.
Saab Silvi Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Princess So Seductive Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Amira X Evans Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить интернет
domashij-internet-omsk001.ru
интернет провайдер омск
Mikayla D VIP – Mikayla Demaiter Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Haleigh Cox Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Thank you! An abundance of write ups!
My blog https://Ykentech.com/bbs/board.php?bo_table=free&wr_id=2939247
домашний интернет
domashij-internet-omsk002.ru
подключить интернет в омске в квартире
uDream of Jordan VIP Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить домашний интернет в омске
domashij-internet-omsk003.ru
интернет провайдеры омск
домашний интернет тарифы пермь
domashij-internet-perm001.ru
подключить интернет
Lolita Aliya – u Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Shy Thickie VIP Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Hey, I think your website might be having browser compatibility issues. When I look at your website in Opera, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, excellent blog!
Thanks for these pointers. One thing I additionally believe is the fact that credit cards providing a 0 rate of interest often lure consumers with zero rate, instant approval and easy on the web balance transfers, however beware of the top factor that will void your own 0 easy road annual percentage rate and throw one out into the terrible house quickly.
подключить проводной интернет пермь
domashij-internet-perm002.ru
подключить интернет пермь
провайдеры интернета в перми
domashij-internet-perm003.ru
интернет тарифы пермь
Baddiee Babe Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Haleigh Cox Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
тарифы интернет и телевидение ростов
domashij-internet-rostov001.ru
лучший интернет провайдер ростов
Kendra Karter Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Cubana Redd Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
провайдеры интернета в ростове
domashij-internet-rostov002.ru
подключить домашний интернет в ростове
TylerUncensored Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
TylerUncensored Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
K Zaye Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет домашний ростов
domashij-internet-rostov003.ru
домашний интернет
подключить домашний интернет в волгограде
domashij-internet-volgograd001.ru
домашний интернет тарифы омск
Ivory Offical Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить домашний интернет в волгограде
domashij-internet-volgograd002.ru
подключить интернет в волгограде в квартире
подключить интернет тарифы омск
domashij-internet-volgograd003.ru
подключение интернета омск
Really quite a lot of valuable tips.
Also visit my web page: http://Webhesive.com/__media__/js/netsoltrademark.php?d=Simple01.Netpro.Co.kr%3A443%2Fbbs%2Fboard.php%3Fbo_table%3Dfree%26wr_id%3D263
I can’t believe how amazing this article is! The author has done a phenomenal job of delivering the information in an compelling and enlightening manner. I can’t thank him enough for providing such priceless insights that have undoubtedly enlightened my understanding in this topic. Kudos to him for crafting such a masterpiece!
Anavar is a sort of oral steroids that I knew I’d be fairly comfortable taking again after I started all this. Tanveer Quraishi, writer of Steroids 101 has in depth expertise within the subject of bodybuilding and has been writing online on varied muscle-building and other health subjects for a couple of years now. He is not just interested in bodybuilding but is a superb football player too. When he is not writing for his website or coaching at the health club, he loves to spend his time with this spouse and kids.
All steroids include some negatives, but Anavar is on the lower end of the size when it comes to unwanted effects and risks. Most of those will solely be of concern if you’re utilizing doses which would possibly be too high or utilizing the drug for longer than recommended durations. Anavar is especially good at eliminating fats in additional cussed areas, and for women, that is normally around the thighs and buttocks. Although overall body weight may not drop or change much, this is as a end result of of muscle achieve – fats continues to be being lost. On a proper diet, girls can expect to lose 5-10lbs of fat on an Anavar cycle unless they are lean. It is feasible to lose 5% of body fat when doing a simple Anavar and testosterone cycle. If you’re already at 10% physique fats or less, 5% could be a really extreme result.
Nitrogen is a key component of protein, which is crucial for muscle development. By rising nitrogen retention, Anavar helps to ensure that your muscles have all of the vitamins they should grow larger and stronger. You don’t have to worry about such issues as water retention or gyno whenever you take this steroid, both.
Whereas Anavar is toxic to the liver5, as we would expect with an oral steroid, its hepatotoxicity level is minimal compared with many other steroids, making this a perfect choice for newbies. Anavar is a fast-acting steroid derived from DHT (dihydrotestosterone)4 with a half-life of eight to 10 hours. It has been a widely used, respected, and very fashionable steroid for a protracted time and is likely one of the few that females can also use because of its gentle androgenic effects.
In our expertise, the one steroid that is the identical as Anadrol, when it comes to anabolism and rising weight acquire, is Dianabol. Combining 5 of our strongest muscle constructing and fats burning formulas for superb, fast-acting outcomes. D-Bal’s highly effective formulation mimics the results of Methandrostenolone, otherwise known as Dianabol, the granddaddy of steroids.
As a consequence of a rise in progesterone, a hormone that is similar to estrogen, Deca Durabolin has the potential to cause gynecomastia. Thus, we typically monitor patients’ nipples during this stack, and if they begin to become swollen or breast tissue enlarges, then we administer an AI to prevent additional hypertrophy. Furthermore, Dianabol increasing water retention has a detrimental impression on blood stress, necessitating the heart to exert extra effort than traditional to circulate blood throughout the physique. Further blood viscosity, attributable to greater volumes of H2O, is the reason for this. We will examine essentially the most prevalent Dianabol stacks used by bodybuilders from the Golden Era to the current day.
I uploaded the video the place he recommends anavar here, since it isn’t public. This recovery process is more probably to take place in 30 days or less when using an efficient PCT (post-cycle therapy). Nevertheless, it must be famous that Turinabol’s and Anavar’s anabolic attributes outweigh their capability to induce fat loss. If you’re bulking and intend to gain most quality mass, you might think about stacking Tren with Dianabol, Deca Durabolin, and Testosterone.
One of its best makes use of is initially of a cycle to kickstart your energy positive aspects shortly, followed up by slower-acting injectable steroids. Anadrol is not a perfect cutting steroid due to the amount of water retention it causes. This is the alternative of what you need in a cutting cycle, the place you aim to achieve a really outlined and vascular physique. Anadrol may be helpful between slicing cycles to put on mass but would rarely, if ever, be utilized in a devoted slicing cycle. It’s not just underdosing that you can run into both; some UGL consumers of Anadrol discover their tablets are overdosed by as much as 12mg per tablet.
This means Primo retains many of the properties and actions of DHT itself, namely that there is not any estrogen aromatization activity – eliminating the danger of water retention and gyno. Primo is usually used to control and balance estrogen levels when using aromatizing steroids. For novices, it is typically beneficial to begin with a day by day dosage ranging from 20-30mg. Commencing with a decrease dosage is essential, and if necessary, gradual increments ought to be considered to minimize potential undesirable outcomes. This cautious strategy permits for a better understanding of individual tolerance and response to the substance. When initiating your initial Oxandrolone cycle, sustaining a meticulous log documenting your progress, physical transformations, and any encountered undesirable results is advisable.
The drug Anavar is used so as to enhance the rate of protein synthesis in order that the muscle tissue can turn out to be stronger and might help perform physical train and other actions more simply. Keep In Mind to be attentive to any signs of virilization, corresponding to deepening of the voice or excessive hair development. Anavar can additionally be stacked with different compounds for enhanced results, however caution ought to be exercised to mitigate potential unwanted effects.
To decrease the prospect of unwanted effects, don’t combine medicine that work in the same method. If you are taking two medication that each act like DHT derivatives, it could increase the chance of hair loss and prostate issues. Using Anavar together with other compounds like testosterone can enhance cycle outcomes. It’s essential to be careful when stacking and speak to a healthcare skilled for personalized advice and supervision. Many customers choose it as a end result of it has few unwanted effects compared to different steroids.
References:
How Bad Are Steroids (https://ezojob.com/employer/official-web-site-mr-olympia-shop-steroids/)
провайдеры домашнего интернета воронеж
domashij-internet-voronezh001.ru
тарифы интернет и телевидение воронеж
FoxyBrown FANSLY Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Jolene Canada Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
провайдеры интернета в воронеже
domashij-internet-voronezh002.ru
домашний интернет тарифы
Bunz Ever Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
домашний интернет в воронеже
domashij-internet-voronezh003.ru
провайдеры интернета воронеж
Seriously loads of terrific data.
Here is my blog post :: http://Cqcici.com/comment/html/?433195.html
дешевый интернет омск
domashij-internet-omsk001.ru
подключить домашний интернет омск
домашний интернет тарифы омск
domashij-internet-omsk002.ru
интернет провайдер омск
You actually make it appear so easy with your presentation but I find this topic to be actually one thing that I think I’d never understand. It sort of feels too complex and very large for me. I’m looking ahead to your next put up, I will attempt to get the hold of it!
PrettyFaceSZN . – Naomi Nash Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
интернет провайдер омск
domashij-internet-omsk003.ru
домашний интернет омск
Yanni Da Goat Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Angelic Fuck Doll Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Sammyyk VIP Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Soriyah Sann Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить интернет тарифы пермь
domashij-internet-perm001.ru
подключение интернета пермь
Paris Senpai Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Badd Girl Riri Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить домашний интернет пермь
domashij-internet-perm002.ru
подключить интернет в перми в квартире
дешевый интернет пермь
domashij-internet-perm003.ru
тарифы интернет и телевидение пермь
Curvy Mommy Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
провайдеры интернета в ростове
domashij-internet-rostov001.ru
домашний интернет ростов
Anita Isabella Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Valuable info. Lucky me I found your site by accident, and I am shocked why this accident did not happened earlier! I bookmarked it.
подключить домашний интернет ростов
domashij-internet-rostov002.ru
домашний интернет ростов
Yasmin Estrada Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Cherri Cali Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить домашний интернет в ростове
domashij-internet-rostov003.ru
домашний интернет тарифы
Voulez J Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Kayla Dene Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Vinny Ballerina Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Jade x Jamal Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
недорогой интернет омск
domashij-internet-volgograd001.ru
домашний интернет омск
интернет провайдер омск
domashij-internet-volgograd002.ru
домашний интернет тарифы
Thanks for your strategies. One thing I’ve noticed is always that banks and also financial institutions really know the spending behavior of consumers as well as understand that plenty of people max out there their own credit cards around the trips. They smartly take advantage of that fact and begin flooding ones inbox plus snail-mail box along with hundreds of Zero APR card offers immediately after the holiday season comes to an end. Knowing that if you are like 98 of American general public, you’ll rush at the chance to consolidate personal credit card debt and transfer balances towards 0 interest rates credit cards.
Awesome https://is.gd/tpjNyL
Lunita Skye Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Tiahnie Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Ms LyLy Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Melanin Cakes – Lexia Will Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
подключить интернет в волгограде в квартире
domashij-internet-volgograd003.ru
домашний интернет тарифы омск
XOXO Melia Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Good https://shorturl.at/2breu
Good https://shorturl.at/2breu
подключить домашний интернет воронеж
domashij-internet-voronezh001.ru
подключить интернет в квартиру воронеж
Very good https://shorturl.at/2breu
подключить интернет в воронеже в квартире
domashij-internet-voronezh002.ru
интернет домашний воронеж
Hɑi Bro! Iam Lakshmi. Тhis iis a rеally insightful and nicely wwritten article!
Ӏ genuinely admire һow clearly you’ѵe laid out thе dіfferent options fοr the Best Glass Door Lock in 2025.
it’s sometimeѕ tricky to find reliable ɑnd aesthetic security solutions,
ƅut уour guide makeѕ thee decision-mɑking pprocess muchh clearer.
Тһе detailed breakdown օf features, pros, ɑnd cons helps readers ⅼike me make an educated decision, еspecially when it comes t᧐ combining security
wiyh aesthetics. I aⅼso appreciated howw уou’ve keⲣt boith hоme and office
needs in mind. Gret job. yߋur worк genuinely adԀs vаlue ɑnd is unique.
Looking forward tⲟ reading moгe posts ⅼike thiѕ inn the future.
Much appreciated!
ElvaSnaps FANSLY Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Gabriella_ Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Juliana x Ferrara Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Thick Lauryn – Thicck Asia Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
домашний интернет подключить воронеж
domashij-internet-voronezh003.ru
подключить интернет в квартиру воронеж
Awesome https://shorturl.at/2breu
Heya i am for the first time here. I found this board and I find It really useful & it helped me out a lot. I hope to give something back and aid others like you helped me.
YogaBlondie Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Paris Senpai Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Very good https://shorturl.at/2breu
Very good https://shorturl.at/2breu
The Official Phat Butt Veda Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
ElvaSnaps FANSLY Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Haleigh Cox Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
NyyJjaae – FANSLY Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
YogaBlondie Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
NamiSwanBB – NamiBBSwan Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Kara J Lee Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Myah Janes VIP Only Fans Leaked Fansly Leaks Mega Folder Download Link ( https://UrbanCrocSpot.org )
Awesome https://lc.cx/xjXBQT
Very good https://lc.cx/xjXBQT
Awesome https://lc.cx/xjXBQT
Excellent post. I used to be checking constantly this weblog and I’m impressed! Very helpful information specially the last phase 🙂 I take care of such information much. I was looking for this certain information for a very lengthy time. Thanks and best of luck.
Awesome https://lc.cx/xjXBQT
Terrific material, Thanks!
Look into my blog post – https://Blogs.Koreaportal.com/bbs/board.php?bo_table=free&wr_id=4054923
In these days of austerity as well as relative anxiety about getting debt, lots of people balk about the idea of making use of a credit card in order to make acquisition of merchandise or even pay for any gift giving occasion, preferring, instead only to rely on a tried and trusted means of making settlement – hard cash. However, in case you have the cash available to make the purchase in full, then, paradoxically, that is the best time just to be able to use the credit card for several causes.
INCREDIBLY PRAGMATIC SHAFTING DOLL WITH METAL SKELETON!
Feel the inequality – ethical like a physical comrade!
ULTRA-SOFT FLAY that perfectly mimics the come near of genuine philanthropist excoriate – indistinguishable!
Anatomically accurate proportions, just like a licit mate – every curve in faultless harmony!
WHY IS THIS DOLL EVERY HOMO SAPIENS’S DREAM?
– STRETCHABLE METAL CONSTRUCT – holds any location you can imagine!
– 100% ALL RIGHT – non-toxic medical-grade material, certified by CCIC – no unnatural smells, lately undefiled pleasure!
– MAXIMUM VERSATILITY – charge out of vaginal, anal, viva voce, tit perform upon and anything else you desire!
– OUTGOING CONTRIBUTION – simple to keep altogether and renewed!
INCOMPATIBLE PROVIDE! Get yours any more at the most suitable figure – while stocks pattern TOP-RATED Bent Doll on AliExpress with BLUSTER REVIEWS!!
BRING SOMEONE ROUND YOUR LUXURIOUS CONFRERE SECOND!
Guarded drab packaging – 100% privacy guaranteed!
This isn’t decent a doll – it’s the fulfillment of your deepest desires! Don’t long for unacceptable – **order age and experience supreme satisfaction!
Good https://lc.cx/xjXBQT
How To Get My Dog Papers
[…]Wonderful story, reckoned we could combine some unrelated information, nonetheless seriously really worth taking a appear, whoa did 1 study about Mid East has got much more problerms as well […]
Dog Papers
[…]usually posts some quite intriguing stuff like this. If you池e new to this site[…]
How To Get My Dog Papers
[…]please go to the internet sites we follow, such as this one, as it represents our picks from the web[…]